 19
Jan,2026
19
Jan,2026
When you pick up a prescription at your local pharmacy in the UK, you might not realize that the medicine you’re handed isn’t always the one your doctor originally wrote. That’s because pharmaceutical substitution is now standard practice under NHS rules. Since 2013, pharmacists have been allowed to swap branded drugs for cheaper generic versions - unless your doctor specifically wrote "dispense as written" on the prescription. But in 2025, everything changed. New laws didn’t just tweak the rules; they overhauled how medicines and care are delivered across the entire NHS.
What Changed in the 2025 NHS Substitution Rules?
The Human Medicines (Amendment) Regulations 2025, which took full effect on October 1, 2025, turned the UK’s pharmacy system upside down. The biggest shift? All NHS pharmaceutical services must now be delivered remotely by Digital Service Providers (DSPs). That means no more face-to-face consultations at the counter. Instead, prescriptions are processed digitally, and medications are sent to patients by post or collected from automated kiosks. This wasn’t a slow transition - it was a hard cutoff. Pharmacies that were already on the pharmaceutical list had to adapt under old rules, but any new provider applying after June 23, 2025, had to meet stricter market entry requirements.
This change was meant to cut costs and increase efficiency. The government estimated that shifting 90% of eligible prescriptions to generic drugs - up from the current 83% - could save over £400 million annually. But the real cost isn’t just financial. It’s human. Community pharmacies reported needing between £75,000 and £120,000 each to upgrade to the new digital systems. Many small, independent pharmacies say they can’t afford it. And with 54% of them expressing serious concerns about safety and sustainability, the risk of service gaps is real.
From Hospital Beds to Living Rooms: Service Substitution in Action
Pharmaceutical substitution is only half the story. The NHS is also pushing hard to replace hospital-based care with community and digital alternatives. The 2025 mandate to NHS England was clear: move care "from hospital to community, sickness to prevention, and analogue to digital." That means fewer emergency visits, fewer outpatient appointments, and more care happening at home.
One of the biggest targets? People over 65. The goal is to cut emergency hospital admissions for this group by 15% by 2026-27. How? By replacing hospital follow-ups with community nurses, virtual clinics, and home-based monitoring. For example, virtual fracture clinics in Manchester reduced unnecessary appointments by 40%. But for elderly patients without smartphones or internet access, that same change created new barriers. One patient in Bolton told the NHS Staff Survey: "I couldn’t join the video call. My grandson helped, but he works long hours. I ended up waiting three weeks for a paper letter. By then, my pain got worse."
Integrated Care Boards (ICBs) are now legally required to design local plans that help people stay independent. That sounds good - until you realize many rural areas lack the infrastructure. The NHS Confederation found that 42% of trusts in remote regions don’t have enough community health workers, transport options, or digital tools to make this work. In places like Cumbria or North Yorkshire, the gap between policy and reality is wide.
Who’s Getting Left Behind?
Not everyone benefits equally from these changes. The King’s Fund warned that without fixing the 28,000-person workforce shortage in community care, substitution could widen health inequalities by 12-18% in the most deprived areas. In Greater Manchester, early attempts to shift care to community hubs actually made things worse before they got better. Vulnerable patients - those with dementia, mental health conditions, or limited English - were missed because the new system assumed everyone could navigate apps, book online appointments, or understand digital instructions.
Dr. Sarah Wollaston, former chair of the Health and Social Care Committee, pointed to a 12% spike in medication errors in North West London’s remote dispensing pilot. Many of those errors came from miscommunication between digital systems and patients who couldn’t verify their prescriptions. One case involved an 81-year-old woman who received two different blood pressure pills because her digital record mixed up two similar-sounding names. She didn’t notice until she collapsed at home.
Meanwhile, tax credit changes as of April 5, 2025, removed exemptions for NHS travel and medication costs for some low-income patients. That means even if a generic drug is cheaper, the cost of getting to a pharmacy or paying for delivery might now be too high for those on tight budgets.

