 6
Dec,2025
6
Dec,2025
Warfarin Antibiotic INR Risk Calculator
Enter your current INR and antibiotic details to see potential bleeding risk. This tool helps you understand how common antibiotics can affect your warfarin treatment.
INR Risk Assessment
Results based on your inputs
Important Notes
- INR changes take 3-7 days after starting antibiotics
- Monitor INR regularly during antibiotic treatment
- Never adjust warfarin without consulting your doctor
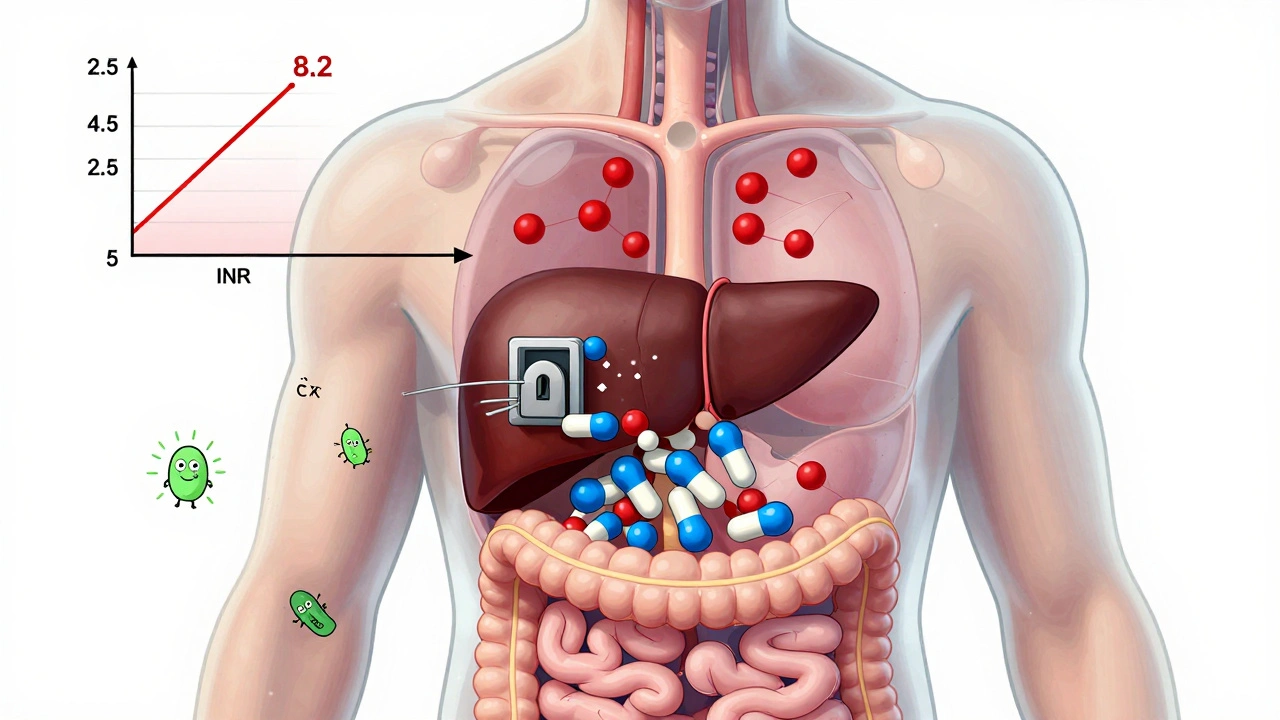
When you’re on warfarin, even a simple antibiotic can throw your blood thinning out of balance - sometimes dangerously so. It’s not just a theoretical risk. Real people, in real clinics, end up in the ER because their INR jumped from 2.5 to 8.2 after taking a common antibiotic for a sinus infection. And it’s not because they missed a dose. It’s because the antibiotic changed how warfarin works in their body.
Why Warfarin Is So Sensitive
Warfarin isn’t like other pills. It has a razor-thin safety margin. Too little, and you’re at risk of a stroke or clot. Too much, and you could bleed internally - in your brain, gut, or joints. The goal is to keep your INR between 2.0 and 3.0. That’s the sweet spot where clot prevention outweighs bleeding risk. But even a small shift - say, from 2.8 to 5.1 - can turn a routine check-up into a hospital trip.
