 12
Feb,2026
12
Feb,2026
SSLR Symptom Checker
What is Serum Sickness-Like Reaction?
SSLR is a delayed reaction to antibiotics (usually cefaclor or amoxicillin) that appears 7-10 days after starting treatment. It's NOT an allergy but a chemical reaction where the body processes the drug differently.
Check Your Child's Symptoms
Results
Likely Serum Sickness-Like Reaction (SSLR)
Your child's symptoms match SSLR patterns: rash that moves, fever, joint pain without breathing trouble or swelling.
What to do now: Stop the antibiotic immediately. Symptoms usually improve within 3-7 days. Use antihistamines for itching and ibuprofen for joint pain. Do NOT label this as an allergy—this could lead to unnecessary antibiotic restrictions.
Not likely SSLR
Your child's symptoms don't match typical SSLR patterns. This could indicate a true allergy or other condition. Seek immediate medical attention if breathing trouble or swelling is present.
What to do now: Contact your doctor immediately. This could be a true allergic reaction requiring epinephrine or other emergency treatment.
Possible SSLR but requires medical evaluation
Your child has some SSLR symptoms but may need doctor confirmation.
What to do now: Contact your pediatrician for evaluation. Do not restart the antibiotic. This could be SSLR but requires professional diagnosis to rule out serious conditions.
When a child gets a rash after taking an antibiotic, most parents panic. Is it an allergy? Should they avoid all penicillins for life? The truth is, serum sickness-like reaction (SSLR) isn’t an allergy at all - and mistaking it for one can lead to years of unnecessary treatment risks and higher healthcare costs.
SSLR shows up 7 to 10 days after a child takes certain antibiotics, most often cefaclor (a common ear infection drug), but sometimes amoxicillin. It doesn’t happen right away like anaphylaxis. Instead, it creeps in slowly: first a fever, then a rash that moves around the body, and often swollen joints. The rash looks like hives - raised, red, itchy patches - but unlike regular hives, it doesn’t stay in one spot. It fades in one area and pops up somewhere else, sometimes every hour. Kids may feel tired, have sore knees or wrists, and feel generally unwell. But here’s the critical part: their kidneys are fine, their lungs are fine, and they’re not in danger.
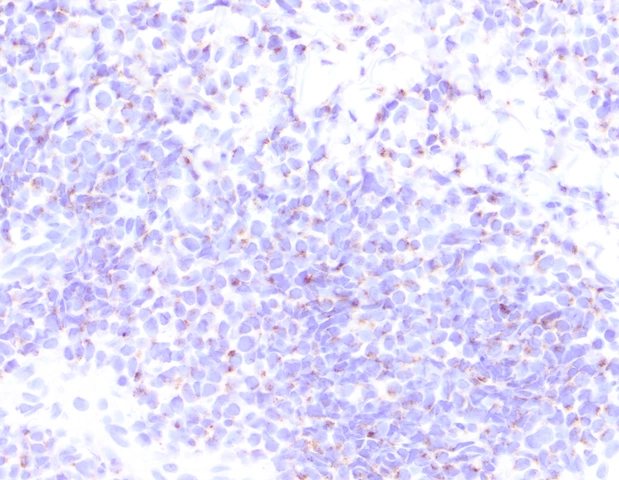
True serum sickness, the kind first described in 1906 after people got antiserum for rabies, is rare today. It causes kidney damage, low complement levels, and immune complexes floating in the blood. SSLR? None of that. Blood tests show normal C3 and C4 levels. Urine tests come back clean. No vasculitis. No protein in the urine. This isn’t a systemic immune crash - it’s a delayed, localized reaction tied to how some kids’ bodies process certain antibiotics.
Why Cefaclor? And Why Kids?
About 78% of SSLR cases happen in children under 6. The reason isn’t fully understood, but evidence points to a metabolic quirk. Some kids inherit a variant in the CYP2C9 gene that slows down how their liver breaks down cefaclor. This leads to a buildup of a specific metabolite that triggers the immune response. It’s not an allergy to the drug - it’s a chemical imbalance that fools the immune system into reacting. That’s why only a small fraction of kids on cefaclor get this reaction - about 1 in 100 prescriptions - but it’s the most common cause of SSLR in children.
Other antibiotics linked to SSLR include amoxicillin, azithromycin, and in rare cases, minocycline. But unlike true allergies, where cross-reactivity is a real concern, SSLR doesn’t mean your child can’t take other antibiotics. In fact, 89% of kids who had SSLR from cefaclor tolerate other cephalosporins just fine. The problem isn’t the drug class - it’s the specific molecule. That’s why doctors now avoid calling it an “allergy” and instead label it as “SSLR triggered by cefaclor.”
