 24
Jan,2026
24
Jan,2026
When your liver gets scarred, it doesn’t heal the way your skin does. Instead of fixing itself, it builds tough, fibrous tissue that blocks blood flow and stops it from doing its job. This isn’t just damage-it’s cirrhosis, the end stage of long-term liver disease. And once it sets in, the damage is mostly permanent. You might not feel anything at first. That’s the danger. By the time symptoms show up, your liver is already struggling. But knowing what’s happening can save your life-or someone else’s.
What Cirrhosis Really Means
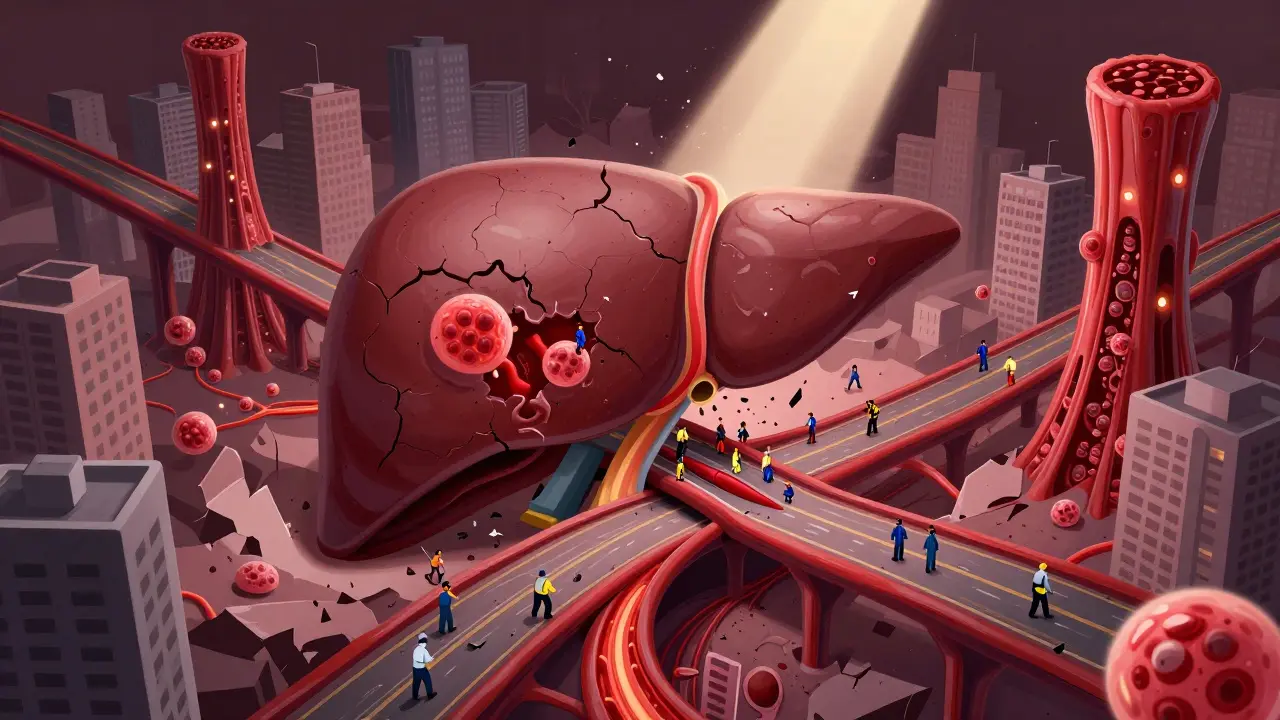
Cirrhosis isn’t a disease on its own. It’s the result of years of injury. Every time your liver gets damaged-by alcohol, hepatitis, fat buildup, or something else-it tries to repair itself. But if the damage keeps coming, the repair process goes wrong. Healthy liver cells get replaced by scar tissue. This scar tissue doesn’t help. It doesn’t filter toxins, make proteins, or store energy. It just sits there, stiff and useless, squeezing blood vessels and messing up the liver’s structure. The liver is one of the few organs that can regenerate. But cirrhosis breaks that ability. The scar tissue forms thick bands called septa, and around them, the liver tries to regrow in lumpy nodules. These nodules look like islands in a sea of scar. Under a microscope, it’s clear: this isn’t healing. It’s collapse. Doctors divide cirrhosis into two stages: compensated and decompensated. In compensated cirrhosis, the liver is scarred, but it’s still doing enough to keep you alive. You might feel tired, but you can still work, cook, and walk the dog. In decompensated cirrhosis, the liver can’t keep up. Fluid builds up in your belly. Your brain gets foggy. You start bleeding easily. That’s when things get serious.How Do You Know If You Have It?
