 22
Jan,2026
22
Jan,2026
Medication Palpitation Risk Checker
This tool helps you assess the risk of your medications causing palpitations based on clinical evidence. Select medications you're taking to see your risk level.
Feeling your heart race for no reason? Like it’s fluttering, pounding, or skipping beats? You’re not alone. Many people experience palpitations after starting a new medication - and most don’t realize the drug could be the cause. It’s not just anxiety or caffeine. Sometimes, it’s something in your medicine cabinet.
What Exactly Are Medication-Induced Palpitations?
Palpitations are when you suddenly notice your heartbeat - too fast, too hard, or irregular. It’s not a disease itself, but a symptom. And when it’s caused by medication, it’s called medication-induced palpitations. These aren’t rare. According to the American Heart Association, up to 20% of all arrhythmia cases seen in clinics are tied to drugs. That’s one in five people who think they’re just “nervous” or “stressed” - but their heart is reacting to something they’re taking. The problem isn’t always obvious. You might start a new antibiotic, asthma inhaler, or thyroid pill and feel fine at first. Then, a few days later, your heart starts acting up. That’s because some medications don’t cause problems right away. They build up. Or they interact with other drugs you’re already on. Or your body just reacts differently than expected.Common Culprits: Which Medications Cause Rapid Heartbeat?
Not all drugs affect the heart the same way. Some speed it up directly. Others mess with the heart’s electrical system, leading to dangerous rhythms. Here are the most common offenders, backed by clinical data:- Asthma inhalers (beta-2 agonists): Albuterol (Ventolin, ProAir) can spike your heart rate by 15-25 beats per minute within 30 minutes. If you’re using it more than recommended - say, for frequent asthma flares - your heart pays the price. Salmeterol (Serevent), the long-acting version, keeps your heart racing for 8-12 hours.
- Antibiotics: Azithromycin (Zithromax) is one of the biggest risks. A 2021 study of over 1.2 million patients found it increases the chance of rapid heartbeat by more than twice. Levofloxacin and ciprofloxacin also prolong the QT interval - the time your heart takes to recharge between beats. When that gets too long, it can trigger a life-threatening rhythm called torsades de pointes.
- Decongestants: Pseudoephedrine (Sudafed) and phenylephrine are in many cold and allergy meds. At standard doses, they can raise your heart rate by 10-20 beats per minute. If you have high blood pressure or heart disease, even one pill can be too much.