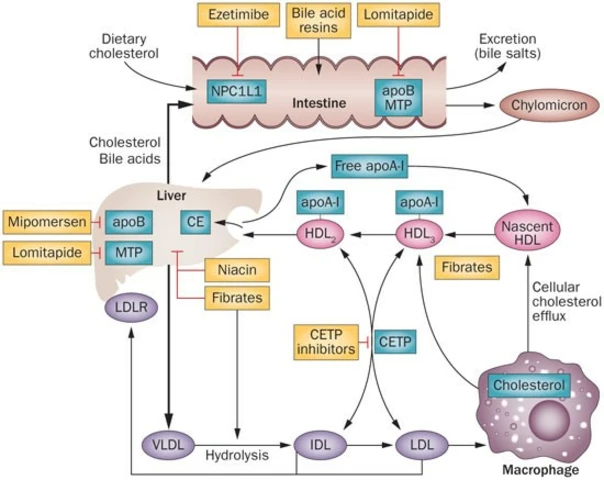
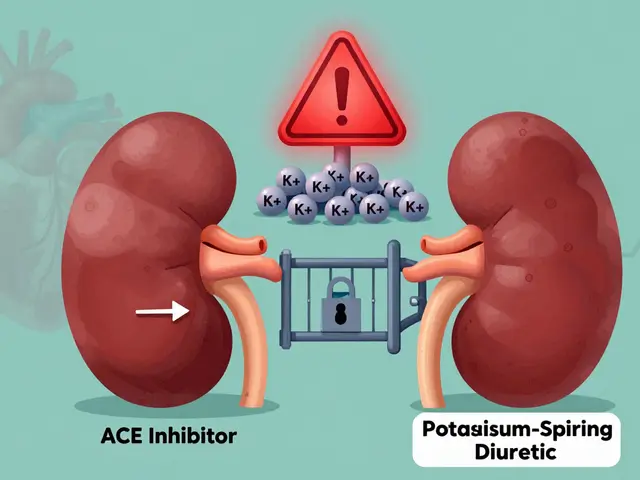
What makes warfarin so unpredictable? Two big reasons: how your liver breaks it down, and what your gut bacteria are doing. Warfarin is processed mainly by the CYP2C9 enzyme. Many antibiotics block this enzyme, meaning warfarin sticks around longer, building up in your blood. At the same time, antibiotics kill off the good bacteria in your gut that naturally produce vitamin K. Since vitamin K counteracts warfarin, less of it means stronger blood thinning. This combo can push your INR up without you even noticing.
Not All Antibiotics Are Created Equal
Some antibiotics are safe. Others? They’re like setting off a landmine under your INR. Here’s what the data shows:
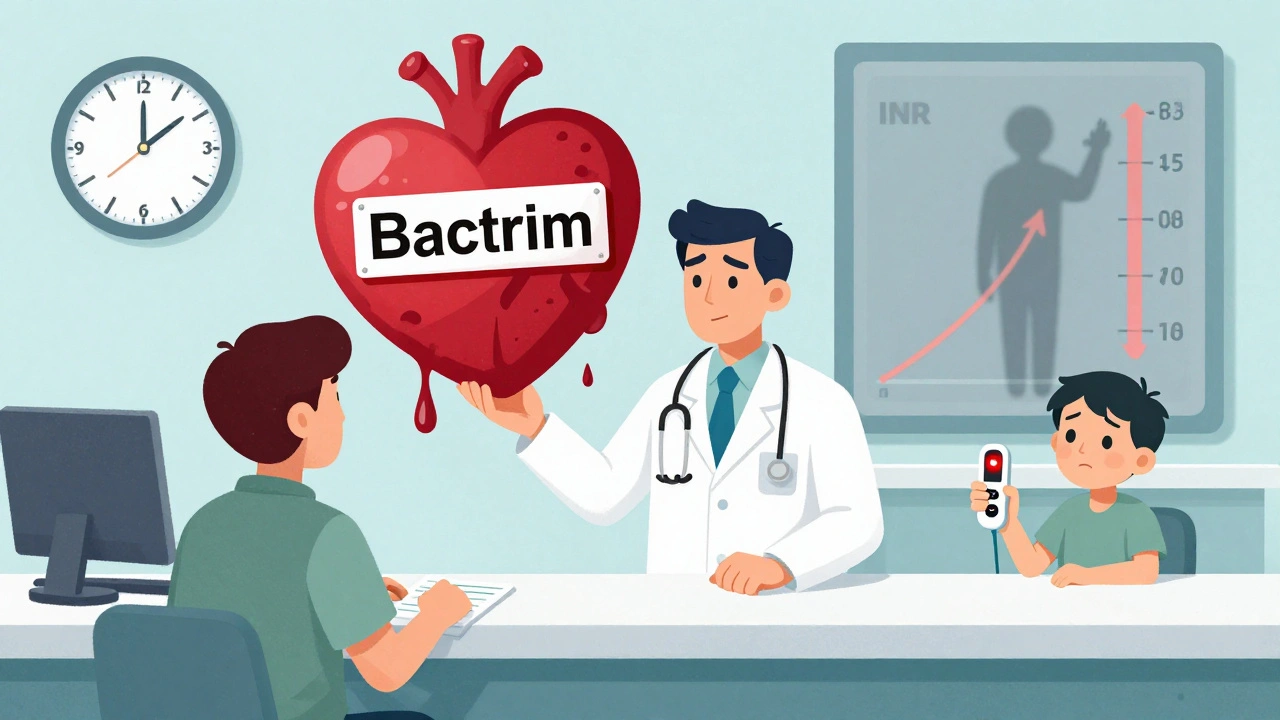
- High-risk antibiotics: Clarithromycin, metronidazole, trimethoprim-sulfamethoxazole (Bactrim), and levofloxacin are the big red flags. These can raise your INR by 1.5 to 3 points within a week. In one study, 34% of patients on clarithromycin saw their INR climb above 5.0.