Many people don’t know they have cirrhosis until it’s advanced. Routine blood tests often catch it first. High liver enzymes, low platelets, high bilirubin, low albumin-these are red flags. A simple ultrasound can show a shrunken, bumpy liver. But the real game-changer is elastography. This test measures how stiff your liver is. A reading over 12.5 kPa almost always means cirrhosis. No biopsy needed. But symptoms don’t always match the numbers. One patient I read about found out she had cirrhosis after a routine check-up. She had no pain, no jaundice, no swelling. Just elevated enzymes. Her liver was already 70% scarred from untreated hepatitis C. That’s the quiet killer. Common signs include:- Constant fatigue-even after a full night’s sleep
- Swelling in the legs or belly (ascites)
- Yellow skin or eyes (jaundice)
- Easy bruising or bleeding
- Confusion, forgetfulness, or slurred speech (hepatic encephalopathy)
- Itchy skin
- Loss of appetite and weight loss
Why Cirrhosis Leads to Liver Failure
The liver does over 500 jobs. It cleans your blood. It makes clotting factors. It turns food into energy. It stores vitamins. It breaks down drugs. When cirrhosis takes over, these jobs stop one by one. Portal hypertension is the big problem. Scar tissue squeezes the portal vein-the main blood vessel bringing blood from your gut to your liver. Blood backs up. Pressure rises. That’s when fluid leaks into your belly. That’s when veins in your esophagus swell and can burst. That’s when your spleen gets huge and swallows up your platelets. Your body can’t make enough albumin, so fluid pools. Your blood doesn’t clot right. Toxins like ammonia build up because your liver can’t filter them. That’s when confusion sets in. That’s hepatic encephalopathy. It can be mild-just forgetting your keys-or severe, leading to coma. The Model for End-Stage Liver Disease (MELD) score tells doctors how urgent your case is. It’s based on three blood tests: bilirubin, creatinine, and INR. The higher the score, the worse your liver is doing. A score above 15 means your chance of dying within a year without a transplant is over 50%. A score above 25? It’s nearly 80%.
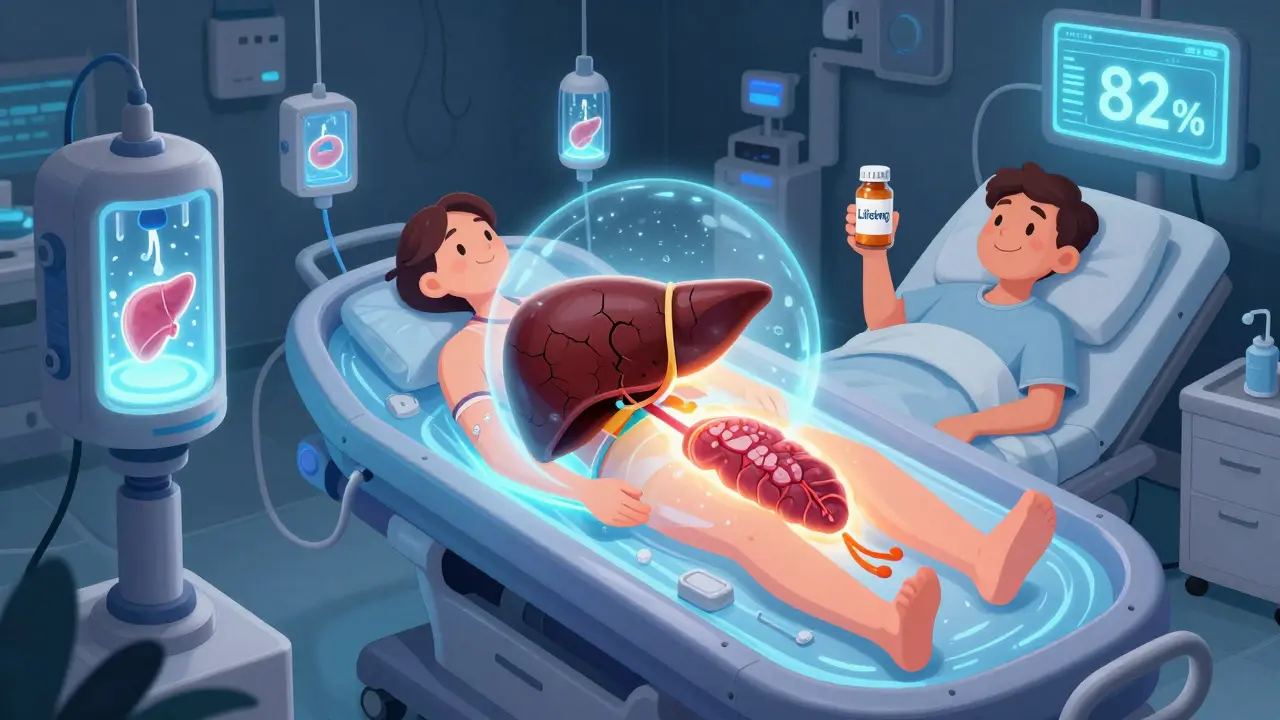
Transplantation: The Only Real Cure
There’s no pill that reverses cirrhosis. No supplement. No herb. No miracle diet. The only thing that can truly replace a failing liver is a transplant. In the U.S., cirrhosis is the top reason for liver transplants-about 40% of all cases. But there’s a brutal shortage. In 2022, over 14,300 people were on the waiting list. Only 8,780 transplants happened. That means about 12% of people on the list die each year waiting. The good news? Transplant success rates are high. Over 80% of patients survive at least five years. Many go back to work, travel, even have kids. But it’s not simple. You need to be healthy enough to survive surgery. You need to stop drinking. You need to prove you’ll take your meds every day. And you need to be on the list before your body breaks down too far. New tech is helping. Machines that keep donor livers alive outside the body-called normothermic perfusion-are making more organs usable. One 2023 study showed a 22% increase in transplantable livers. That’s life-saving progress. But even with a transplant, you’re not done. You’ll take anti-rejection drugs for life. You’ll need regular blood tests. You’ll be at higher risk for infections and some cancers. But for most, it’s a second chance.What You Can Do-Before It’s Too Late
