 12
Oct,2025
12
Oct,2025
Fertility Environment Risk Calculator
How Your Environment Affects Fertility
This tool evaluates how environmental factors mentioned in the article may impact your ovulation cycle. Rate your current exposure levels.
Quick Summary / Key Takeaways
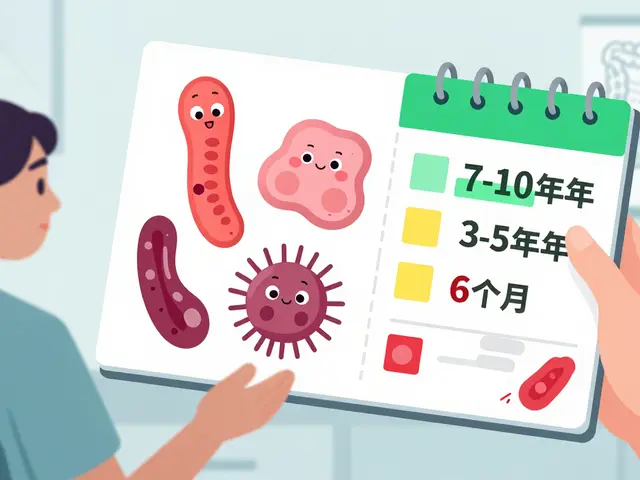
- Both natural and man‑made environmental factors can shift hormone levels that drive ovulation.
- Endocrine‑disrupting chemicals (EDCs) like BPA and phthalates are linked to irregular cycles and lower egg quality.
- Extreme temperatures, high stress, and poor air quality can shorten the fertile window.
- Simple lifestyle tweaks-improving indoor air, managing stress, and watching temperature exposure-can protect ovulation.
- Regular tracking and a short‑term checklist help you spot patterns before they impact pregnancy plans.
What Ovulation and Fertility Really Mean
When you hear the word Ovulation is the release of a mature egg from the ovary, typically occurring once each menstrual cycle, think of it as the body’s monthly invitation for pregnancy. If the egg meets sperm within roughly 24 hours, fertilization can happen, and the uterine lining prepares for implantation.
Fertility is the ability to conceive and carry a pregnancy to term. It’s not just a single event; it’s a complex interplay of hormone signaling, egg health, uterine environment, and timing. Anything that disturbs the hormone cascade-whether a sudden temperature spike or a chemical from a plastic bottle-can reduce the odds of successful conception.
Key Environmental Players That Touch Hormones
Our bodies live inside a constantly shifting environment. Below are the biggest external forces that have scientific backing for messing with the hormone systems that control ovulation.
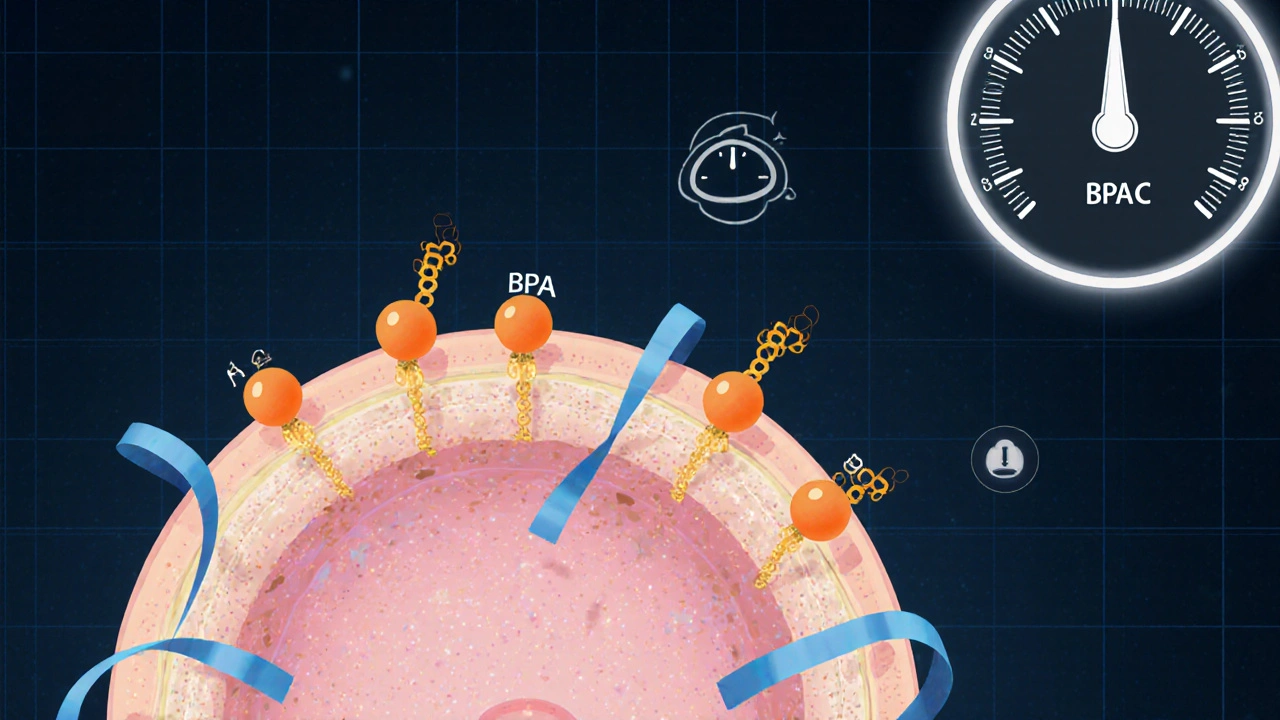
- Endocrine‑Disrupting Chemicals are synthetic compounds that mimic or block natural hormones, especially estrogen and progesterone. Common culprits are BPA (found in polycarbonate plastics), phthalates (in fragrances), and certain pesticides.