How Doctors Tell It Apart
Many pediatricians mistake SSLR for a viral rash, especially during cold and flu season. A child gets a fever and rash after antibiotics - maybe it’s just a virus? But SSLR has patterns. The rash appears 1-21 days after the drug was started (most often day 7). Fever is usually mild to moderate (38-39°C). Joint pain is symmetric - knees, wrists, ankles. No breathing trouble. No swelling of the lips or tongue. No low blood pressure. If the child had true anaphylaxis, it would’ve happened within minutes. If it’s a viral exanthem, the rash wouldn’t move around so dramatically.
Key lab clues:
- Normal white blood cell count (no spike)
- No protein or blood in urine
- Normal complement levels (C3, C4)
- No cryoglobulins
- No elevated ASO titers (rules out rheumatic fever)
Most importantly, if you stop the antibiotic, the symptoms fade - fast. In 92% of cases, the rash and joint pain disappear within 3 to 7 days. No steroids needed. No hospitalization. Just time and rest.

What to Do If It Happens
First: stop the antibiotic immediately. Don’t wait. If the child is still on the drug after the rash appears, the reaction can worsen. Get them off it within 24 hours if possible.
Second: manage symptoms. Second-generation antihistamines like cetirizine (0.25 mg/kg every 12 hours) work well for itching. For joint pain, ibuprofen (10 mg/kg every 8 hours) is safe and effective. Most kids don’t need steroids. But if the rash is severe, the child can’t sleep, or joint pain is keeping them from walking, a short 7-10 day course of prednisone (1 mg/kg/day, then tapered) can help.
Third: don’t label it as an allergy. This is the biggest mistake. If the child’s chart says “penicillin allergy” because they had SSLR from amoxicillin, they’ll be put on broader-spectrum antibiotics like vancomycin or clindamycin for every future infection. These drugs are more expensive, harder on the gut, and increase the risk of C. diff infections. A 2022 study found that 42% of SSLR patients ended up on unnecessary broad-spectrum antibiotics - adding up to $187 million in extra healthcare costs annually in the U.S. alone.
Can They Take Antibiotics Again?
Yes - but not the one that caused it. After 6 to 36 months (most often 12 months), a supervised oral challenge can be done by an allergist. In 92% of cases, the child tolerates other antibiotics without issue. One parent on Reddit shared: “My son had SSLR at age 3 from cefaclor. At age 5, we did a challenge with amoxicillin. No reaction. He’s now on amoxicillin for every ear infection.”
But avoid rechallenging with the same drug. If cefaclor triggered it, don’t try it again. If amoxicillin was the culprit, avoid it. But other penicillins? Other cephalosporins? Usually fine.

What’s New in 2025
The 2024 International Consensus Document officially gave SSLR its own ICD-11 code: RA43.1. This means doctors can now code it accurately - no more “allergy” misclassification. The FDA is also pushing for SSLR to be clearly noted on antibiotic labels.
Research is moving fast. A study at the University of California is testing a urine test that detects specific cefaclor metabolites. In early trials, it spotted SSLR with 94% accuracy. If it becomes routine, we could diagnose it without waiting for symptoms to fade.
AI tools are also helping. Boston Children’s Hospital is piloting an EHR alert system that flags when a child gets a rash 7-10 days after cefaclor. The system has 88% sensitivity and 91% specificity. It’s not perfect - but it’s cutting down misdiagnosis.
What Parents Should Remember
- SSLR is not an allergy. It’s a delayed immune reaction to a specific drug.
- Cefaclor is the #1 trigger - especially in kids under 5.
- Stop the antibiotic immediately if rash + fever + joint pain appear 1-3 weeks after starting it.
- Antihistamines and ibuprofen are usually enough. Steroids only if symptoms are severe.
- Don’t let your child be labeled “penicillin allergic” because of SSLR. Ask for an allergist referral.
- Rechallenge after 12 months is safe and recommended for most children.
- SSLR doesn’t affect future vaccines. Rabies or tetanus shots? Still safe.
One last thing: if your child had SSLR, keep a note in your phone: “SSLR after cefaclor - not a true allergy.” Share it with every doctor. This one note could save them from years of risky, expensive, and unnecessary treatments.
Is serum sickness-like reaction the same as a penicillin allergy?