- Moderate-risk: Ciprofloxacin is tricky. Some studies say it’s fine. Others show it spikes INR in 20-25% of people. Don’t assume it’s safe.
- Low-risk: Amoxicillin, cephalexin, and azithromycin rarely cause problems. Azithromycin, in particular, doesn’t interfere with liver enzymes and leaves gut bacteria mostly alone.
That’s why your doctor shouldn’t just pick any antibiotic for your infection. They need to know you’re on warfarin - and choose wisely. If you’re prescribed Bactrim for a UTI, or metronidazole for a dental abscess, you’re entering high-risk territory.
The Delay That Kills
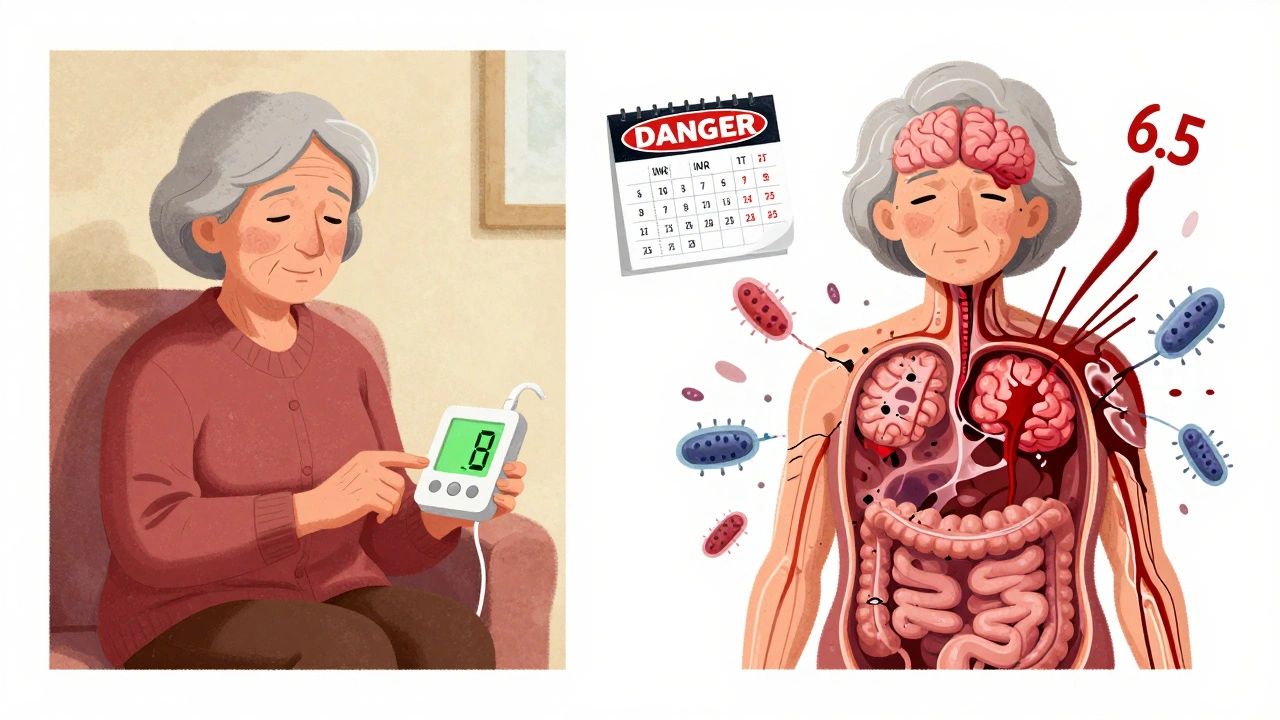
Here’s the part most people don’t get: the danger doesn’t show up right away. It takes 3 to 7 days for your INR to climb after starting an antibiotic. That’s because it takes time for gut bacteria to die off and for vitamin K levels to drop. So if you take your first dose on Monday, you might feel fine on Wednesday - and think everything’s okay. But by Friday, your INR could be climbing fast.
