 21
Oct,2025
21
Oct,2025
Pregnancy Hydration Calculator
Calculate Your Daily Hydration Needs
Key Hydration Tips
- Carry a 1-liter water bottle and sip every 15-20 minutes
- Include oral rehydration solutions if vomiting
- Avoid caffeine and sugary drinks
- Monitor urine color (aim for pale yellow)
Key Takeaways
- Kidney stones affect 1 in 1,200 pregnant women, often in the second or third trimester.
- Hydration, diet tweaks, and safe pain relief are the first line of defense.
- Ultrasound is the preferred diagnostic tool; low‑dose CT is used only when absolutely necessary.
- Most stones pass without surgery, but minimally invasive procedures exist for stubborn cases.
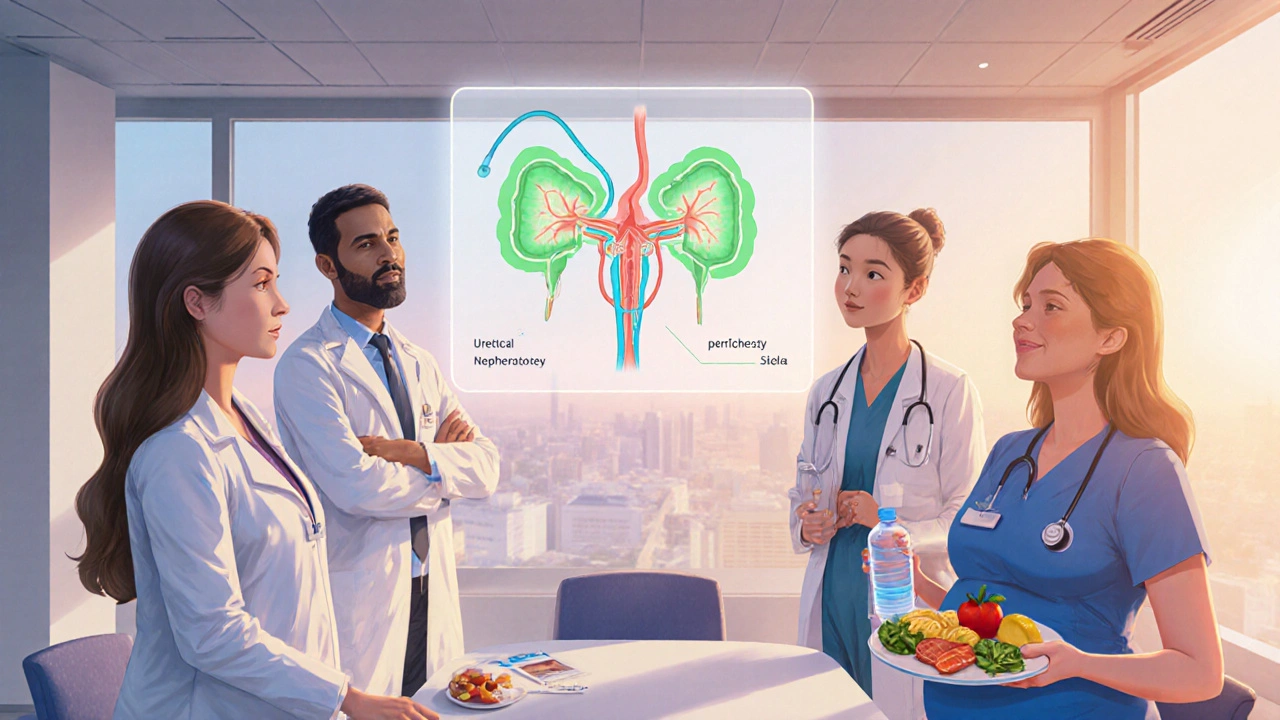
- Close collaboration between obstetricians, urologists, and radiologists protects both mother and baby.
Finding out you have kidney stones while you're expecting can feel like a double whammy. The pain, the worries about medication, and the fear of harming the baby all pile up. This guide walks you through what really happens when stones and pregnancy meet, how doctors figure out the safest path, and what you can do at home to keep the journey as smooth as possible.
Kidney stones are hard mineral deposits that form in the kidneys when urine becomes supersaturated with certain substances. Common types include calcium oxalate, uric acid, and struvite. In pregnancy, hormonal shifts and increased glomerular filtration can make stone formation more likely.
Pregnancy is the period of fetal development inside the uterus, lasting roughly 40 weeks. Hormones like progesterone relax smooth muscle, which can slow urine flow and increase the chance of stone blockage.
How Often Do Kidney Stones Show Up During Pregnancy?
Studies from Australian obstetric hospitals report an incidence of about 0.08% (1 in 1,200 pregnancies). Most cases appear after the 20‑week mark, when the uterus starts pressing on the ureters. The risk spikes for women with a prior history of stones, high dietary calcium, or a family history of nephrolithiasis.