No. A penicillin allergy is an IgE-mediated reaction that happens within minutes and can cause anaphylaxis. SSLR is a delayed T-cell-mediated reaction that occurs days after taking the drug. It causes rash, fever, and joint pain - not breathing trouble or shock. Lab tests show no immune complexes or complement drop, which confirms it’s not an allergy.
Can my child take other antibiotics after having SSLR?
Yes, absolutely. Only the specific antibiotic that triggered the reaction needs to be avoided. For example, if cefaclor caused SSLR, your child can still safely take amoxicillin, cephalexin, or azithromycin. Studies show 89% of children tolerate other cephalosporins without issue. An allergist can perform a supervised challenge if you’re unsure.
How long does SSLR last?
Most children recover in 3 to 7 days after stopping the antibiotic. The rash fades first, then joint pain. In about 8% of cases, mild symptoms like occasional rash or joint stiffness can linger for up to 3 months, but these are rare and don’t require treatment. No long-term damage occurs.
Should I avoid all cephalosporins if my child had SSLR from cefaclor?
No. Cefaclor is a specific second-generation cephalosporin. Other cephalosporins like cephalexin (Keflex) or cefdinir (Omnicef) have different chemical structures and rarely trigger SSLR. Avoiding all cephalosporins is unnecessary and can lead to using less effective or more toxic antibiotics. Only avoid the exact drug that caused the reaction.
Why do some doctors still call it an allergy?
Because the symptoms look like an allergic reaction - rash, fever, itching. Many pediatricians aren’t trained to recognize the subtle differences. A 2022 study found 74% of pediatricians incorrectly document SSLR as “penicillin allergy” in electronic records. This leads to lifelong avoidance and inappropriate antibiotic choices. Always ask for an allergist evaluation if SSLR is suspected.
Can SSLR happen again if my child takes the same antibiotic later?
Yes. Re-exposure to the same drug - like cefaclor - almost always causes a recurrence, and it can be more severe. That’s why the drug must be permanently avoided. But as mentioned, other antibiotics are generally safe. Never give the triggering drug again.
Is SSLR dangerous?
In most cases, no. It’s uncomfortable and concerning, but not life-threatening. Unlike true serum sickness, it doesn’t damage kidneys, lungs, or other organs. The biggest danger is misdiagnosis - leading to unnecessary use of broad-spectrum antibiotics, which increases the risk of resistant infections and gut problems. With proper recognition and management, SSLR is a self-limiting condition with no long-term consequences.



Man, I wish I'd known this when my daughter broke out in that wild rash after her ear infection meds. We thought it was an allergy and she's been labeled 'penicillin allergic' ever since. Now I'm kicking myself-she missed out on so many simpler, cheaper treatments. This post is a game-changer. I'm printing it out and handing it to every pediatrician we see from now on.
Also, that 2022 study about $187 million in wasted costs? Yeah, that's real. We're not just talking about one family here-we're talking about a systemic failure. Doctors need to stop calling this an allergy. It's not even close.
just wanted to say thank u for this. my son had sslr from cefaclor at 2.5 yrs. we were scared to death. doc said 'allergy' and we believed it. now at 7, he's on amoxicillin for his 3rd ear infection this year-no probs. no steroids, no hospital, just a rash that went away in 4 days. i wish i'd known back then what i know now. pls share this with every parent you know. it could save someone from years of bad meds.
ps: antihistamines + ibuprofen worked like magic. no need to overreact. chill out, stop the drug, and let it run its course.
Oh wow, so you're telling me that after 30 years of medical practice, pediatricians still can't tell the difference between a rash and an allergy? And now we have a whole new term-SSLR? How many more buzzwords are we going to invent before we actually fix the system? This isn't science, this is bureaucratic gymnastics.
Let me guess-next they'll call it 'immune confusion syndrome' and charge $800 for a 'specialized consultation.'
And don't even get me started on that urine test. Who's paying for it? The parents? Of course. Because healthcare is just a pyramid scheme with stethoscopes.
Also, why is cefaclor the #1 trigger? Because Big Pharma wanted a cheaper alternative to amoxicillin and didn't test for metabolites. Surprise surprise. You're all just lab rats in white coats.
So… we’ve been mislabeling a self-limiting reaction as a life-threatening allergy… for decades?
And now we’re gonna slap an ICD-11 code on it and call it progress?
😂
Meanwhile, my kid’s chart still says ‘penicillin allergy’ because the nurse didn’t read past the word ‘rash.’
AI alerts? Cool. But someone still has to click ‘confirm.’
Meanwhile, in 2025, we’re still using paper charts in 70% of clinics.