And it gets worse. When you stop the antibiotic, your gut bacteria start bouncing back. Vitamin K production resumes. Suddenly, your blood isn’t thin enough anymore. INR can crash from 3.0 to 1.2 in just 3-4 days. That’s when clots form. There are documented cases of strokes happening days after finishing an antibiotic because the warfarin dose wasn’t adjusted back up.
Who’s Most at Risk?
Not everyone reacts the same way. Some people are walking time bombs. Risk factors include:
- Age over 75
- Cancer diagnosis (your body’s already under stress)
- Baseline INR above 2.5
- Female sex (women tend to have higher INR spikes)
- Low body weight or poor nutrition (less vitamin K stores)
If you fit even one of these, your risk of a dangerous INR spike is nearly double. A 2014 study found that cancer patients on warfarin were almost twice as likely to have an INR above 5.0 after taking an antibiotic. That’s not a small number. That’s a red alert.
What You Need to Do - Step by Step
If you’re on warfarin and need an antibiotic, here’s what you must do - no exceptions:
- Ask your doctor: "Is this antibiotic safe with warfarin?" If they say "probably," push for specifics. Demand to know the risk level.
- Get an INR test before you start: Know your baseline. If it’s already 2.8, you’re already close to the danger zone.
- Test again in 3-5 days: Don’t wait for symptoms. Don’t wait for your next scheduled check. Test early.
- Test again 7-10 days after stopping: This is when INR can drop too low. You might need a higher warfarin dose than before.
- Watch for signs of bleeding: Unexplained bruising, nosebleeds that won’t stop, dark stools, or sudden headaches could mean your INR is too high.
Some patients use home INR monitors now - devices like the Roche CoaguChek INRange. If you have one, use it. Daily monitoring during antibiotic therapy isn’t overkill. It’s life-saving.
What Happens When It Goes Wrong
In 2022, the FDA recorded over 1,800 cases of warfarin-antibiotic interactions. Nearly 20% involved major bleeding - bleeding that required hospitalization, blood transfusions, or surgery. A 2021 study found that nearly a quarter of all warfarin-related ER visits happened because someone took an antibiotic without proper monitoring.
One Reddit thread from r/Anticoagulation had 37 stories of people whose INR shot to 6.5 or higher after clarithromycin. One woman needed vitamin K injections. Another had a brain bleed. In another thread, 15 people reported INR crashes after stopping ciprofloxacin. Two had strokes.
These aren’t rare. They’re predictable. And they’re preventable.
The Bigger Picture
Warfarin is still used by over 3 million Americans. Why? It’s cheap - about $4 a month. Newer blood thinners like apixaban cost over $500. For Medicare patients, warfarin is often the only option. But cost shouldn’t come at the price of safety.
Doctors are still getting it wrong. Only 33% of primary care providers consistently order INR checks after starting antibiotics, according to a 2020 study. That’s not negligence - it’s ignorance. Many still think "all antibiotics are the same." They’re not.
There’s new tech helping. Pharmacogenetic testing can now predict how you’ll metabolize warfarin based on your DNA. AI tools like WAR-DRUG can forecast your INR response to specific antibiotics with nearly 90% accuracy. But none of that matters if you don’t get tested.