How Pharmacists Are Coping
Pharmacists are on the front lines. They’re no longer just dispensing pills - they’re now tech support, patient advocates, and remote care coordinators. Many say they’re being asked to do more with less. The British Pharmaceutical Industry survey showed that 78% of hospital pharmacists are worried about medication safety under the new remote model. Why? Because they’ve lost direct contact with patients. No more asking, "Did you take your pill today?" No more noticing a tremor or confusion during a quick chat at the counter.
Some pharmacies are adapting. In Bristol, a pharmacy chain installed AI-powered voice assistants in their kiosks to help older patients confirm their prescriptions. In Leeds, pharmacists now do weekly phone check-ins with high-risk patients. But these are exceptions. Most pharmacies don’t have the budget for tech upgrades, let alone staff training.
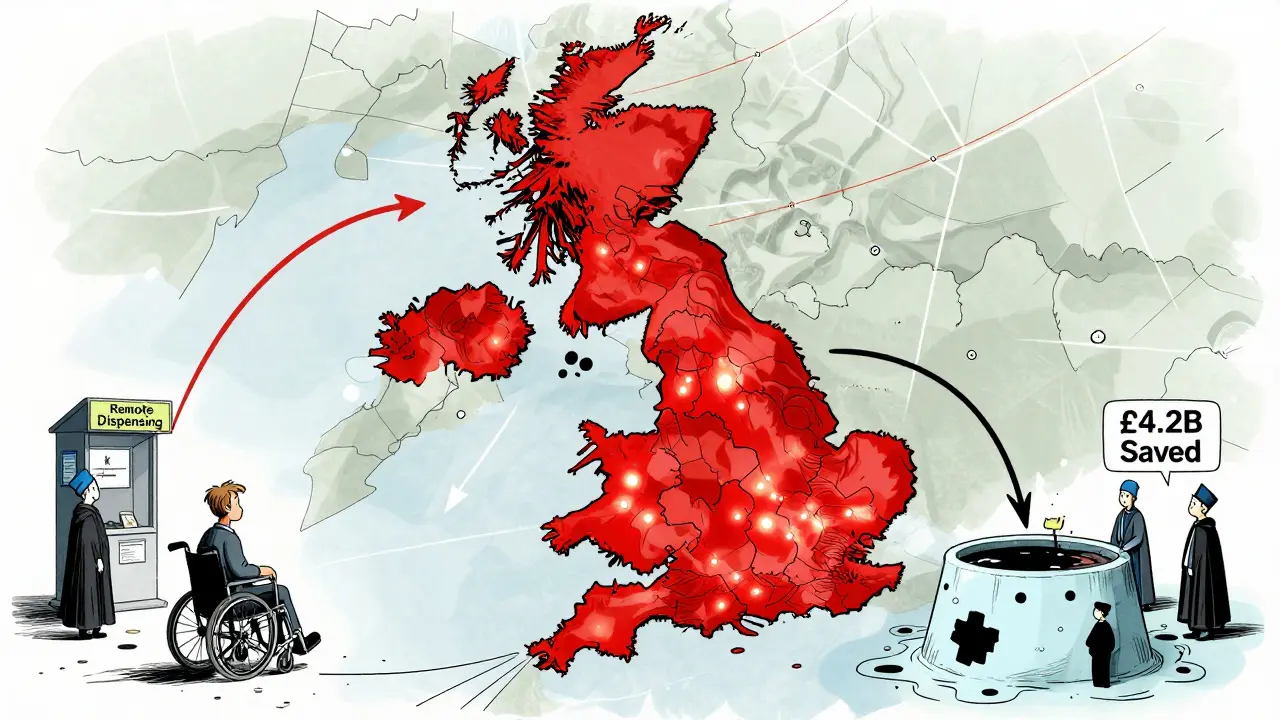
What’s Next? The 2030 Vision
The NHS 10-Year Health Plan lays out a bold goal: by 2030, 45% of current outpatient appointments will be replaced with community or virtual care. That’s over 1.2 million fewer hospital visits per year - if it works. The Department of Health estimates this could save £4.2 billion annually. But the Nuffield Trust cautions that if workforce gaps and digital exclusion aren’t fixed, the system could end up spending 7-10% more due to avoidable errors, readmissions, and fragmented care.
