 9
May,2023
9
May,2023
Understanding Mycosis Fungoides
Mycosis Fungoides (MF) is a rare type of cutaneous T-cell lymphoma that affects the skin. It is a slow-growing cancer that can cause scaly, red patches, plaques, and tumors on the skin. As someone living with Mycosis Fungoides, I know firsthand how important it is to find the most effective treatment options. In this article, we will discuss different treatment options available for managing MF and improving the quality of life for patients.
Topical Treatments for Mycosis Fungoides
Topical treatments are often the first line of defense for MF, as they are applied directly to the affected skin areas. There are several topical medications that can help control symptoms and slow the progression of MF.
Corticosteroids
Topical corticosteroids are often prescribed to reduce inflammation and itching associated with MF. These medications can help control symptoms and improve the appearance of the skin. However, long-term use of corticosteroids can cause side effects such as thinning of the skin, so it is essential to follow your healthcare provider's recommendations closely.
Topical Chemotherapy
Topical chemotherapy, such as carmustine or mechlorethamine, can be applied directly to the skin to target MF cells. These treatments can help control the progression of the disease and reduce symptoms. However, they can also cause irritation and redness, so it is crucial to monitor your skin's reaction and work closely with your healthcare provider during treatment.
Phototherapy for Mycosis Fungoides
Phototherapy involves using ultraviolet (UV) light to treat the skin affected by MF. There are two main types of phototherapy: narrowband UVB and PUVA (psoralen plus UVA).
Narrowband UVB
Narrowband UVB phototherapy uses a specific wavelength of UVB light to treat the skin. This treatment is usually well-tolerated and can help reduce symptoms and improve the appearance of the skin. It is typically administered two to three times per week for several weeks or until the skin improves.
PUVA
PUVA therapy involves taking a medication called psoralen, which makes the skin more sensitive to UVA light. The affected skin is then exposed to UVA light, which penetrates deeper into the skin than UVB light. This treatment can be effective in controlling MF symptoms and may help induce long-term remission. However, it is essential to protect your skin from the sun during PUVA therapy, as the increased sensitivity to UVA light can increase the risk of sunburn and skin damage.
Systemic Treatments for Mycosis Fungoides
Systemic treatments are medications that work throughout the body to target MF cells. These treatments are usually reserved for more advanced cases or when topical treatments and phototherapy have not been effective.
Oral Medications
Oral medications, such as bexarotene or interferon-alpha, can help control the growth and spread of MF cells. These medications can be effective in treating MF, but they can also cause side effects such as fatigue, nausea, and liver problems. It is important to discuss the potential risks and benefits of these treatments with your healthcare provider before starting therapy.
Chemotherapy
Systemic chemotherapy may be used to treat advanced MF or when other treatments have not been effective. Chemotherapy drugs can help kill MF cells, but they can also cause side effects such as hair loss, nausea, and fatigue. Your healthcare provider will carefully consider the potential benefits and risks of chemotherapy before recommending this treatment.
Targeted Therapies for Mycosis Fungoides
Targeted therapies are medications that specifically target MF cells while sparing healthy cells. These treatments can be an effective option for managing MF, especially in advanced cases or when other treatments have not been successful.
Brentuximab Vedotin
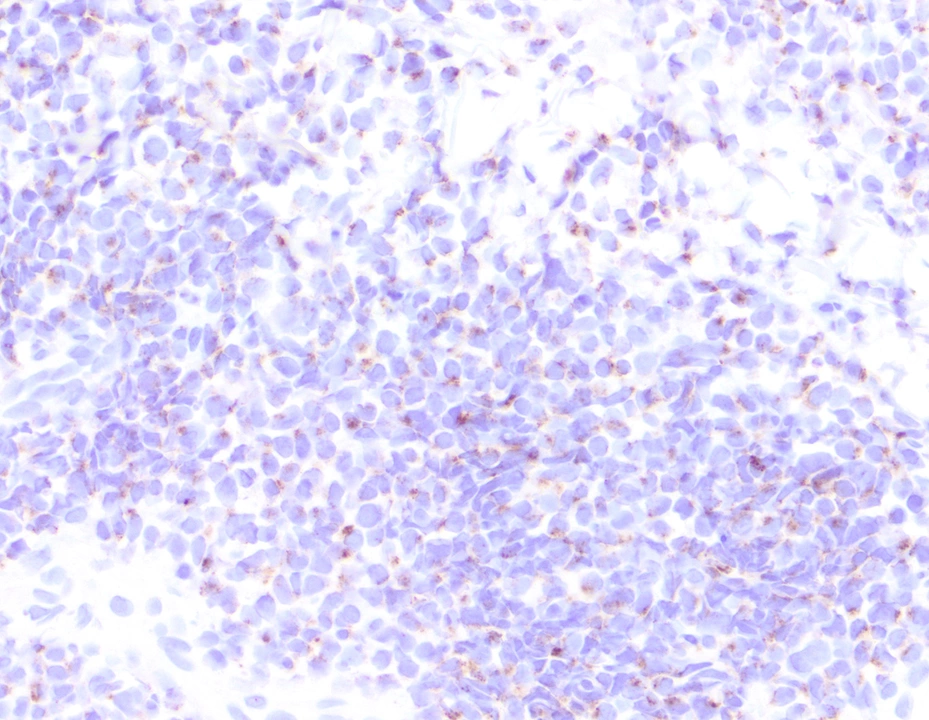
Brentuximab vedotin is a targeted therapy that works by attaching to a protein called CD30 on the surface of MF cells. This allows the medication to be delivered directly to the cancer cells, where it can help kill them. Brentuximab vedotin can be an effective treatment for some patients with MF, but it can also cause side effects such as nerve damage, so it is essential to work closely with your healthcare provider during treatment.