- Thyroid meds: Levothyroxine (Synthroid) is essential for many, but too much sends your heart into overdrive. When your TSH drops below 0.1 mIU/L, palpitations show up in 8-12% of users. That’s why regular blood tests aren’t optional - they’re lifesaving.
- Antidepressants: Tricyclics like amitriptyline can stretch the QT interval by 40-60 milliseconds. Even SSRIs like citalopram (Celexa) carry risk, especially at doses over 40 mg/day. Many people don’t know their depression meds could be affecting their heart.
- Newer weight-loss drugs: Semaglutide (Ozempic, Wegovy), once thought to be heart-safe, now shows up in reports as a cause of mild but consistent heart rate increases - 3-5 bpm on average. For someone already prone to palpitations, that’s enough to notice.
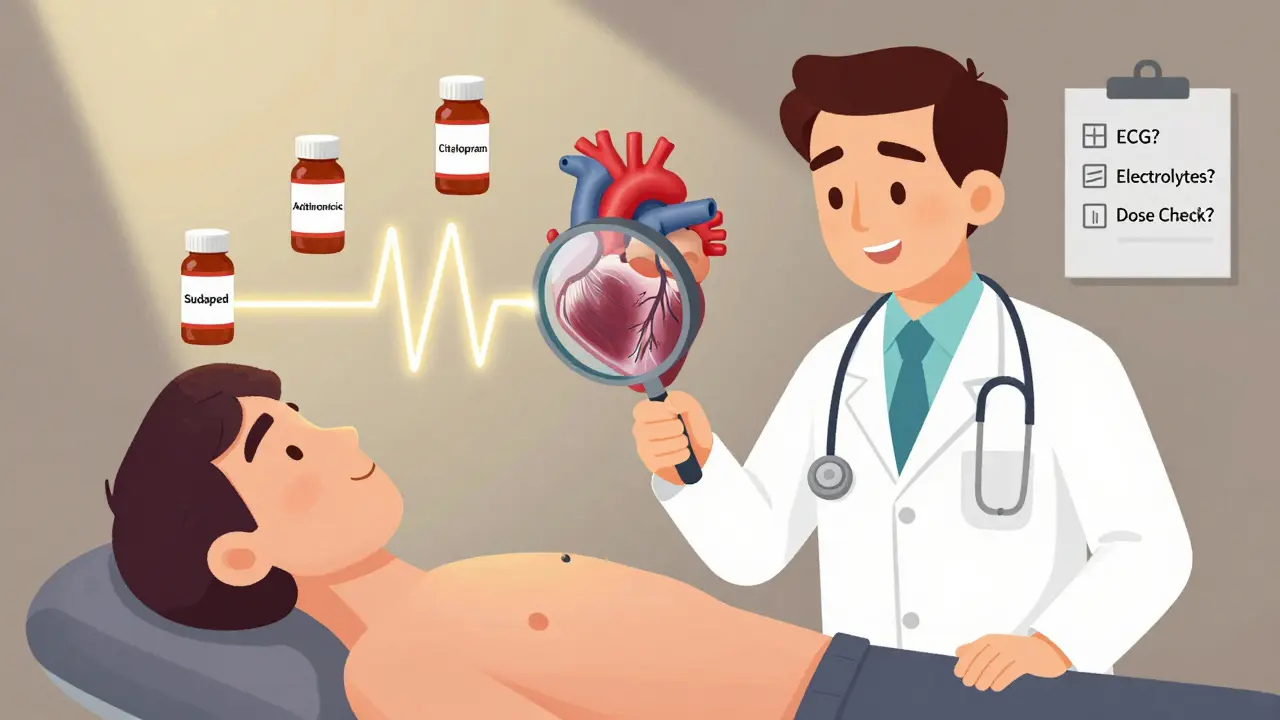
How Doctors Evaluate Medication-Induced Palpitations
If you’re having palpitations, your doctor shouldn’t just say, “It’s probably nothing.” They need to check for drug-related causes - and fast. Here’s what a real evaluation looks like:- Complete medication review: Every pill, supplement, and OTC drug you’ve taken in the last 72 hours. Why? Because 70% of drug-induced arrhythmias show up within three days of starting or changing a dose.
- ECG (electrocardiogram): This is non-negotiable. It measures your heart’s electrical activity. The key number? QTc interval. Normal is under 450ms for men, under 460ms for women. If it’s over 500ms - or jumps more than 60ms from your baseline - you’re at high risk.
- 24- to 48-hour Holter monitor: If your resting ECG looks fine but you still feel your heart racing, this portable device records your rhythm all day. It catches problems a single ECG misses in 35-45% of cases.
- Blood tests: Low potassium (<3.5 mmol/L) or low magnesium (<1.7 mg/dL) make your heart way more sensitive to bad drug effects. Thyroid levels (TSH) are checked too - especially if you’re on levothyroxine.
What to Do If a Medication Is Causing Your Palpitations
The good news? Most cases get better - once you know what’s causing it.- Mild cases: If your QTc is under 500ms and you’re not dizzy or passing out, your doctor might just keep you on the drug - but with tighter monitoring. Weekly ECGs. Better electrolytes. Maybe lower your dose.
- Modifying the dose: For many, cutting the dose by 25-50% stops the palpitations. One Mayo Clinic study found 60-70% of patients felt better within 72 hours of a dose change.
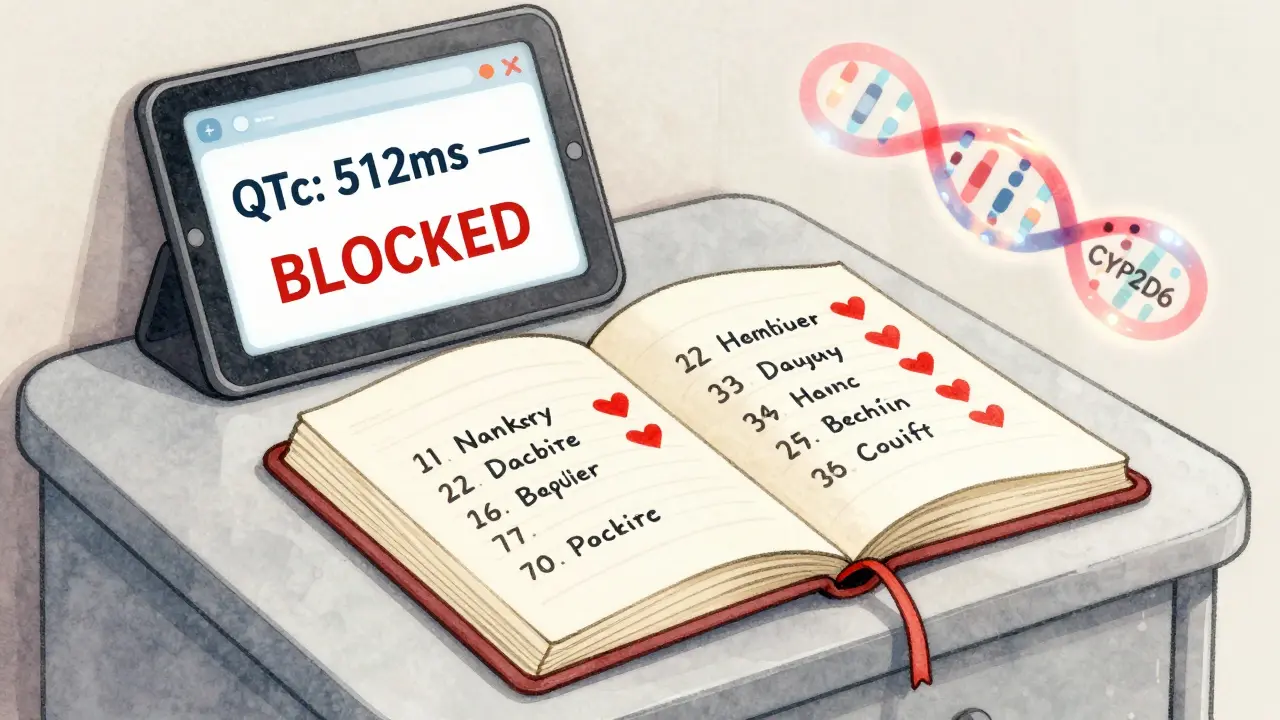
- Stopping the drug: If your QTc is over 500ms, you’ve had a dangerous rhythm, or you’re fainting - the drug must go. No exceptions. 95% of hospitals follow this rule.