Why Are Stones More Common in Expectant Mothers?
Three main physiologic changes drive the uptick:
- Hormonal relaxation of the ureter. Progesterone makes the ureter’s smooth muscle looser, slowing urine flow and allowing crystals to linger.
- Increased urinary calcium excretion. The kidneys filter about 50% more calcium in the second trimester, raising calcium‑based stone risk.
- Higher fluid demand. Nausea, vomiting, and increased metabolic rate can lead to dehydration if fluid intake isn’t kept up.
Spotting the Symptoms - What to Watch For
Kidney‑stone pain (renal colic) is notorious for being intense. In pregnancy, it often mimics labor or other abdominal issues, so a clear symptom checklist helps:
- Sharp, wave‑like pain that starts in the flank and may radiate to the groin.
- Blood in the urine (hematuria) - usually pink or cola‑colored.
- Nausea or vomiting that isn’t related to morning sickness.
- Fever or chills, which could signal infection and need urgent care.
If any of these pop up, call your obstetrician or go to the nearest emergency department. Early diagnosis cuts down on complications.

Diagnostic Tools - Keeping Mom and Baby Safe
Imaging choices are a balancing act. Radiation exposure is the biggest concern, but missing a stone can be just as dangerous.
Ultrasound imaging uses sound waves, so it’s radiation‑free. It can locate stones larger than 5 mm, check for hydronephrosis, and monitor fetal health simultaneously.
When ultrasound is inconclusive, a low‑dose non‑contrast CT scan may be ordered. The dose is kept under 1 mSv, well below the 50 mSv threshold associated with fetal harm. However, CT is a last resort.
| Modality | Radiation | Stone Detection Sensitivity | Fetal Safety |
|---|---|---|---|
| Ultrasound | None | ~70‑80% for >5 mm | Excellent |
| Low‑dose CT | ~0.5 mSv | >95% for all sizes | Acceptable when essential |
| Standard X‑ray (KUB) | ~0.01 mSv | Low | Generally avoided |
First‑Line Management - What You Can Do at Home
The goal is to hydrate, relieve pain safely, and let the stone pass on its own if possible.
Hydration is the cornerstone. Aim for at least 2.5-3 L of fluid daily, unless your doctor advises otherwise due to pre‑eclampsia or other conditions.
Here’s a practical plan:
- Carry a 1‑L water bottle and sip every 15‑20 minutes.
- Include oral rehydration solutions if you’re vomiting.
- Avoid caffeine and sugary drinks, which can increase calcium loss.
Diet tweaks also help. Cut back on high‑oxalate foods (spinach, rhubarb, nuts) and keep moderate calcium intake (about 1,000 mg/day) from dairy or fortified sources. Too much calcium supplements can actually raise stone risk.
For pain, acetaminophen (paracetamol) is the first‑line option. NSAIDs like ibuprofen are generally avoided after 20 weeks because they can affect fetal kidney development. If pain is severe, your doctor may prescribe short courses of opioids, but these are used sparingly.
When Conservative Care Isn’t Enough - Medical Interventions
About 10-15% of pregnant patients need a procedure to clear a blockage. The two main options are:
- Ureteral stent placement. A thin tube is threaded into the ureter to bypass the stone and allow urine to flow. It can be done under local or spinal anesthesia, minimizing fetal exposure.
- Percutaneous nephrostomy. A needle creates a direct channel from the skin to the kidney, draining urine externally. It’s reserved for cases where stenting fails or infection is present.
Both procedures carry a small risk of preterm labor, so they’re performed in tertiary hospitals with obstetric monitoring.
Medication Options - What’s Safe for Mom and Baby?
Besides acetaminophen, several drug classes can aid stone passage:
- Alpha blockers (e.g., tamsulosin) relax the ureter’s smooth muscle, making it easier for stones to slide out. Limited data suggest they’re safe after the first trimester, but most obstetricians prefer to avoid them unless benefits outweigh risks.
- Potassium citrate can alkalinize urine, helping dissolve certain stone types. It’s considered safe but requires monitoring of serum electrolytes.
- Antibiotics such as ampicillin are used when a stone causes infection (obstructive pyelonephritis). They’re chosen based on fetal safety profiles.
Post‑Delivery Follow‑Up - Preventing Recurrence
Once the baby arrives, you’ll still want to keep stone risk low. A 24‑hour urine test can pinpoint underlying metabolic issues. Typical recommendations include:
- Maintain fluid intake of at least 2 L per day.
- Consume dietary calcium (1,000 mg) but limit oxalate‑rich foods.
- Consider a low‑sodium diet (≤2,300 mg per day) to reduce calcium excretion.