Bottom Line
If you’re on warfarin, antibiotics aren’t just another pill. They’re a potential trigger for serious harm. The risk isn’t hypothetical. It’s documented, measured, and deadly. The solution isn’t avoiding antibiotics - it’s managing the interaction. Know which ones are dangerous. Get tested before, during, and after. Talk to your pharmacist. Ask your doctor to document the antibiotic’s risk level in your chart.
Your INR isn’t just a number. It’s your life’s balance. And antibiotics can tip it - quietly, suddenly, and without warning. Don’t wait for a bleed to realize you should’ve checked it sooner.



This is the kind of post that makes you realize how little we’re taught about our own medications. I was on warfarin for AFib and got prescribed cipro for a UTI - no one warned me. Three days later I was bruising like a toddler who fell down the stairs. Got my INR checked - 6.8. They gave me vitamin K and told me to "be more careful." No follow-up. No explanation. I’m alive because I noticed the bruising. Don’t wait for a bleed.
There is no excuse for physicians to prescribe high-risk antibiotics to patients on warfarin without first consulting a pharmacist or ordering an immediate INR test. The data is clear, the guidelines are published, and the consequences are documented. This is not a gray area. It is a systemic failure in primary care that results in preventable hemorrhages, strokes, and deaths. If your doctor doesn’t know this, they shouldn’t be prescribing anticoagulants.
Wow. So antibiotics are bad. Who knew? Next you’ll tell me water is wet.
Listen - if you’re on warfarin, you need to treat every antibiotic like a grenade. Don’t assume it’s safe. Don’t trust the label. Don’t wait for symptoms. Test before, test after, test again. I’ve been on warfarin for 12 years. I have a home monitor. I check every other day when I’m on antibiotics. It’s not a hassle - it’s the difference between walking out of the hospital and being wheeled in. Your life is worth the extra 5 minutes.
Big Pharma doesn’t want you to know this. They make billions off warfarin and new anticoagulants. They bury the data. The FDA? A puppet. They let Bactrim stay on the market even though it’s a silent killer for 3 million people. And the doctors? They’re trained by the same pharma reps who give them free lunches. Wake up. This isn’t medicine - it’s a profit-driven slaughterhouse with white coats.
As someone from India where warfarin is the only affordable option for millions, this is terrifying. We don’t have home INR monitors. We don’t have easy access to pharmacists. Most doctors just prescribe amoxicillin and move on. This post should be translated and shared in every rural clinic. People are dying because no one told them.
What’s interesting is how this reflects the fragility of biological systems. Warfarin’s mechanism is elegant - it blocks vitamin K recycling. But the gut microbiome? That’s an entire ecosystem. Antibiotics don’t just kill pathogens; they collapse the metabolic architecture that maintains homeostasis. We treat drugs like isolated variables, but biology is a network. A change in one node - gut flora - ripples through coagulation, inflammation, even mood. We’re not just dosing pills. We’re hacking a living system.
They say warfarin is outdated. But here’s the truth - it’s not the drug that’s dangerous. It’s the system that treats it like a commodity. We don’t monitor. We don’t educate. We don’t train. We just hand out scripts and hope for the best. And then we act shocked when someone bleeds out. This isn’t about science. It’s about arrogance. We think we control biology, but we’re just stumbling through it with a clipboard and a calculator.
so like… dont take antibiotics if ur on warfarin? duh.
I’m a nurse and I’ve seen this too many times. One lady came in with a GI bleed after taking Bactrim for a UTI. She was 78, had cancer, and her INR was 9.4. She didn’t know she needed to check it. No one told her. We need to make sure every patient on warfarin gets a printed card - like a wallet card - that says "DANGEROUS ANTIBIOTICS" and "TEST IN 3 DAYS." Simple. Free. Life-saving.
Thank you for this. I’ve been on warfarin since my pulmonary embolism. I use a home monitor now. I check every day when I’m on antibiotics. I also tell my pharmacist every time I get a new script - even if it’s for a cough. They’ve started keeping a flag on my file. It feels weird to be so paranoid… but I’d rather be annoying than dead. 💙
The real tragedy isn’t the interaction - it’s that we’ve normalized this risk. We accept that patients on warfarin are collateral damage in the antibiotic economy. We don’t redesign prescribing protocols. We don’t mandate pharmacist consults. We don’t fund public education. We just hope people read the pamphlet. That’s not healthcare. That’s gambling with lives and calling it medicine.