The best way to avoid cirrhosis is to stop the damage before it starts. If you have fatty liver from obesity or diabetes, lose weight. Even 5-10% of your body weight can reverse early scarring. If you drink alcohol, cut it out. No safe level exists once liver damage begins. If you have hepatitis B or C, get treated. New antivirals can cure hepatitis C in 8-12 weeks with over 95% success. If you already have cirrhosis, your job is to stop it from getting worse. That means:- Zero alcohol
- Sodium under 2,000 mg a day (no processed food, no salt shaker)
- Protein in moderation (too much can trigger brain fog)
- Vaccines for hepatitis A and B, flu, and pneumonia
- Regular blood tests and imaging
- Medications like beta-blockers to lower portal pressure
- Spironolactone or furosemide to reduce belly fluid
What’s Coming Next
Science is racing to find new treatments. Right now, there are over 50 drugs in clinical trials targeting liver scarring. One, called simtuzumab, showed a 30% slowdown in fibrosis progression in patients with fatty liver disease. Another, obeticholic acid, is already approved for certain types of cirrhosis. The future may not be about transplants. Researchers are testing lab-grown liver cells and bioartificial livers-devices that can temporarily take over liver function while the real one heals. Early trials show patients’ MELD scores dropping by 40% after just six months of cell therapy. But here’s the hard truth: none of this replaces early detection. The sooner you know your liver is in trouble, the more you can do. A simple blood test, an ultrasound, a fibroscan-these can catch cirrhosis before you feel a thing.Frequently Asked Questions
Can cirrhosis be reversed?
In the early stages, before extensive scarring sets in, yes-sometimes. If you stop drinking, cure hepatitis C, or lose weight with fatty liver disease, the liver can repair some of the damage. But once cirrhosis is fully developed, the scar tissue is permanent. The goal then is to stop it from getting worse and prevent complications.
What’s the difference between cirrhosis and liver failure?
Cirrhosis is the long-term scarring of the liver. Liver failure happens when the organ can no longer function. Cirrhosis often leads to liver failure, but not all liver failure comes from cirrhosis. Acute liver failure can happen suddenly in a healthy liver due to overdose or poisoning. Cirrhosis is slow, silent, and progressive.
How long can you live with cirrhosis?
It depends. With compensated cirrhosis, many live 10-15 years or more if they manage their condition. Once it becomes decompensated, survival drops sharply-only 20-50% live five years without a transplant. The MELD score gives a clearer picture: a score of 20 means about a 50% chance of dying within a year.
Can you drink alcohol with cirrhosis?
No. Any amount of alcohol can speed up liver damage and push you into liver failure faster. Even small amounts are dangerous. Abstinence is the only safe choice.
How do you get on the liver transplant list?
You need a referral from your doctor to a transplant center. They’ll run tests to check your overall health, mental readiness, and support system. You’ll need to prove you’ve stopped drinking or using drugs. Once approved, your MELD score determines your place on the list. Higher scores mean higher priority.
What foods should you avoid with cirrhosis?
Avoid high-sodium foods-canned soups, deli meats, chips, soy sauce, and fast food. Limit processed sugar and saturated fats. Protein is okay in moderate amounts unless you have brain fog, then your doctor may lower it. Always cook fresh, and avoid raw shellfish, which can cause dangerous infections.




