 1
Jan,2026
1
Jan,2026
After a colonoscopy finds polyps, many people assume they’ll need another one in five years. But that’s not always true. The right time for your next colonoscopy depends on the type, size, number, and shape of the polyps removed - not a one-size-fits-all timeline. In fact, some people may wait up to 10 years. Others need to return in just 3 months. Getting this wrong can mean missing early cancer or getting unnecessary procedures. Here’s what actually matters.
What Kind of Polyp Was Removed?
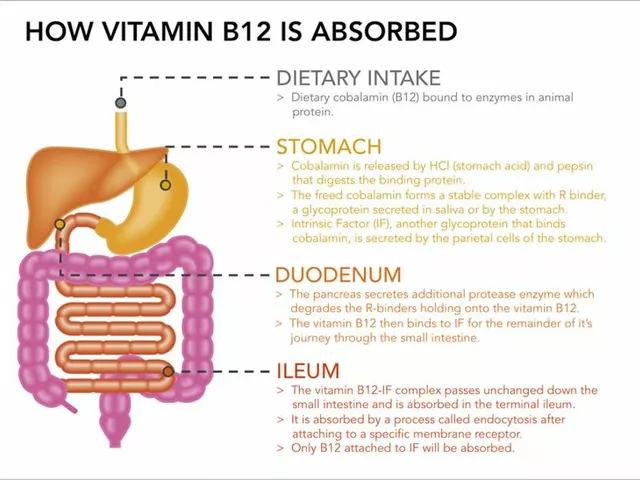
Not all polyps are the same. The biggest factor in deciding when to return is the pathology report. There are three main types that matter: adenomas, serrated polyps, and hyperplastic polyps.
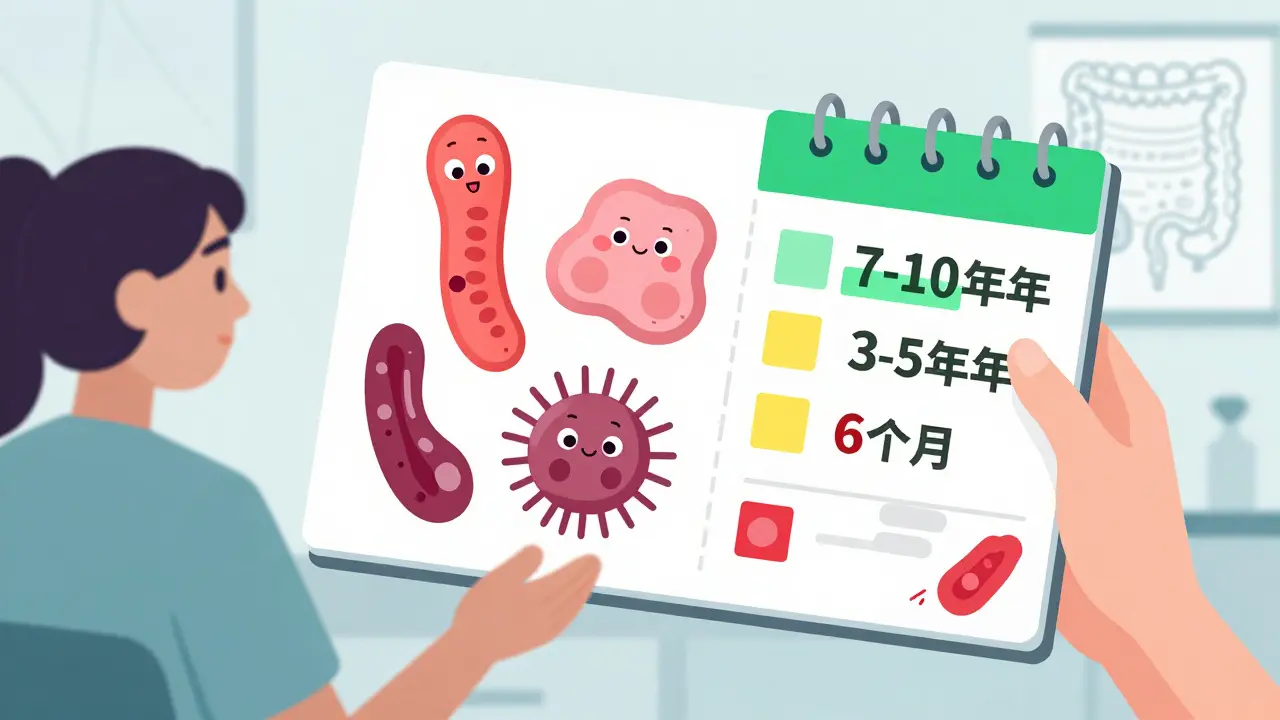
Adenomas are the most common precancerous polyps. If your report says "tubular adenoma" or "tubulovillous adenoma," that’s a red flag. But size and number matter more than the label. A 5-mm adenoma is very different from a 15-mm one. The 2020 US Multi-Society Task Force guidelines updated intervals based on real-world cancer data. For one or two adenomas under 10 mm, you now wait 7 to 10 years - not 5. That’s because studies show people with these small polyps have nearly the same cancer risk as those with no polyps at all.
