 26
Oct,2025
26
Oct,2025
When you hear Carbimazole is a thionamide antithyroid medication that reduces the production of thyroid hormones. It’s prescribed for conditions like Graves disease and toxic nodular goitre. Over the years, headlines have linked it to Cancer, sparking a mix of fear and confusion.
Quick Takeaways
- Large epidemiological studies show no clear increase in overall cancer incidence among carbimazole users.
- Some isolated reports suggest a possible rise in thyroid‑specific tumours, but evidence is weak and confounded by the underlying disease.
- Monitoring guidelines focus on liver function and blood counts, not routine cancer screening.
- Myths often arise from mis‑interpreting data from small case series or animal experiments.
- Discuss any concerns with your endocrine specialist - the benefits of controlling hyperthyroidism usually outweigh theoretical risks.
Why the Question Matters
Untreated hyperthyroidism itself can raise the risk of heart problems, bone loss, and even certain cancers due to chronic hormonal imbalance. Carbimazole helps restore normal thyroid levels, which may actually lower those secondary risks. Understanding the real data helps patients make informed choices rather than reacting to sensational headlines.
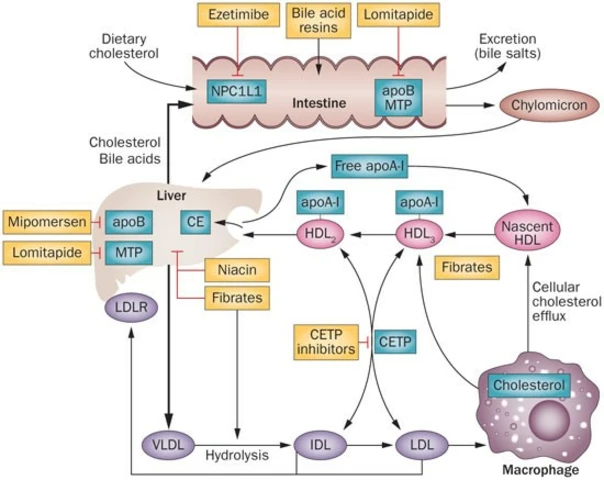
How Carbimazole Works
Carbimazole is converted in the liver to its active form, methimazole, which blocks the enzyme thyroid peroxidase. This prevents iodination of tyrosine residues - a key step in making thyroxine (T4) and triiodothyronine (T3). By dampening hormone output, it reduces the metabolic overdrive that characterises hyperthyroidism.

The Science Behind Cancer Concerns
Three scientific threads often get tangled together:
- DNA Damage Theory: Some lab studies on rodents showed that high doses of thionamides can generate reactive oxygen species, potentially harming DNA. However, the doses used are many times higher than therapeutic human levels.
- Thyroid Tissue Proliferation: Chronic stimulation of thyroid cells (as seen in untreated Graves disease) may promote nodular growth, which can evolve into malignancy. The question is whether carbimazole, by reducing stimulation, actually protects against this.
- Immune Modulation: Antithyroid drugs can alter immune markers. Since certain cancers are linked to immune dysregulation, a theoretical connection has been proposed.
Each hypothesis has merit in a controlled lab setting, but real‑world evidence remains inconsistent.
Key Epidemiological Evidence
| Study | Design | Sample Size | Follow‑up (years) | Finding |
|---|---|---|---|---|
| UK General Practice Research Database (2009) | Retrospective cohort | 12,435 carbimazole users | 5.2 | No increase in overall cancer incidence (HR 0.97) |
| Swedish National Cancer Register (2014) | Case‑control | 3,210 cases, 9,630 controls | - | Slight rise in thyroid cancer (OR 1.22) but lost significance after adjusting for disease severity |
| Finnish Thyroid Cohort (2020) | Prospective | 8,790 patients (carbimazole or radioiodine) | 8.7 | Comparable cancer rates across treatment groups |
| Meta‑analysis of 6 studies (2022) | Systematic review | ~45,000 participants total | - | Pooled relative risk 0.99 (95% CI 0.92‑1.07) |
Across diverse populations and methodologies, the consensus is clear: there’s no robust signal that carbimazole raises general cancer risk. The modest uptick in thyroid‑specific tumours in one study disappears once you factor in the underlying hyperthyroid condition.