Looking ahead, the Carr-Hill formula - set to launch in April 2026 - will try to fix this by directing more funding to areas with the greatest need. But that’s still a year away. In the meantime, NHS trusts are under pressure to cut deficits. The withdrawal of deficit support funding starting in 2026-27 means hospitals will be forced to push even more care into the community - whether the systems are ready or not.
What This Means for You
If you’re on long-term medication, expect your prescription to be switched to a generic version unless your doctor says otherwise. You won’t always be told. That’s legal under current rules. But if you’re elderly, have mobility issues, or struggle with technology, you might find it harder to get your meds. Ask your pharmacist: "Is this a substitution? Can I still pick it up in person?"
If you’re a caregiver, keep track of medication changes. Write down names, dosages, and what’s been switched. If you notice side effects or confusion, contact your GP immediately. Don’t assume the new system is flawless.
And if you’re a patient who’s been pushed into a virtual appointment you can’t join - speak up. There are still legal rights to reasonable adjustments under the Equality Act 2010. The NHS is changing fast. But you still have a voice.
Can my pharmacist legally swap my branded medicine for a generic one without telling me?
Yes, under NHS rules, pharmacists can substitute a branded drug with a generic version unless your doctor has marked the prescription with "dispense as written" (DAW). They are not legally required to notify you beforehand, but many pharmacies do so as a courtesy. You have the right to ask for the original brand if you prefer - though you may need to pay the difference in cost.
Are remote dispensing services safe?
Safety concerns are real. A pilot in North West London saw a 12% increase in medication errors after switching to remote dispensing. Issues included digital miscommunication, patients not understanding instructions, and lack of face-to-face checks. While the system reduces wait times and cuts costs, it’s not yet foolproof - especially for older adults, people with cognitive impairments, or those without reliable internet access.
What if I can’t use digital services for my NHS care?
You have a legal right to reasonable adjustments under the Equality Act 2010. If you can’t use apps, video calls, or online booking systems, your GP or ICB must offer alternatives - like phone appointments, paper forms, or in-person visits. Don’t accept being forced into a digital system you can’t use. Ask for help from your local Patient Advice and Liaison Service (PALS).
Why is the NHS pushing so hard for generic drugs and remote care?
The NHS is under massive financial pressure. Generic drugs cost up to 80% less than branded ones. Moving care to community settings reduces expensive hospital overheads. The government estimates these changes could save £4.2 billion by 2030. But the goal isn’t just cost-cutting - it’s also about preventing illness before it leads to hospitalization. The real challenge is doing this without leaving vulnerable people behind.
Will I still be able to get my prescription from my local pharmacy?
It depends. Pharmacies that can afford the £75,000-£120,000 tech upgrades and meet new digital requirements will stay open. Many smaller, independent pharmacies may close or merge. If your local pharmacy becomes a Digital Service Provider, you’ll likely get your meds by post or from a kiosk - not the counter. Check with your pharmacy directly about their plans.
Final Thoughts
The UK’s shift toward substitution - in both medicine and care delivery - is one of the biggest changes to the NHS in decades. It’s driven by money, efficiency, and a vision of prevention over crisis. But technology can’t replace human judgment. A pill is only as good as the person who takes it - and the system that supports them.
If you’re healthy and tech-savvy, these changes might make your life easier. But if you’re older, disabled, or living in a rural area, you might find yourself caught in the gap between policy and practice. The NHS promises better care. But better care isn’t just cheaper. It’s safer, kinder, and more accessible. That’s the real test - and right now, it’s still being written.






The NHS is just outsourcing its failures to algorithms and kiosks. They think replacing human interaction with a voice assistant is innovation? It’s negligence wrapped in a PowerPoint slide. People aren’t data points. They’re grandparents who can’t read tiny screens and don’t trust robots with their pills.
It is regrettable that the implementation of the 2025 regulations has proceeded with insufficient regard for the sociological ramifications upon the elderly and economically disadvantaged. The structural integrity of primary care delivery has been compromised in the name of fiscal austerity, and the resultant fragmentation of patient-provider rapport is not merely a logistical concern-it is an ethical failure of the first order.