Serrated polyps are trickier. There are two kinds: sessile serrated lesions (SSLs) and traditional serrated adenomas (TSAs). SSLs are especially concerning because they can turn cancerous quietly, without looking like typical polyps. If you have one or two SSLs under 10 mm, your next colonoscopy is due in 5 to 10 years. If you have three to four, you come back in 3 to 5 years. Five or more? Back in 3 years. The key here is that size matters less than the number. Even small SSLs add up in risk.
Hyperplastic polyps are usually harmless - unless they’re bigger than 10 mm. If you have one large hyperplastic polyp, your doctor will likely recommend a repeat colonoscopy in 3 to 5 years. Why? Because it’s hard to tell the difference between a large hyperplastic polyp and an SSL without expert review. Better safe than sorry.
Size and Number Change Everything
Two small adenomas? Wait 7 to 10 years. Three or four? That’s a 3 to 5 year window. Five or more? Back in 3 years. This isn’t arbitrary. Data from over 1.2 million colonoscopies shows that the risk of developing cancer jumps sharply after four adenomas, even if they’re all under 10 mm.
Size matters too. Any adenoma 10 mm or larger - even just one - pushes you into the high-risk group. Same goes for any polyp with villous features or high-grade dysplasia. These are signs the cells are changing fast. You’ll need a follow-up in 3 years, no exceptions. And if the polyp was removed in pieces (piecemeal resection), especially if it was over 20 mm, you’re coming back in 6 months. Why? Because leftover tissue can grow back unnoticed.
Here’s what a typical case looks like: A 58-year-old woman has a 6-mm tubular adenoma removed. No other polyps. Her report says complete resection, good bowel prep. She doesn’t need another colonoscopy until she’s 65. That’s 7 years. But if she had two 8-mm adenomas, she’d still wait 7 to 10 years. If she had three, she’d come back in 4 years. If she had one 12-mm adenoma? Back in 3 years. The difference isn’t just timing - it’s peace of mind.
What About Sessile Serrated Lesions (SSLs)?
SSLs are the silent threat. They don’t look scary. They’re flat, pale, and often hidden in the right side of the colon. That’s why they’re missed in up to 25% of colonoscopies. But once they’re found, they demand attention.
If you have one or two SSLs under 10 mm and no other risk factors, your next colonoscopy is due in 5 to 10 years. That’s the same as low-risk adenomas. But if you have three to four, it drops to 3 to 5 years. Five or more? 3 years. And if any SSL is 10 mm or larger? You’re in the 3-year group, no matter what.
Here’s where confusion happens: Many doctors still treat SSLs like regular adenomas. But the data doesn’t support that. A 2023 study in Endoscopy International Open found only 52% of US gastroenterologists correctly applied the 5-10 year interval for small SSLs. That means nearly half of patients were either over-treated or under-treated. If your doctor says “come back in 5 years” after finding one small SSL, they’re likely right. But if they say “come back in 3,” ask why.
What If the Polyp Wasn’t Fully Removed?
Polyp removal isn’t always clean. Sometimes, especially with large or flat polyps, the endoscopist has to remove it in pieces. That’s called piecemeal resection. And it’s a problem.
When a polyp over 20 mm is removed in pieces, leftover cells can regrow. The 2020 US guidelines say: come back in 6 months. So do the Japanese and Korean guidelines. But in Europe, the recommendation is a range: 3 to 6 months. Why the difference? European data shows most recurrences happen within 6 months, so they prefer a tighter window. The US standard is fixed at 6 months - simple, clear, and backed by evidence.
If you had a 25-mm polyp removed in pieces, don’t wait. Schedule your next colonoscopy for 6 months out. And make sure your doctor documents the resection type. If they don’t, ask for a copy of the report. This isn’t a suggestion - it’s a safety step.

What Is Serrated Polyposis Syndrome?
This is rare - affecting less than 1% of people who get colonoscopies - but it’s serious. If you have 20 or more serrated polyps total, with at least five being 5 mm or larger, you have serrated polyposis syndrome (SPS). This isn’t just about surveillance. It’s about lifelong monitoring.
The British guidelines say: annual colonoscopy until age 75. The Japanese guidelines say: every year, no exceptions. The US guidelines are more flexible: start with yearly, then extend to every 2 years if no large polyps are found. Why the variation? Because SPS carries a 70% lifetime risk of colorectal cancer. You can’t afford to wait.
