INR: What It Is, Why It Matters, and How Medications Affect Your Blood Clotting
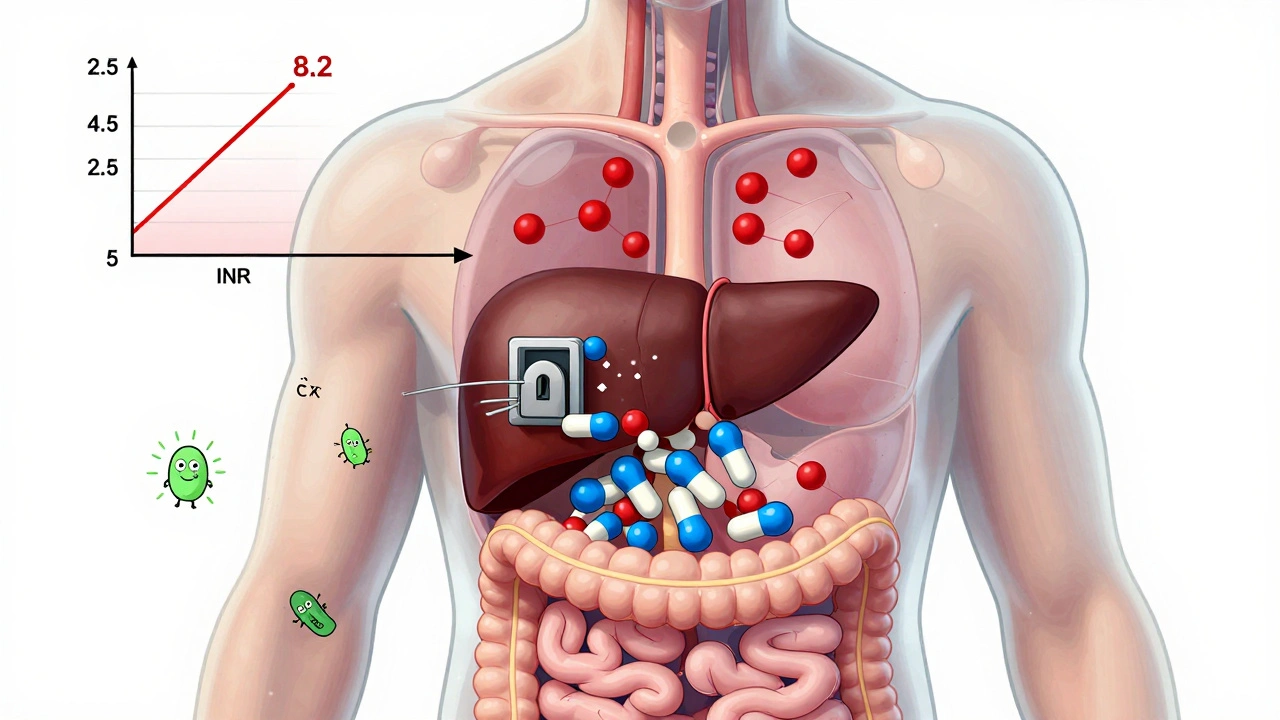
When your doctor talks about your INR, International Normalized Ratio, a standardized measure of how long your blood takes to clot. Also known as prothrombin time ratio, it’s the single most important number for people taking blood thinners like warfarin. Think of it like a traffic light for your blood: too low, and you risk clots that can cause strokes or heart attacks; too high, and you could bleed internally from a simple bump. It’s not a number you ignore—it’s a daily guide to staying safe.
INR doesn’t exist in a vacuum. It’s directly shaped by warfarin, a common anticoagulant that slows blood clotting by interfering with vitamin K, and by what you eat. Leafy greens, alcohol, antibiotics, even herbal supplements can swing your INR up or down. That’s why people on warfarin need regular blood tests—sometimes every week, sometimes every month. The goal? Keep it in the narrow window your doctor sets, usually between 2.0 and 3.0 for most conditions like atrial fibrillation or deep vein thrombosis. But if you’ve had a mechanical heart valve, your target might be higher. There’s no one-size-fits-all.
It’s not just warfarin that affects INR. Newer blood thinners like apixaban or rivaroxaban don’t require INR monitoring because they work differently. But if you’re switching from one to the other, your doctor will still check your INR to make sure the old drug is fully out of your system. And if you’re on multiple meds—say, an antibiotic for an infection while on warfarin—that’s when INR can spike dangerously. That’s why pharmacists are trained to flag drug interactions. They see the big picture: your pills, your labs, your diet. Your INR is a conversation between your body and your meds.
You’ll find posts here that dig into how anticoagulants, medications designed to prevent dangerous blood clots interact with everyday life—like how to travel with them, what to do if you miss a dose, or why your INR dropped after you started eating more kale. You’ll also see how INR monitoring, the process of regularly testing blood clotting time to adjust medication doses fits into broader safety systems like FDA post-market surveillance and pharmacist-led adverse event reporting. These aren’t abstract concepts. They’re real tools that keep people alive.
Whether you’re new to anticoagulants or have been on them for years, the posts below give you practical, no-fluff advice: how to read your lab results, what to ask your pharmacist, how to avoid dangerous mix-ups with OTC painkillers, and why some people need more frequent checks than others. This isn’t theory. It’s what happens when your medicine meets your life—and how to make sure it works without putting you at risk.
Warfarin and Antibiotics: How Common Drugs Can Spike Your INR Risk
Warfarin and certain antibiotics can dangerously raise your INR, increasing bleeding risk. Learn which antibiotics are risky, why the delay matters, and how to protect yourself with timely testing.
View more