- Temperature & Seasonal Change refer to external heat or cold exposure that can alter core body temperature and affect the hypothalamic‑pituitary‑ovarian axis. Women living in very hot climates often see shorter luteal phases.
- Stress is the body’s psychological and physiological response to perceived threats, releasing cortisol that interferes with reproductive hormones. Chronic work pressure, anxiety, or major life events are typical sources.
- Air Pollution includes fine particulate matter (PM2.5), nitrogen dioxide, and ozone that trigger systemic inflammation and oxidative stress. Studies in urban centers link high PM2.5 levels to delayed ovulation.
- Nutrition and Body Mass Index (BMI) act as a bridge between environment and hormones. Poor diet, excessive caffeine, or low body fat can blunt estrogen production, while obesity raises insulin and androgen levels.
How Each Factor Disrupts the Ovulation Cycle
Let’s walk through the biological chain reaction for each major factor.
- Endocrine‑Disrupting Chemicals: EDCs bind to estrogen receptors in the brain and ovaries, sending mixed signals that can either advance or delay the luteinizing hormone (LH) surge. A 2023 cohort of 2,400 women showed a 12% drop in monthly ovulation probability when urinary BPA levels rose above the 75th percentile.
- Temperature & Seasonal Change: When core temperature rises above 37.2°C, the hypothalamus reduces gonadotropin‑releasing hormone (GnRH) pulses, which in turn lowers LH and follicle‑stimulating hormone (FSH). Women working in hot factories report up to 3‑day delays in ovulation during summer months.
- Stress: Chronic cortisol spikes blunt GnRH release and can cause anovulatory cycles. A longitudinal study of 1,800 nurses found that high perceived stress correlated with a 22% increase in missed ovulations over a year.
- Air Pollution: Fine particles penetrate lung tissue, prompting systemic inflammation and oxidative damage to ovarian follicles. In a European panel, women exposed to PM2.5 >35µg/m³ had a 17% longer follicular phase.