- For antibiotics: Amoxicillin has a 0.8% risk of arrhythmia. Azithromycin? 2.9%. That’s nearly 4 times higher.
- For thyroid meds: If levothyroxine causes palpitations, don’t stop it - adjust it. Keeping TSH between 0.5 and 2.0 mIU/L drops palpitation rates from 12% to just 4.3%.
- For antidepressants: Switching from citalopram to sertraline (Zoloft) often resolves palpitations without losing mood control - as shown in patient case studies.
Prevention: The Best Way to Avoid Drug-Induced Heart Problems
The smartest move isn’t waiting until your heart starts racing. It’s preventing it before it starts.- Baseline ECG before starting high-risk drugs: The American Heart Association now recommends this for anyone starting azithromycin, fluoroquinolones, or certain antidepressants. It’s quick, cheap, and could save your life.
- Know your risk factors: If you’re over 75, female, have heart disease, or take more than one QT-prolonging drug - you’re in the danger zone. The risk of torsades de pointes is over three times higher in older adults.
- Use a symptom journal: Write down when you take your meds and when you feel your heart race. Do the two line up? That’s your clue. Dr. John Day, a leading heart rhythm specialist, says this simple habit helps patients spot patterns doctors miss.
- Combining two QT-prolonging drugs (risk jumps 5.7x)
- Giving high-dose ondansetron (Zofran) to someone with a long QT
- Using fluoroquinolones in people with heart failure
- Prescribing more than 40mg/day of citalopram to someone over 60
- Starting levothyroxine without an ECG if you have heart disease
Real Stories: What Patients Are Saying
On Reddit, one user wrote: “Started azithromycin for a sinus infection. Two days later, my chest felt like a bird was trapped inside. I thought I was having a panic attack - until my ECG showed prolonged QT.” Another on Patient.info: “I was on Synthroid for years. Then I started waking up with my heart pounding. My doctor said my TSH was 0.05. We lowered my dose. Within two weeks, it was gone.” And a cancer patient on a support forum: “My heart started fluttering during chemo infusions. At first, I thought it was anxiety. Turns out, it was trastuzumab. My oncologist added metoprolol. The palpitations stopped - and my treatment kept working.” These aren’t outliers. They’re patterns.What’s Changing in 2026
Technology is catching up. Most major hospitals now use electronic health records with built-in alerts. If your doctor tries to prescribe azithromycin and your QTc is over 480ms, the system blocks it - and pops up a warning. Epic Systems’ QTc Alert Module prevents over 8,500 risky prescriptions every month. In the next few years, genetic testing will play a bigger role. Some people are born with genes that make them extra sensitive to certain drugs. A CYP2D6 poor metabolizer, for example, has a 3.4 times higher risk of bad reactions to beta-blockers. Testing for these isn’t routine yet - but it’s coming. The European Heart Rhythm Association is tracking 50,000 patients across 15 countries to build better risk models. By late 2025, we’ll know even more about who’s most at risk - and how to protect them.You’re Not Alone - But You Need to Speak Up
Palpitations from meds are common. But they’re often ignored. Patients think it’s stress. Doctors think it’s anxiety. But the data doesn’t lie. If you’ve started a new drug and your heart feels off - don’t wait. Don’t assume it’ll pass. Ask your doctor: “Could this medication be causing my palpitations?” Bring a list of everything you take. Ask for an ECG. Check your potassium and magnesium. Ask if your dose is right. Your heart is listening. Make sure your meds aren’t shouting at it.Can over-the-counter cold meds cause palpitations?
