 3
Dec,2025
3
Dec,2025
When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. And for the most part, it does. But how does the FDA make sure it keeps working safely - especially after millions of people start taking it? The answer isn’t just in the lab. It’s in the real world.
Approval Isn’t the End - It’s Just the Start
Generic drugs don’t need to repeat the same long clinical trials as brand-name drugs. Thanks to the 1984 Hatch-Waxman Act, manufacturers only need to prove their product is bioequivalent to the original. That means the active ingredient is the same, and it gets absorbed into the body at the same rate and amount. Simple, right? But here’s the catch: bioequivalence doesn’t catch everything. A pill might have the same chemistry but a different filler, coating, or release mechanism. These small differences can matter - especially for complex drugs like extended-release painkillers, inhalers, or topical creams. That’s why the FDA doesn’t stop watching after approval. In fact, most of what they learn about safety happens after the drug hits the shelves.How the FDA Tracks Problems After Approval
The FDA doesn’t wait for complaints. They’re actively listening - and looking - through several systems:- FAERS (FDA Adverse Event Reporting System): This is the main hub for reports. Doctors, pharmacists, patients, and even drug companies can submit reports about side effects, allergic reactions, or unexpected outcomes. In 2023 alone, FAERS received over 1.2 million reports for all drugs - including generics.
- MedWatch: This is the public-facing portal where anyone can report a problem. If you notice your generic blood pressure pill makes you dizzy when the brand didn’t, you can file a report here. These reports help the FDA spot patterns.
- Sentinel Initiative: This isn’t just passive reporting. Sentinel uses real-time data from health insurers and electronic medical records covering over 200 million Americans. It can detect if a certain generic is linked to a spike in hospital visits or heart issues - even before anyone files a report.
- Unannounced factory inspections: The FDA shows up at manufacturing sites without warning. They check if the pills being made today match what was approved years ago. A change in the supplier of an inactive ingredient? That’s a red flag.
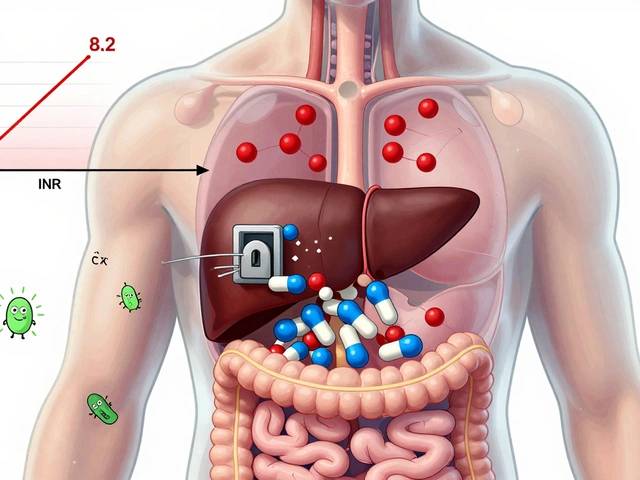
Complex Generics Are the Biggest Challenge
Not all generics are created equal. Simple tablets - like metformin or lisinopril - are easy to copy. But what about an inhaler that delivers medicine deep into the lungs? Or a topical cream that needs to penetrate skin at a precise rate? These are called complex generics. Bioequivalence studies can’t always predict how they’ll behave in real patients. That’s why the FDA has launched special programs to monitor them. In 2020, the agency partnered with the Universities of Maryland and Michigan to create the Center for Research on Complex Generics (CRCG). Their job? To figure out how formulation differences - like particle size or viscosity - might affect safety. In 2023, the FDA allocated $5.2 million to develop AI tools that can analyze real-world data and spot potential problems faster.
It’s Not Always the Drug - Sometimes It’s the Mind
Here’s something surprising: a lot of complaints about generics aren’t about chemistry. They’re about perception. A 2019 study in JAMA Internal Medicine found that about 15% of reports from patients switching to generics mentioned reduced effectiveness - even when lab tests showed no difference. This is called the nocebo effect. If you’ve been told generics are inferior, your brain might convince you you’re feeling worse. But the FDA doesn’t ignore these reports. They’re still investigated. Why? Because if a patient stops taking their medication because they think it’s not working, that’s a real health risk - even if the drug itself is fine.What Happens When Something Goes Wrong?
When a pattern emerges - say, multiple reports of low blood pressure in patients taking a specific generic version of a heart drug - the FDA’s Office of Generic Drugs steps in. They dig into the data. Did all the reports come from one manufacturer? Was the batch number the same? Did the formulation change? If they find a problem, they can take action:- Update the drug’s label to warn about new risks
- Ask the manufacturer to recall a specific batch
- Issue a “Dear Healthcare Provider” letter
- Require the company to conduct a new study

Who’s Watching the Watchers?