- Nutrition & BMI: Low body fat (<18%) reduces leptin, a hormone that signals energy sufficiency to the brain; insufficient leptin stalls the LH surge. Conversely, high BMI raises insulin, which can increase androgen production and disrupt follicle maturation.
Practical Steps to Shield Ovulation from Harmful Influences
You don’t need a chemistry degree to make smarter choices. Below are evidence‑backed actions you can start today.
- Swap Plastic for Glass or Stainless Steel: Use BPA‑free containers for food storage; avoid microwaving plastic.
- Regulate Indoor Temperature: Keep bedroom temperature between 18-22°C. If you work in a hot environment, schedule a cool‑down break after 2hours of exposure.
- Stress‑Management Toolbox: Try 10minutes of diaphragmatic breathing, progressive muscle relaxation, or a short walk during lunch. Consistency beats intensity.
- Improve Air Quality: Run HEPA filters, keep windows closed during rush‑hour traffic, and plant air‑purifying indoor species (e.g., snake plant).
- Balanced Nutrition: Aim for 45-55% carbs, 20-30% protein, and 25-35% healthy fats. Include omega‑3 rich foods (salmon, walnuts) to counteract inflammation from pollutants.
- Track Your Cycle: Use a fertility app or basal body temperature chart to spot irregularities early. If you notice a pattern of delayed ovulation, bring it up with a healthcare provider.
Checklist: Weekly Self‑Audit for Reproductive Health
Give yourself a quick scan every Sunday. Tick off items that apply; missing pieces may point to a hidden environmental stressor.
| Area | Question | Yes/No |
|---|---|---|
| Plastic Exposure | Did I use BPA‑free containers for meals and drinks? | |
| Temperature Control | Was my sleeping environment kept below 22°C? | |
| Stress Levels | Did I practice a stress‑relief technique for at least 10minutes? | |
| Air Quality | Is the indoor air filtered or ventilated at least twice daily? | |
| Nutrition | Did I eat at least three servings of fruit/veg and omega‑3 foods? | |
| Cycle Tracking | Did I log basal temperature or ovulation symptoms? |

Comparison of Environmental Factors and Their Typical Impact on Ovulation
| Factor | Typical Effect | Evidence Strength (1‑5) |
|---|---|---|
| Endocrine‑Disrupting Chemicals | Irregular cycles, reduced egg quality | 5 |
| Extreme Temperature | Delayed LH surge, shorter fertile window | 3 |
| Chronic Stress | Missed ovulation, lower progesterone | 4 |
| Air Pollution (PM2.5) | Lengthened follicular phase, oxidative damage | 3 |
| Poor Nutrition/High BMI | Hormonal imbalance, anovulatory cycles | 4 |
When to Seek Professional Help
If you notice any of the following, schedule a visit with a reproductive endocrinologist or a knowledgeable OB‑GYN:
- Three consecutive months without ovulation (confirmed by tracking).
- Sudden weight change (>10% body weight) with cycle disruption.
- Persistent high stress that interferes with sleep or appetite.
- Living in a high‑pollution area and experiencing irregular periods.
Doctors can run hormone panels, ultrasound monitoring, and, if needed, recommend interventions such as medication, counseling, or environmental remediation strategies.
Frequently Asked Questions
Can occasional exposure to BPA really affect my chances of getting pregnant?
Yes. Even short‑term spikes in BPA can transiently mimic estrogen, which may shift the timing of the LH surge. A study of 500 couples found a 7% reduction in conception rates when women reported using polycarbonate water bottles daily for just one month.
Is it safe to exercise outdoors in hot weather while trying to conceive?
Light to moderate activity is fine, but avoid prolonged exposure above 30°C. If you must train in heat, hydrate well, wear breathable fabrics, and cool down indoors soon after to keep core temperature stable.
Do air purifiers actually improve fertility outcomes?
Research from 2022 indicates that using HEPA filters lowered indoor PM2.5 by 40% and was associated with a modest 5% increase in regular ovulation among women living in polluted cities.
How much stress is too much for my reproductive health?