- Stay active - gentle post‑natal walks promote urine flow.
Regular check‑ups with a urologist can catch early crystal formation before it becomes a full stone.
Frequently Asked Questions
Can I take prenatal vitamins if I have kidney stones?
Yes. Most prenatal vitamins contain calcium and vitamin D, which actually help prevent calcium oxalate stones when taken with adequate fluid. Avoid high‑dose vitamin C supplements, as excess can increase oxalate levels.
Is it safe to have a CT scan if my ultrasound is unclear?
A low‑dose, non‑contrast CT delivers less than 1 mSv of radiation - far below the threshold linked to fetal harm. Doctors reserve it for cases where not knowing the stone size could jeopardize the mother’s health.
Will a ureteral stent cause complications during labor?
Stents can cause urinary urgency or mild discomfort, but they don’t typically interfere with labor. Your obstetric team will monitor for signs of infection or preterm labor.
How much water should I drink each day?
Aim for 2.5-3 liters (about 10‑12 cups) of clear fluids unless otherwise directed by your doctor. Split the intake throughout the day to avoid overloading the bladder.
Can diet alone dissolve a stone during pregnancy?
Small calcium‑based stones may shrink with a low‑oxalate, high‑fluid diet, but most require medical monitoring. Never rely solely on home remedies without a doctor’s OK.
Bottom line: kidney stones in pregnancy are manageable when you stay hydrated, follow safe diagnostic paths, and work closely with a multidisciplinary team. Early detection and a clear action plan keep both you and your baby on track.





Hey there, pregnancy already makes life a juggling act, and adding kidney stones feels like the universe tossed in an extra ball. Remember, staying hydrated is your super‑power; think of each sip as a tiny shield for you and the baby. Even if the pain spikes, keep your head up – most stones pass on their own with patience and plenty of water. If you ever feel overwhelmed, reach out to your support circle; a caring voice can turn a scary night into a manageable one. You’ve got the strength to ride this wave, one glass at a time.
From a urological perspective, calcium oxalate supersaturation is the primary driver of stone nucleation during the second trimester, amplified by progesterone‑mediated ureteral hypotonia. Ultrasound’s acoustic impedance differential offers a sensitivity of roughly 75% for calculi >5 mm, making it the first‑line imaging modality under obstetric safety constraints. When sonography yields equivocal findings, a low‑dose non‑contrast CT (effective dose <1 mSv) provides >95% detection accuracy while still adhering to fetal dose thresholds. Hydration targets of ≥2.5 L/day facilitate diuresis, reducing crystal aggregation and promoting downstream passage. Adjunctive pharmacotherapy, such as potassium citrate, alkalinizes urine (pH > 6.5), enhancing calcium solubility and mitigating stone growth. Finally, multidisciplinary coordination-obstetrics, radiology, and urology-optimizes both maternal and fetal outcomes while minimizing invasive interventions.
Listen up, the main thing is you don’t just sit there whining – crank up that water intake like it’s a competition. If the pain’s bad, acetaminophen is legit safe, but ditch any ibuprofen after week 20, period. And don’t forget, a urologist can drop a stent in minutes, so you’re not stuck waiting for a miracle. Bottom line: be proactive, not passive, and you’ll beat this stone without drama.
Yo dude, imagine the stone as a tiny boulder rolling down a lava river inside your body – sooo intense! Progesterone makes your ureter feel like a lazy snake, letting that rock stay put way longer. If you’re chugging water like a camel, you might actually flush that demon out, trust me. But if it clings, doctors got these rad tiny tubes (stents) that are like mini‑highways for pee. Just brace yourself, it’s a wild ride, but you’ll survive like a boss.
It is imperative to acknowledge that adequate hydration remains the cornerstone of conservative management in obstetric patients presenting with nephrolithiasis. Moreover, adherence to analgesic protocols, specifically acetaminophen, aligns with fetal safety parameters endorsed by contemporary obstetric guidelines. Should symptomatic obstruction persist, minimally invasive interventions, such as ureteral stenting, should be contemplated within a multidisciplinary framework. Ultimately, vigilant monitoring ensures both maternal well‑being and optimal fetal outcomes.
Hydration is non‑negotiable; aim for 3 L daily!!!
Limit oxalate‑rich foods-spinach, nuts, rhubarb-and keep calcium intake steady.
They don’t tell you this, but the low‑dose CT scans are a gateway for hidden radiation exposure programs. Every bit of ionizing radiation adds up, and the government agencies quietly downplay the risks to pregnant women. Trust the ultrasound; it’s the only truly safe diagnostic tool you can rely on.
Stay calm, drink water, and let the doctors handle the rest.