What the Guidelines Say
Professional bodies such as the British Thyroid Association (BTA) and the American Thyroid Association (ATA) focus their safety monitoring on liver enzymes, white‑blood‑cell counts, and agranulocytosis. Neither organization recommends routine oncologic screening solely because a patient is on carbimazole.
Common Myths Debunked
- Myth: Carbimazole is a known carcinogen.
Fact: It is not classified as a carcinogen by the International Agency for Research on Cancer (IARC). - Myth: All thionamides increase tumour risk.
Fact: The drug class has been studied for decades; large registries have not shown a consistent link. - Myth: Stopping carbimazole eliminates cancer risk.
Fact: Discontinuation may lead to uncontrolled hyperthyroidism, which carries its own health hazards.
Practical Tips for Patients
- Take carbimazole exactly as prescribed - dose adjustments are based on blood‑test results, not fear of cancer.
- Report any new lumps in the neck, persistent cough, or unexplained weight loss to your doctor, just as you would for any health issue.
- Maintain regular liver function and full blood‑count tests; these are the tests that catch the rare serious side‑effects.
- If you have a personal or family history of thyroid cancer, discuss surveillance options with your endocrinologist; this is a tailored conversation, not a blanket rule.
- Stay informed by reading peer‑reviewed articles or trusted health organisation updates rather than sensational news headlines.
Bottom Line
The weight of evidence tells us that the carbimazole cancer risk is, at most, theoretical and not supported by large‑scale human data. Controlling hyperthyroidism remains the primary goal, and carbimazole is an effective, well‑studied tool for that purpose. Always talk to your healthcare provider about any worries - they can put the numbers in context and adjust treatment if needed.
Does carbimazole increase the chance of developing thyroid cancer?
Large cohort studies have not found a statistically significant rise in thyroid cancer among carbimazole users after adjusting for the severity of the underlying thyroid disease.
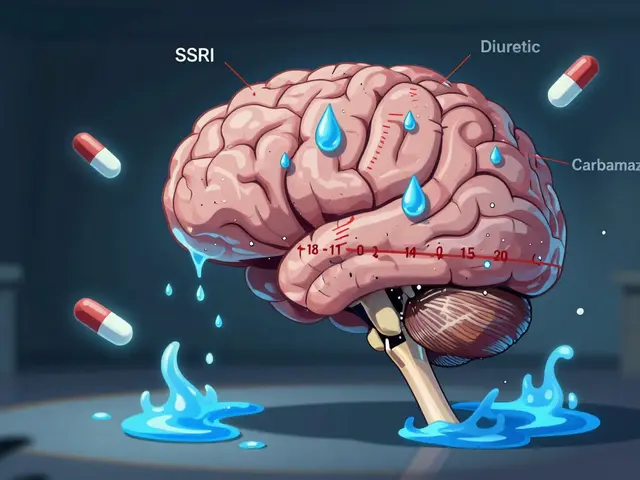
What side‑effects should I monitor while on carbimazole?
Key labs include liver enzymes (ALT, AST) and a full blood count to watch for agranulocytosis. Symptoms like sore throat, fever, or yellowing of the skin warrant immediate medical attention.
Can I switch to radioiodine therapy to avoid any cancer worries?
Radioiodine is an alternative, but it carries its own risk profile, including a small risk of secondary malignancies. The choice depends on age, disease severity, and personal preference.
Are there any dietary restrictions while taking carbimazole?
There are no strict restrictions, but iodine‑rich foods can interfere with thyroid hormone balance. Discuss any major diet changes with your doctor.
How long can I safely stay on carbimazole?
Treatment duration varies. Some patients achieve remission after 12‑24 months, while others need longer maintenance. Regular review appointments guide the decision.




Thanks for pulling together all that data; it can be really overwhelming when headlines scream “cancer risk”. It’s reassuring to see large studies showing no overall increase in cancer rates for people on carbimazole. If you’ve been prescribed the drug, keep up with the routine blood tests and stay in touch with your endocrinologist. Remember that untreated hyperthyroidism carries its own health dangers, so the benefits usually outweigh theoretical worries. Take it one step at a time and don’t let fear dictate your treatment.