Chronic stress that elevates cortisol above normal waking levels for more than three weeks is problematic. Tools like the Perceived Stress Scale can help you gauge whether you’re in the risky zone.
Should I get my hormone levels checked if I’m trying to conceive?
A baseline panel (FSH, LH, estradiol, progesterone, and thyroid hormones) is a good starting point, especially if you’re exposed to high‑risk environmental factors. Results guide personalized lifestyle or medical interventions.
Understanding how the world around you nudges the delicate hormone orchestra gives you a real advantage. By spotting the biggest culprits-chemical exposures, temperature swings, stress bursts, and polluted air-you can take targeted steps that keep ovulation on schedule and boost your fertility chances.
Remember, the body is resilient, but it also signals when something’s off. Use the checklist, trust your cycle data, and don’t hesitate to seek professional input when patterns persist. Your reproductive journey is a partnership between biology and environment-make the environment work for you.





I think it’s pretty eye‑opening how something as simple as a plastic water bottle can tweak hormone signals and mess with ovulation cycles we just go about our day using these items without a second thought and it really shows how our environment is subtly influencing fertility outcomes we don’t even notice
From a clinical perspective it is valuable to recognize that endocrine‑disrupting chemicals, temperature fluctuations, chronic stress, and air quality are all modifiable risk factors; adopting proactive measures such as reducing plastic use, ensuring adequate hydration, and incorporating stress‑reduction techniques can meaningfully improve ovulatory health.
When you look at the hypothalamic‑pituitary‑ovarian axis the feedback loops are highly sensitive to exogenous endocrine disruptors; BPA binds to estrogen receptors and can alter the LH surge timing which in turn affects follicular development – think of it like a noisy signal interfering with a well‑tuned circuit, so minimizing exposure is a pragmatic strategy.
It’s encouraging to see that simple lifestyle tweaks such as using HEPA filters, staying cool during workouts, and practicing mindfulness can collectively shift the risk profile toward a healthier ovulatory environment :)
While the enthusiasm is noted one might contend that the emphasis on personal responsibility overlooks systemic issues such as regulatory failures and socioeconomic disparities that limit access to low‑exposure environments.
Consider, if you will, the intricate ballet of endocrine signaling wherein each hormone acts as a dancer perfectly timed to the music of the hypothalamus the moment a synthetic compound such as phthalate steps onto the stage the choreography is disrupted the audience-our bodies-perceive discord that can delay the luteinizing hormone surge the rhythm of ovulation is thus thrown off beat studies have shown that women with elevated urinary BPA experience a measurable shift in cycle length this is not merely anecdotal but a quantifiable perturbation of the reproductive axis the temperature factor, often dismissed as trivial, plays a role by influencing core body temperature and thereby modulating GnRH pulse frequency; sustained exposure to high ambient heat can blunt this pulse leading to a downstream reduction in LH and FSH output stress, another invisible hand, elevates cortisol which antagonizes gonadotropin release creating an anovulatory environment chronic exposure to fine particulate matter incites systemic inflammation that translates into oxidative stress within ovarian follicles shortening their viability the cumulative effect of these variables is a mosaic of risk that can be mapped and, importantly, mitigated with informed choices the calculator presented offers a practical interface for individuals to quantify their exposure and prioritize interventions thereby translating abstract science into actionable steps
This comprehensive overview really drives home that we have agency-by swapping plastic containers for glass, cool‑down after workouts, using air purifiers, and finding moments to breathe deeply we can rewrite the script of our fertility journey; the science backs it and the calculator makes the path clear, so let’s seize it and turn those risk numbers into success stories.
One might jest that an app could replace a specialist, yet the calculator merely serves as a preliminary screening tool, not a definitive diagnostic.
The methodology appears overly simplistic given the multifactorial nature of reproductive endocrinology.
It’s great that the tool is user‑friendly; pairing it with regular cycle tracking and occasional check‑ups can really help you stay on top of things while keeping the stress low.