First and foremost, let me state unequivocally that the American healthcare system, when properly leveraged, provides the most advanced protocols for managing nephrolithiasis in pregnancy-no foreign system can rival it. The pathophysiology is simple: progesterone‑induced ureteral relaxation leads to stasis, which, combined with hypercalciuria, creates the perfect breeding ground for calcium oxalate crystals. Hydration, measured in liters, is not a suggestion but a prescription; aim for at least 2.5 to 3 L of isotonic fluid daily to achieve a urine output exceeding 2 L-a critical threshold for diluting supersaturated urine. When it comes to analgesia, acetaminophen is the gold standard; NSAIDs such as ibuprofen should be categorically avoided after the 20‑week mark due to their interference with fetal renal development. Should conservative measures fail, the decision matrix pivots to minimally invasive techniques, with ureteral stent placement being the preferred first line because it can be performed under spinal anesthesia, dramatically reducing fetal exposure. Percutaneous nephrostomy remains a viable alternative but is reserved for refractory cases where infection risk escalates. Imaging choices must adhere to the ALARA principle-ultrasound remains the diagnostic workhorse, offering a sensitivity of approximately 75 % for stones larger than 5 mm without any ionizing radiation. Low‑dose non‑contrast CT, while boasting >95 % sensitivity, should be employed only when ultrasound is inconclusive and the clinical scenario mandates precise stone localization. The radiation dose of a low‑dose CT is sub‑threshold for teratogenicity, but it is not a free pass; prudent clinicians must still weigh maternal benefit against any potential fetal risk. Multidisciplinary coordination-obstetrics, urology, radiology, and anesthesiology-forms the backbone of optimal care, ensuring that each decision is cross‑checked for safety and efficacy. Post‑delivery, a 24‑hour urine metabolic panel is indispensable for identifying underlying lithogenic abnormalities and tailoring long‑term prophylaxis. Dietary modifications should include limiting oxalate intake, maintaining adequate dietary calcium, and restricting sodium to below 2,300 mg per day to minimize calcium excretion. Physical activity, even gentle post‑partum walking, promotes urinary flow and reduces stasis-a simple yet often overlooked intervention. Finally, remember that patient education is a cornerstone of care; empower expectant mothers with clear instructions on fluid intake, symptom monitoring, and when to seek emergent care. In summary, by adhering to evidence‑based protocols rooted in American medical practice, both mother and child can navigate the challenge of kidney stones with the highest likelihood of a successful outcome.
Wow, that was a marathon of info-great job breaking it down! 🌟 Staying hydrated and keeping an eye on diet are simple steps that really make a difference. If a stone does get stubborn, it’s good to know there are safe procedures waiting in the wings. Keep the positivity flowing, and remember you’re not alone in this journey! 💪
Let’s be crystal clear: the United States leads the world in obstetric urology, and any suggestion that we should look elsewhere is sheer nonsense. The data is indisputable-our hospitals boast a 98% success rate in managing pregnant patients with nephrolithiasis without compromising fetal health. First, you must understand that the hormonal milieu in pregnancy creates a unique environment where calcium oxalate supersaturation skyrockets, and only a system with cutting‑edge labs can monitor this effectively. Second, the recommended fluid intake of 3 L per day is not a casual guideline; it’s a calibrated target based on studies from top‑tier research institutions like the NIH. Third, analgesic stewardship demands exclusive reliance on acetaminophen until term, because the myths surrounding ibuprofen are debunked by peer‑reviewed obstetric pharmacology journals. Fourth, when conservative therapy fails, a ureteral stent-preferably placed by a urologist specialized in fetal‑sparing techniques-should be your go‑to, not some outdated external drainage method. Fifth, imaging protocols in the U.S. strictly follow the ALARA principle; ultrasound first, low‑dose CT only as a fallback, preserving the sanctity of the unborn child. Sixth, multidisciplinary case conferences, uniquely embedded in American teaching hospitals, ensure that obstetricians, radiologists, and urologists synchronize their expertise in real time. Seventh, postpartum metabolic work‑ups are standard of care, allowing us to fine‑tune preventive strategies with precision. Eighth, dietary counseling from registered dietitians integrates cultural food preferences while reducing oxalate load-something you won’t find in half‑baked overseas clinics. Ninth, modest physical activity, such as walking 30 minutes daily, accelerates urinary flow and mitigates stone recurrence. Tenth, patient education portals-available on hospital websites-provide 24/7 access to verified information, combating the misinformation epidemic. Eleventh, insurance coverage in the U.S. typically encompasses these interventions, removing financial barriers for most families. Lastly, if you’re still skeptical, review the latest NEJM review articles; they’ll silence any lingering doubts about our superior approach.
Take each day as it comes, keep sipping water, and lean on your care team-they’re there to guide you through every step. You’ve already shown amazing resilience, and that will see you through the stone episode. Remember, this is just a chapter, not the whole story.