I’ve been a pharmacist for 22 years, and I’ve seen a lot. But this? This is the first time I’ve felt like I’m being asked to be a tech support rep, a mental health counselor, and a pharmacist all at once-with no training, no budget, and no backup. The worst part? We’re being blamed when patients get confused or miss doses. We didn’t design this system. We’re just the ones stuck cleaning up the mess.
One lady came in last week because her blood pressure med was swapped. She didn’t know the new one had a different name. She thought it was a scam. She called the cops. We had to explain it three times. No one asked us if we had the time or resources to do this.
And now they want us to do weekly phone check-ins? On top of 60 prescriptions a day? You can’t scale compassion with a spreadsheet.
THIS IS THE NEW WORLD ORDER!!! 🤖💊 They’re replacing doctors with robots so they can track your meds and your movements. Next thing you know, the government will be deciding which pills you’re allowed to take based on your credit score. You think this is about saving money? No. It’s about control. They want you dependent on the system so you can’t question anything. The NHS isn’t broken-it’s been hijacked. Wake up, sheeple!
Remember when they said 5G was a weapon? Now look. Same playbook. They’re testing this on the elderly first. They know you won’t fight back. But I’m not letting them take my freedom. I’m switching to herbal remedies and raw milk. #NHSIsTheNewSocialCredit
So… they’re switching meds, removing cashiers, and making people use apps… and nobody’s surprised? I mean, it’s just… what’s next? AI prescribing? Drone-delivered insulin? It’s not even shocking anymore. It’s just… the new normal. Like when your phone updates and suddenly the home button is gone. You just… adapt. Or don’t. And then you get left behind.
One must interrogate the epistemological foundations of the substitution paradigm. If efficacy is measured solely by cost-per-unit and not by patient-reported outcomes, then the entire enterprise is predicated upon a fallacy: that health can be commodified without consequence. The data presented, while statistically compelling, lacks qualitative nuance. One cannot optimize human suffering into a line item.
I just want to say thank you to all the pharmacists and community nurses trying to hold this together. 🙏 I know it’s not perfect, but I’ve seen how hard they work. My mom got her meds delivered last week-she couldn’t leave the house-and the nurse called to check in. She cried because someone remembered her name. That matters. Even if the system’s broken, people still show up.
Think about it. Why now? Why the sudden push for remote care? The EU was leaking data on NHS patient records in 2024. The AI systems they’re rolling out? Built by private contractors with ties to defense firms. They’re not just saving money-they’re building a biometric surveillance network under the guise of healthcare efficiency. Your blood pressure readings, your medication history, your mobility patterns-all feeding into a predictive model that could one day flag you as ‘high-risk’ and deny you care before you even ask for it.
They call it ‘substitution.’ I call it a Trojan horse. And the people who cheer this on? They’re the ones who’ll be the first to disappear when the algorithm decides they’re no longer ‘productive.’
They’re not replacing pills. They’re replacing your autonomy. And you’re handing it over because it’s ‘convenient.’
Hey everyone-I’m a caregiver for my dad with dementia. This whole system is terrifying, but I’m not giving up. I called my ICB and asked for a paper prescription option. They sent me a form. I filled it out. They approved it. It took two weeks, but I got it. You have rights. Don’t let them tell you it’s impossible. Just keep asking. Keep pushing. You’re not alone.
Wow. So the NHS is just… giving up? Like, what’s next? No more doctors? Just a chatbot that says ‘take two pills and text your symptoms’? I mean, I get saving money, but this feels like the UK version of ‘let them eat cake’ but with less cake and more confusion.
This isn’t innovation. It’s abandonment. They’ve turned healthcare into a logistics problem instead of a moral one. And now they’re pretending the people who suffer most are just ‘edge cases.’ They’re not edge cases. They’re our parents. Our neighbors. Our future.
There’s a quiet tragedy here that no one talks about: the loss of the pharmacy counter as a social space. For so many elderly people, especially widows and widowers, that weekly visit was the only human interaction they had. Now it’s replaced by a kiosk that asks, ‘Are you sure you want this medication?’ in a robotic voice. No smile. No ‘How’s your grandson?’ No ‘You look tired today.’ That’s not efficiency. That’s loneliness packaged as progress.