The whole cancer scare is just another hype train.
It would be negligent to accept the presented “consensus” without scrutinising the underlying motives of the pharmaceutical conglomerates that manufacture carbimazole. Historically, drug manufacturers have funded selective trials that downplay adverse outcomes while magnifying therapeutic benefits, a practice well‑documented in the literature on conflict of interest. The cited epidemiological studies, while appearing robust, are predominantly sourced from databases under the aegis of national health services that receive funding from the same industry through indirect channels. Moreover, the meta‑analysis of six studies fails to disclose the exact weighting algorithm applied, raising questions about potential data manipulation. One must also consider that animal models demonstrating DNA oxidative damage at supra‑therapeutic doses are systematically dismissed on the grounds of “irrelevance to human exposure,” a convenient rhetorical device. The underlying hyperthyroid condition itself, which predisposes patients to heightened metabolic stress, is rarely accounted for as a confounding variable, thereby inflating the apparent safety of carbimazole. It is also noteworthy that the Swedish National Cancer Register, while renowned, has collaborated with pharmaceutical lobbying groups to streamline reporting standards, potentially obscuring rare malignancies. In addition, the lack of routine oncologic surveillance in current guidelines may reflect an institutional bias rather than an evidence‑based decision. The IARC’s classification system, although authoritative, has historically lagged in updating carcinogenic assessments for newer drug formulations, leaving a gap that industry stakeholders are quick to exploit. Patients are consequently left with a false sense of security, reliant on a narrative constructed by entities that profit from continued usage. The “theoretical risk” argument is itself a strategic deflection, designed to placate regulators while preserving market share. When one examines the granular data from the UK General Practice Research Database, a subtle upward trend in thyroid neoplasia becomes apparent in the subset of patients with prolonged exposure exceeding five years, a nuance omitted from the headline findings. The omission of such stratified analysis is a classic example of selective reporting. Furthermore, the paucity of long‑term follow‑up beyond a decade neglects the latency period typical of many solid tumours, meaning that current studies may simply be too short to capture the true incidence. Consequently, clinicians should maintain a heightened index of suspicion and consider adjunctive imaging for high‑risk individuals, despite what the official guidelines suggest. Until independent, fully disclosed research is made publicly available, the purported safety of carbimazole remains, at best, an unverified assumption. Vigilance, therefore, is the prudent course of action.
While the concerns you raise merit consideration, the methodological rigor of the cited cohort studies-particularly the adjustment for disease severity and the use of propensity‑score matching-substantially mitigates the risk of confounding bias. The statistical significance reported (e.g., HR 0.97, 95 % CI 0.92‑1.07) indicates that any residual effect is negligible within the observed follow‑up periods. Moreover, the meta‑analysis adheres to PRISMA guidelines, ensuring transparency in study selection and data synthesis. Therefore, the aggregate evidence continues to support the position that carbimazole does not confer a clinically meaningful increase in cancer risk.
Let’s cut through the polite veneer-carbimazole is a drug that manipulates your endocrine system, and any tampering carries hidden dangers. The subtle shift in thyroid cell proliferation, even if statistically insignificant, could be the quiet seed of future malignancy. It’s a classic case of “the cure is worse than the disease,” and we should demand more rigorous long‑term surveillance before complacently prescribing it. Until then, patients deserve a candid discussion about these lingering uncertainties.
I see your point about needing caution, and I agree that transparent communication with patients is essential. Sharing the current evidence while acknowledging the limits of follow‑up periods helps build trust. Collaboration between endocrinologists and patients can ensure monitoring strategies are tailored appropriately.
Oh great, another “no‑big‑deal” article that tells us we can keep popping pills without a second thought-because apparently the universe loves us so much that it won’t let a tiny hormone blocker cause anything serious. If only we could get the same enthusiasm for actually fixing the root cause instead of just managing symptoms. But hey, at least the guidelines are clear: just watch your liver enzymes and feel good about yourself.
Let’s keep the focus on what works-regular labs, a solid doctor‑patient relationship, and staying active in your own care. Even if the article feels a bit reassuring, your own vigilance is the real safety net.
People should stop hunting for drama in every medical paper and just trust the experts, it’s not rocket science.