Critics say the system isn’t enough. Public Citizen, a consumer advocacy group, argues that the FDA doesn’t have enough staff or funding to properly monitor over 15,000 approved generic drugs. And with 90% of prescriptions now filled with generics, the stakes are higher than ever. The National Academies of Sciences echoed this concern in a 2021 report, urging the FDA to create tailored surveillance plans for complex generics - not just one-size-fits-all monitoring. The FDA agrees. That’s why they’re moving toward AI. Machine learning can scan millions of reports, spot unusual clusters, and flag risks before humans even notice them. Early tests show AI could cut detection time from months to weeks.What You Can Do
You don’t have to wait for the FDA to find a problem. If you notice something unusual after switching to a generic - new dizziness, nausea, or a change in how the drug works - report it. Use MedWatch. Tell your doctor. Write down the manufacturer’s name and lot number on the bottle. These reports matter. They’re the eyes and ears of the system. And with over 4 billion generic prescriptions filled each year in the U.S., your voice is part of the safety net.The Future of Generic Drug Safety
By 2027, experts predict AI-driven surveillance could reduce detection time for safety signals in complex generics by 60-70%. Imagine a system that doesn’t just react to problems - but predicts them before they hurt people. The FDA’s goal isn’t to replace human judgment. It’s to give it better tools. The same science that powers your smartphone’s voice assistant is now being used to protect your health. The system isn’t perfect. But it’s evolving - fast. And it’s working. Because behind every generic pill on the shelf is a quiet, ongoing effort to make sure it’s safe, effective, and reliable - not just on day one, but for every dose you take.Are generic drugs as safe as brand-name drugs?
Yes, generic drugs are required by the FDA to be as safe and effective as their brand-name counterparts. They must contain the same active ingredient, dosage, and route of administration. The main difference is in inactive ingredients, which rarely cause issues. The FDA’s post-market surveillance system ensures ongoing safety, even after approval.
How does the FDA know if a generic drug is causing side effects?
The FDA uses multiple systems: the FDA Adverse Event Reporting System (FAERS) collects reports from doctors, patients, and manufacturers; the Sentinel Initiative analyzes health data from over 200 million Americans to spot trends; and MedWatch allows the public to report problems directly. These systems help identify patterns that suggest a drug may be linked to unexpected side effects.
Can I report a problem with a generic drug myself?
Yes. Anyone - patients, caregivers, or healthcare providers - can report side effects, medication errors, or product quality issues through MedWatch, the FDA’s online reporting system. Even if you’re not sure if the drug caused the problem, reporting it helps the FDA detect potential safety signals early.
Why do some people say generic drugs don’t work as well?
Sometimes it’s not the drug - it’s the mind. The nocebo effect can make people feel worse after switching to a generic, especially if they believe generics are inferior. Studies show many reports of reduced effectiveness don’t match lab results. But the FDA still investigates these reports because if patients stop taking their medicine, it can lead to real health risks.
What are complex generics, and why are they harder to monitor?
Complex generics include inhalers, topical creams, and extended-release pills where small changes in formulation can affect how the drug works in the body. Standard bioequivalence tests can’t always predict real-world performance. That’s why the FDA uses special tools, including AI and real-world data, to monitor these products more closely than simple tablets.
Does the FDA inspect generic drug factories?
Yes. The FDA conducts unannounced inspections of both U.S. and international manufacturing sites for generic drugs. These inspections check for compliance with quality standards, proper labeling, and consistent production. A single batch made with a different ingredient or process can trigger an investigation.




Just had to switch my dad to a generic for his cholesterol med last year. He swore it wasn’t working - same dose, same routine. Turned out the new batch had a different filler that made it harder to absorb. We reported it on MedWatch, and within three weeks, the pharmacy switched back to the old maker. The system works if you speak up.
I work in a pharmacy and see this all the time. People freak out when their generic looks different - same pill, different color, different shape. They think it’s fake. But 9 times out of 10, it’s just a different manufacturer. The FDA’s inspections are way stricter than most folks realize. Still, I always tell ’em to check the lot number if something feels off.
Let’s be real - the FDA is underfunded, overworked, and outsources half its inspections to countries where labor laws are a suggestion. You think they’re watching every batch of metformin made in India? Ha. The ‘AI surveillance’ they brag about? It’s just keyword scraping with a fancy name. Real safety comes from transparency - and right now, we’re trusting corporations to self-report. That’s like letting a fox guard the henhouse while it writes its own report.
Y’all act like generics are some miracle of modern medicine. Meanwhile, I’ve seen people have seizures after switching to a $2 generic version of Keppra. The FDA didn’t act until three people ended up in the ER. And now they’re patting themselves on the back for ‘improving AI detection’? Dude. That’s like saying your smoke alarm is better because it now beeps louder after the house burns down.
My sister has epilepsy. She’s been on the same generic levetiracetam for five years. Then, last year, the bottle looked different - smaller, lighter, white instead of blue. She started having breakthrough seizures. We called the pharmacy, found the lot number, reported it. The FDA issued that letter you mentioned - and within a month, her seizures stopped. This isn’t theoretical. It’s life or death. And yes, your report matters.
It’s not just about chemistry - it’s about trust. People don’t trust generics because they’ve been sold a narrative that ‘you get what you pay for.’ But the data doesn’t lie. For simple drugs, generics are just as safe. The real issue is the lack of public education. We need more doctors explaining this - not just handing out prescriptions and walking away.
My mom’s blood pressure spiked after switching generics. We didn’t know what to do - so we called her doctor, wrote down the manufacturer and lot number, and filed a MedWatch report. Two weeks later, the pharmacy switched her back. No drama. No lawsuit. Just a quiet, effective system. It works if you pay attention.
Oh wow, so the FDA’s got AI now? That’s cute. Meanwhile, I’ve got a cousin who died because his generic heart med had a bad batch - and the FDA didn’t act until 17 other people had heart attacks. You think they’re watching? They’re just waiting for the media to catch on. Then they do a press release and call it a win. This isn’t safety. It’s damage control with a PowerPoint.