It’s not a science problem. It’s a paperwork problem.
I just want to say how much I appreciate this post-it's so clear, so thoughtful, and so needed. As a mom of two kids who both had SSLR (one from cefaclor, one from amoxicillin), I spent YEARS feeling guilty, confused, and terrified that I'd somehow 'broken' my kids by giving them antibiotics.
The fact that this isn't an allergy? That they can safely take other drugs? That it's not dangerous? That it resolves on its own? This is the kind of info that changes lives. I wish I'd had this when my first child broke out in that awful rash. I cried for three days thinking we'd ruined her. Turns out? We just needed to stop the drug and give her some ibuprofen.
And yes-I've been screaming this from the rooftops since. My sister's kid just had SSLR last month, and I sent her this whole article. She cried too-but this time, it was from relief.
Please, doctors-stop calling it an allergy. Parents are scared enough. We don't need another label that makes us feel like we failed.
So let me get this straight-you're telling me a kid gets a rash, and instead of immediately going into full allergy protocol, we should just wait and see if it goes away? And then, what? Just give them antihistamines? No labs? No specialists? No second opinion?
This sounds like medical malpractice waiting to happen. What if it *is* something worse? What if it's early-stage lupus? Or Kawasaki? Or a hidden infection?
And you're just telling parents to stop the drug and 'chill out'? That's not medicine. That's a blog post with a pretty chart.
I'm not saying this is wrong-I'm saying it's dangerously oversimplified. If you're going to tell parents to ignore a rash, you better have a 99.9% accuracy rate. And we don't. Not even close.
lol this is why americans are so dumb. they think every rash is an allergy. in nigeria, we just give paracetamol and wait. if the kid dies, well… that’s life.
also, why is everyone so obsessed with labels? ‘sslr’? ‘not an allergy’? you people need to stop overthinking everything. just stop the drug. give medicine. if they get better, good. if not, take them to hospital. done.
you’re making a science problem into a social media trend. 🤡
Okay, I’ve been waiting for someone to say this, and now I have to speak up: THIS IS A BIG PHARMA SCAM. Cefaclor was pushed hard in the 90s because it was cheap to make-and guess what? They knew about the metabolite issue but buried the data. Now they’re slapping on a new code, a new test, a new ‘solution’-all while the same companies still make the drug!
And don’t even get me started on the ‘supervised challenge’-who’s paying for that? The parents? Of course. And then they’ll charge you $500 for a 10-minute appointment where the allergist just says, ‘Yep, you’re fine.’
They’re monetizing fear. They’re monetizing confusion. And they’re monetizing your kid’s rash.
I’m not saying this isn’t real-but I’m saying the whole system is rigged. And if you believe this is just ‘medical progress,’ you’re being played.
As an Indian parent, I find this entire discussion laughably Western. In our country, we have no access to cefaclor, no EHR alerts, no allergist referrals. Our kids get amoxicillin. If they get a rash? We give paracetamol. If they get worse? We go to the local clinic. No labels. No codes. No $187 million in costs.
Why are we spending so much energy on terminology when most of the world doesn’t even have antibiotics in stock?
Also, why is everyone so obsessed with ‘not calling it an allergy’? In India, we call it ‘drug rash.’ Simple. Clear. No drama.
This post reads like a marketing brochure for American pediatricians. Real talk: most of the world doesn’t need ICD-11 codes. They need pills. And clean water.
Just wanted to say-this post saved me. My 4-year-old had SSLR last year. We were terrified. The ER doc said, 'Penicillin allergy. Avoid all beta-lactams.' We believed him.
Then I found this thread. Changed everything.
We did the challenge at 14 months later-amoxicillin. Zero reaction. He’s now on it for every infection. No steroids. No panic. Just a happy kid with a clean chart.
And yeah, I’m telling everyone. My sister’s kid had the same thing. She’s now the one sharing this article. It’s like a chain reaction of relief.
Thank you for writing this. Seriously. This is the kind of info that fixes healthcare-one parent at a time.
Replying to myself because I just had to add this: I called my kid’s allergist yesterday and asked if they could update her chart. They said, 'We don’t have the authority.' So I emailed the pediatrician’s office. They replied: 'We’ll update it next time she comes in.'
Next time? She’s due for a vaccine next month.
So I printed out this entire post. Highlighted the key lines. Taped it to her chart.
And now I’m calling every doctor’s office in the state. If they won’t update it… I’ll hand them the paper. One by one.
This isn’t just about one kid. It’s about fixing a system that’s still stuck in 1995.