If you’ve been diagnosed with SPS, don’t delay. Your next colonoscopy should be in 1 year. If your doctor says “wait 2 years,” push back. Ask for the evidence. This isn’t a routine check-up - it’s cancer prevention.
Why Do So Many People Get Colonoscopies Too Soon?
Despite clear guidelines, most people still get repeat colonoscopies every 5 years - even when they don’t need to. A 2020 study at a Veterans Affairs hospital found that only 18.6% of doctors followed the updated 7-10 year rule for low-risk adenomas. Eighty-one percent stuck with the old 5-year rule.
Why? Fear. Fear of missing something. Fear of lawsuits. Fear of patients complaining. A 2021 study by Dr. Douglas Rex found that 18.6% of US gastroenterologists who knew the new guidelines still recommended 5-year intervals. They knew better - but didn’t act.
Patients also contribute. After hearing “you have polyps,” many assume they’re at high risk. They call their doctor and demand a repeat colonoscopy in 5 years. Doctors, wanting to reassure, often comply - even if it’s not needed. This leads to overuse. The US spends $2.3 billion a year on colonoscopies. Up to 40% of those are unnecessary because of outdated intervals.
Here’s the truth: Waiting 7 to 10 years for low-risk polyps doesn’t increase cancer risk. It reduces unnecessary procedures, lowers costs, and avoids complications from repeat sedation. But only if the guidelines are followed.
What Tools Help Doctors Get This Right?
Guidelines are complex. A doctor sees 20 patients a day. They can’t memorize every rule. That’s why tools like Polyp.app exist. Developed by gastroenterologists at Massachusetts General Hospital, this free app lets doctors enter polyp details and instantly get the recommended interval.
As of 2023, over 12,400 clinicians use it. Many hospitals now have EHR integrations - Epic and Cerner systems automatically suggest intervals based on what’s documented in the procedure note. But not all systems are updated. If your doctor uses an older system, they might still be using 2012 guidelines.
Ask: “Is your recommendation based on the 2020 US Multi-Society Task Force guidelines?” If they look confused, ask for a copy of your pathology report and the follow-up recommendation in writing. You have the right to know why they’re telling you to come back when they do.

What’s Coming Next?
The future of colonoscopy surveillance isn’t just about counting polyps. Researchers are testing blood and stool tests that detect DNA changes linked to cancer risk. Trials are underway to see if molecular markers can replace the current system. Imagine a test that says: “Your risk is low - wait 10 years.” Or: “Your risk is high - come back in 2.”
Dr. Samir Gupta, a lead author of the 2020 guidelines, says we’re moving toward personalized intervals based on biology, not just size and number. That’s coming. But it’s not here yet. For now, polyp characteristics are still the gold standard.
Meanwhile, the European Society of Gastrointestinal Endoscopy plans to update its guidelines in late 2024. They may shorten intervals for certain SSL subtypes. The science keeps evolving. So should your understanding.
What Should You Do Now?
After your colonoscopy, get your pathology report. Don’t wait for your doctor to call. Look for these key phrases:
- Type: adenoma, SSL, hyperplastic
- Number: 1, 2, 3, 5+
- Size: under 10 mm, 10 mm or larger
- Resection: complete or piecemeal
Then match it to the rules:
- 1-2 adenomas ≤10 mm → 7-10 years
- 3-4 adenomas <10 mm → 3-5 years
- 5-10 adenomas → 3 years
- Any adenoma ≥10 mm → 3 years
- 1-2 SSLs <10 mm → 5-10 years
- 3-4 SSLs → 3-5 years
- 5+ SSLs → 3 years
- SSL ≥10 mm → 3 years
- Large hyperplastic polyp ≥10 mm → 3-5 years
- Piecemeal resection of polyp ≥20 mm → 6 months
- Serrated polyposis syndrome → annual until age 75
If your doctor recommends a different timeline, ask why. Show them your report. Ask if they’re using the 2020 US guidelines. If they’re not, consider getting a second opinion. Your next colonoscopy should be based on science - not habit.
How soon should I get my next colonoscopy if I had one small adenoma?
If you had one adenoma under 10 mm and no other polyps, you should wait 7 to 10 years. This is based on the 2020 US Multi-Society Task Force guidelines, which show that cancer risk is nearly the same as someone with a normal colonoscopy. Many doctors still say 5 years, but that’s outdated. Ask for your pathology report and confirm the polyp size and type.
Do serrated polyps need more frequent follow-up than regular adenomas?
It depends. Small sessile serrated lesions (SSLs) under 10 mm follow the same 5-10 year rule as small adenomas. But if you have three or more SSLs, even if they’re small, you need a colonoscopy in 3 to 5 years. Five or more? 3 years. SSLs are harder to detect and can turn cancerous faster than adenomas, so number matters more than size.
What if my polyp was removed in pieces?