Just read this and I’m sitting here with my coffee thinking how wild it is that our bodies can keep lying to us like this. The liver doesn’t scream-it whispers. And by the time you hear it, you’re already two steps behind. I lost my uncle to this. No pain, no warning. Just… gone. Don’t wait for symptoms. Get checked. Seriously.
Love how you broke down elastography. I’m a nurse and I see so many patients skip the fibroscan because they think ‘no pain = no problem.’ But that 12.5 kPa cutoff? It’s terrifyingly accurate. I’ve had patients cry when they see the number-because they finally understand why they’ve been so tired for years.
Oh please. Everyone’s acting like this is some new revelation. I’ve been screaming about liver health since 2018. You think your ‘routine blood test’ is magic? It’s not. It’s the bare minimum. You need a fibroscan AND a viral panel AND a metabolic panel. And if you’re not tracking your albumin and INR monthly once you’re over 40, you’re playing Russian roulette with your organs. #CanadaSavesLivers
they’re hiding the truth… the real cause isn’t alcohol or hepatitis… it’s the glyphosate in our food. big pharma doesn’t want you to know that the liver is literally being poisoned by the same chemicals that make your corn syrup. that’s why transplants are rising. they’re not curing it-they’re profiting off it. 🌱☠️
Let’s deconstruct the metaphysics of hepatic regeneration, shall we? The liver’s ‘regenerative capacity’ is a neoliberal myth-a capitalist illusion of resilience designed to absolve us of collective responsibility for environmental degradation and dietary nihilism. Scar tissue isn’t failure-it’s adaptation. The body isn’t breaking down; it’s reorganizing in response to systemic violence. So when you say ‘stop drinking,’ you’re really saying ‘conform to the hegemony of metabolic purity.’ And let’s not ignore that the MELD score is just a quantified manifestation of bio-power.
Thank you for writing this with so much heart 💛 I’ve been living with compensated cirrhosis for 3 years now. I stopped drinking. I lost 22 lbs. I take my meds. Some days are still rough-but I’m here. And if this helps even one person get tested? That’s everything. You’re not alone. We’re in this together. 🌿
From India, where liver disease is rising fast but awareness is low. I shared this with my village clinic. Many people think only alcoholics get this. I told them: ‘Your roti, your sugar, your soda-these are the real killers.’ Thank you for the clarity. We need more like this.
ok so i just found out my alt is 120 and i drink 2 beers a night… is it too late?? i mean i stopped last week but my wife says im gonna die 😭 i dont wanna die i just wanna play video games
Of course you’re all missing the point. This isn’t about health-it’s about control. The medical industrial complex profits off fear. They push transplants because they’re expensive. They scare you with MELD scores to keep you compliant. The truth? Your liver can heal if you just eat raw foods, sunbathe, and stop taking ‘meds’ that are just poison in capsules. You’re being manipulated.
bro i just saw a guy on tiktok say liver transplants are fake and the hospital just gives you a new liver from a parallel universe… i dont know what to believe anymore 🤯
You’re not alone. I was diagnosed with fatty liver at 32. I thought I was fine because I didn’t drink. Then I learned it was sugar. I swapped soda for water, started walking 30 mins a day, and my enzymes dropped in 6 months. It’s not magic. It’s consistency. You can turn this around. Start today. Not tomorrow. Today.
Thank you for this. I’ve been a liver transplant recipient for 7 years now. I take my anti-rejection meds every single day. I’ve had infections, I’ve had scares, I’ve had panic attacks over bloodwork. But I’m alive. I’m coaching my daughter’s soccer team. I’m traveling. I’m not ‘cured’-but I’m living. And if you’re reading this and you’re scared? I was too. But you don’t have to be. Get help. Get tested. You’re worth it.
Just wanted to add-spironolactone isn’t just for fluid. It can actually help with gynecomastia in men with cirrhosis. I didn’t know that until my doctor mentioned it. Small thing, big impact on quality of life. Always ask about side effects you didn’t know about.
While the clinical overview presented is both comprehensive and commendable, one must acknowledge the socio-economic disparities that impede equitable access to diagnostic modalities such as elastography and transplantation services. In underserved populations, particularly in rural and low-income regions, the absence of infrastructure renders even basic screening inaccessible. Therefore, while the biomedical model is robust, its implementation remains contingent upon structural reform.
Everyone’s so focused on the liver, but what about the pancreas? You think cirrhosis is bad? Try type 2 diabetes with fatty liver. Your body’s just one big broken machine. And you’re all still eating pizza. Pathetic.