Yes. Decongestants like pseudoephedrine (in Sudafed) and phenylephrine can raise your heart rate by 10-20 beats per minute. Even if you’re young and healthy, taking more than the recommended dose - or combining them with caffeine, alcohol, or other stimulants - can trigger palpitations. If you have high blood pressure, heart disease, or an irregular heartbeat, avoid them entirely.
How do I know if my palpitations are dangerous?
Danger signs include dizziness, fainting, chest pain, shortness of breath, or palpitations that last more than a few minutes. If your heart races suddenly after starting a new drug - especially if you’re over 65, female, or have heart disease - treat it as a warning. Don’t wait. Get an ECG. A QTc interval over 500ms or a rise of more than 60ms from your baseline means you’re at risk for a life-threatening rhythm.
Can I keep taking my medication if I have mild palpitations?
Maybe - but only under close supervision. If your QTc is under 500ms and you’re not dizzy or in pain, your doctor might keep you on the drug while lowering the dose or checking your electrolytes. But if you’re symptomatic, even mildly, stopping or switching is usually safer. Never ignore palpitations just because they’re “not bad yet.”
Are antidepressants safe for my heart?
Some are, some aren’t. Tricyclics like amitriptyline and SSRIs like citalopram (especially at doses over 40mg/day) can prolong the QT interval. Sertraline and escitalopram are generally safer. If you’re on an antidepressant and feel heart flutters, talk to your doctor. Switching meds doesn’t mean giving up on mental health treatment - it means finding one that’s safer for your heart.
What should I ask my doctor before starting a new medication?
Ask: “Can this drug cause heart rhythm problems?” “Do I need an ECG before starting?” “What’s my risk if I’m over 65 or have heart disease?” “Are there safer alternatives?” “Should I check my potassium or magnesium levels?” Don’t assume your doctor knows all the risks - many aren’t listed clearly on the label. Be your own advocate.




Man, I had no idea my Sudafed could make my heart feel like it was trying to escape my chest. Been popping those like candy during allergy season. Guess I’m switching to saline sprays now.
THIS. I thought I was having panic attacks-turns out my new Zithromax was turning my heart into a jackhammer. Got an ECG, they caught the QT prolongation. Saved my life. Don’t ignore your heartbeat. It’s talking.
So… we’re just blaming meds now? What about stress? Or caffeine? Or the fact that we’re all just wired too tight in 2025?
Medication-induced palpitations are a well-documented clinical phenomenon. The American Heart Association recommends a thorough medication reconciliation prior to diagnosing idiopathic arrhythmias. Always consult your provider before discontinuing any prescribed therapy.
Levothyroxine did this to me too-my heart was racing at 110 bpm at rest. My doctor didn’t check my TSH for 6 months. Don’t let them ignore you. Demand the labs. You’re not being dramatic-you’re being smart.
so like… i’ve been on ozempic for 4 months… and yeah… my heart feels… weird? not bad… just… different? like it’s humming? and i thought it was just… me? being anxious? but now i’m like… wait… is this… real? or am i just… overthinking? again?
Physiological responses to pharmacological agents are highly individualized. A population-level risk does not equate to individual harm. Clinical context is paramount.
My cardiologist told me to stop my albuterol inhaler because I was using it 8 times a day. I thought I was being responsible. Turns out I was basically giving my heart a daily caffeine IV. Now I use a spacer, limit it to 2 puffs max, and my heart stopped feeling like it was trying to break out of my ribs. Also, I’m not dying. I’m just… careful now.
Y’all need to stop blaming meds and start blaming the system. Pharma companies don’t tell you this stuff because they make billions off you getting heart issues and then needing more pills. It’s a loop. Break the cycle. Ask for alternatives. Don’t just swallow what they give you.
In Nigeria, many people use antibiotics without prescriptions. I’ve seen friends with fever take azithromycin daily for weeks. No monitoring. No ECG. It’s terrifying. This post should be translated and shared everywhere.
If you’re experiencing palpitations, please don’t panic-but please don’t ignore it either. Your heart is a muscle that deserves respect. Talk to your doctor. Get tested. You’re worth the time it takes to be safe.
The QTc interval is the critical metric for assessing drug-induced torsadogenic risk. Prolongation beyond 500 ms warrants immediate discontinuation and electrolyte repletion. ECG monitoring is standard of care for high-risk agents.
People blame drugs. But if you’re taking 12 different pills and your heart races, maybe you’re the problem. Stop self-medicating. Stop popping OTC stuff like candy. Your body isn’t a lab experiment.
Thank you for sharing this. I’ve had palpitations for years and assumed it was anxiety. After reading this, I asked my doctor to check my QT interval. It was 498 ms. We switched my citalopram. My heart hasn’t felt like that since. This information saved me.