If a polyp larger than 20 mm was removed in pieces, you need a repeat colonoscopy in 6 months. This is because leftover tissue can regrow. The 2020 US guidelines and most international experts agree on this. Don’t wait - schedule it early. Your doctor should note "piecemeal resection" in the report. If they don’t, ask for clarification.
Can I skip my next colonoscopy if I feel fine?
No. Colorectal cancer often has no symptoms until it’s advanced. Polyps grow slowly, but they don’t disappear. Even if you feel perfectly healthy, skipping your scheduled colonoscopy based on how you feel puts you at risk. The goal of surveillance is to catch changes before they become cancer - not after.
Are there alternatives to colonoscopy for surveillance?
For people who’ve had polyps removed, colonoscopy is still the only recommended surveillance tool. Stool tests like FIT or Cologuard can screen for cancer in average-risk people, but they can’t detect new polyps or confirm if a previous one was fully removed. If you’ve had polyps, you need a colonoscopy to visually inspect and remove any new growths.
Final Thought: Don’t Let Fear Drive Your Schedule
Having polyps doesn’t mean you’re doomed. Most are harmless. Most cancers take 10 to 15 years to develop. The goal isn’t to chase every cell - it’s to catch the dangerous ones early. Following the right interval means you’re doing everything right: you’re preventing cancer without overdoing it. Get your report. Know your numbers. Ask questions. And trust the science - not the habit.




Wow, this is actually one of the clearest explanations I’ve ever seen-thank you. I had two small adenomas last year, and my doctor said ‘5 years,’ but now I’m going to ask for the 2020 guidelines. I’ve been stressing over this for months. 😅
THEY’RE LYING TO YOU. EVERY SINGLE ONE OF THEM. The pharmaceutical companies own the guidelines. They want you coming back every 5 years so you keep buying those $2000 prep kits and sedatives. And don’t even get me started on the colonoscopy machines-those things cost $1.2 million, and hospitals make a killing off repeat visits. They don’t care if you’re low risk-they care about profit. I read a whistleblower report from 2021 that got buried. The real cancer risk for small adenomas? Near zero. But they’ll scare you into another procedure. You’re being exploited. 🤫💊
Life doesn’t come with a manual-but this? This is the closest thing to a map for your insides. 🌱 I used to think polyps were just… lumps. Turns out they’re whispers from your body, screaming in a language only doctors half-hear. I’m printing this out. My mom’s next colonoscopy is in two weeks. I’m handing her this like a survival guide. Thank you for turning fear into clarity. You didn’t just write an article-you gave people back their peace.
Ugh, I hate how people treat colonoscopies like a spa day. ‘Oh, I’ll just go every five years, it’s fine.’ No. It’s not fine. You need to know the difference between an SSL and a hyperplastic polyp like it’s your job-because your life depends on it. If your doctor doesn’t quote the 2020 guidelines verbatim, they’re not doing their job. I’ve seen too many people get complacent. This isn’t a checklist. It’s your body’s last warning before it screams. And you? You owe it to yourself to read the fine print.
As a gastroenterology researcher, I’m appalled that 81% of clinicians still use outdated intervals. The 2020 US Multi-Society Task Force guidelines were peer-reviewed, evidence-based, and statistically robust-yet they’re being ignored in favor of institutional inertia and liability aversion. The $2.3 billion annual spend on unnecessary colonoscopies? That’s not just waste-it’s medical malpractice by omission. Patients deserve precision, not platitudes. If your provider can’t articulate the difference between tubulovillous adenoma and sessile serrated lesion, find someone who can. Your colon is not a suggestion box.
Okay, so if I had one 8mm adenoma and one 5mm SSL, do I go by the adenoma rule (7-10 years) or the SSL rule (5-10)? Or do they stack? I’ve been reading this article three times and I still feel like I’m missing the math. Anyone know if the guidelines specify how to combine different polyp types? Like… is it max interval? Or worst-case scenario? Asking for a friend who’s currently Googling polyp types at 2 a.m. 🤓
My doctor just told me to come back in 5 years after finding two small adenomas. I printed this article and handed it to him. He paused, looked at the screen, and said, ‘Huh. I didn’t realize the guidelines changed.’ He then updated my chart. So… maybe not everyone’s clueless. But why does it take a patient to educate their own doctor? 🤷♀️
Thank you for writing this. In my country, most people don’t even know what a polyp is. We wait until we bleed. This information could save lives where resources are scarce. I’ve shared it with my community group. Simple words. Clear rules. No fear. Just facts. 🙏
So let me get this straight… the system is so broken that patients have to become amateur pathologists just to get basic care? And the doctors who *do* follow guidelines? They’re the exception, not the rule? Wow. I’m not even mad. I’m just… impressed by how efficiently we’ve turned prevention into a lottery. 🎲