Mogamulizumab
Mogamulizumab is another targeted therapy that binds to a protein called CCR4 on the surface of MF cells. This medication can help control the growth and spread of MF cells and may be an effective treatment option for some patients. However, it can also cause side effects such as infusion reactions and skin rash, so it is crucial to discuss the potential risks and benefits of this treatment with your healthcare provider.
Conclusion
Treatment options for Mycosis Fungoides have come a long way, with various therapies available to help manage symptoms and slow the progression of the disease. It is essential to work closely with your healthcare provider to determine the best treatment plan for your individual needs. By staying informed and proactive about your treatment options, you can take control of your health and improve your quality of life while living with Mycosis Fungoides.






Honestly, the article seems to skim the surface while pretending depth. The author throws in buzzwords like "targeted therapies" without mentioning how accessibility and cost shape patient outcomes. It feels like a marketing brochure rather than a balanced overview. Also, where's the discussion on the long-term psychological impact of chronic skin lesions? A more critical look at real-world data would have been appreciated.
One must consider the hidden agendas behind the promotion of phototherapy. Industry-sponsored studies often downplay the carcinogenic potential of UVA exposure, a fact conveniently omitted in this piece. It is incumbent upon the discerning reader to scrutinize the funding sources of cited research, lest we become unwitting pawns in a larger biomedical conspiracy.
Good overview.
From a mechanistic standpoint, Mycosis Fungoides epitomizes the paradox of cutaneous immunosurveillance gone awry. The dysregulated T‑cell homing signals intersect with epithelial cytokine milieus, fostering a niche where malignant clones thrive. Thus, topical agents merely act as surface-level modulators, while systemic interventions aim at the clonal architecture. Phototherapy, in this schema, serves as a photonic reset, inducing apoptosis via DNA cross‑linking. Nevertheless, the therapeutic horizon now expands with antibody‑drug conjugates that exploit CD30 expression, heralding a shift toward precision oncology. In sum, a layered approach-integrating skin‑directed and systemic modalities-optimally mitigates disease burden.
I totally get where you're coming from, it's kinda crazy how the skin and immune system talk to each other. Some patients really feel relief when they get topical stuff, but yeah, you need to watch for side effects. Also, don’t forget to keep an open dialog with your doc, they can help you weigh the pros and cons. It's all about finding that sweet spot for you.
Wow, another fluff piece. Like, sure, UV light is cool, but have you ever thought about how many skin cancers we’re spawning? And hey, if you love spending hours under a lamp, go ahead-just don’t blame us when the insurance rejects your claim.
It is imperative to recognize that the pharmaceutical narratives surrounding Brentuximab Vedotin and Mogamulizumab are meticulously curated. The hidden data on long‑term neurotoxicity and infusion‑related adverse events are often buried beneath glossy press releases. Moreover, the regulatory approvals were expedited under emergency provisions, raising questions about the rigor of underlying trials. One must remain vigilant, lest we accept half‑truths as medical doctrine.
First of all, I want to thank the author for compiling such a comprehensive overview of Mycosis Fungoides treatments. The breakdown of topical, phototherapy, systemic, and targeted therapies is clear and helpful for patients navigating this complex landscape. It’s crucial to emphasize that each treatment modality carries its own risk‑benefit profile, and shared decision‑making with a dermatologist or oncologist is essential. For instance, while topical steroids are effective for early lesions, long‑term use can lead to skin atrophy, so clinicians often rotate to calcineurin inhibitors or consider low‑dose phototherapy. Speaking of phototherapy, the distinction between narrowband UVB and PUVA is well captured; however, patients should be made aware of the cumulative UV exposure and the need for photoprotection post‑treatment. Systemic options such as bexarotene and interferon‑alpha have proven efficacy but require monitoring of liver function and lipid panels. Chemotherapy remains a last‑line option due to its systemic toxicity, yet novel agents like brentuximab vedotin have shown promising results in CD30‑positive disease. Targeted therapies, particularly mogamulizumab, offer a more tailored approach but come with infusion‑related reactions that must be managed proactively. Importantly, the psychosocial impact of chronic skin disease cannot be overstated; incorporating supportive care and counseling can improve quality of life. I also appreciate the article’s call for individualized treatment plans, as disease stage, comorbidities, and patient preferences all influence therapeutic choices. In summary, staying informed about emerging therapies and maintaining open communication with the care team empowers patients to make the best possible decisions for their health.
i wish i could find a treatment that actually works without making me feel like i’m on a chemo bus lol
Sure, because reading a Wikipedia‑style article totally solves decades of clinical research… 🙄
Wow, the author really missed the chance to discuss the epistemic void behind “targeted” drugs 😏. When you peel back the glossy veneer, you see that most of these agents were fast‑tracked after secretive Phase I trials, data that never saw the light of day. The real question is not “how effective are they?” but “who profits from the hype?” 🤔 Keep your eyes open, folks!
Great points on individualizing therapy! I think it’s also worth noting that patient support groups can share real‑world tips about managing side effects, which isn’t covered in most clinical write‑ups. Staying connected can make a huge difference in adherence and overall morale.