 16
Dec,2025
16
Dec,2025
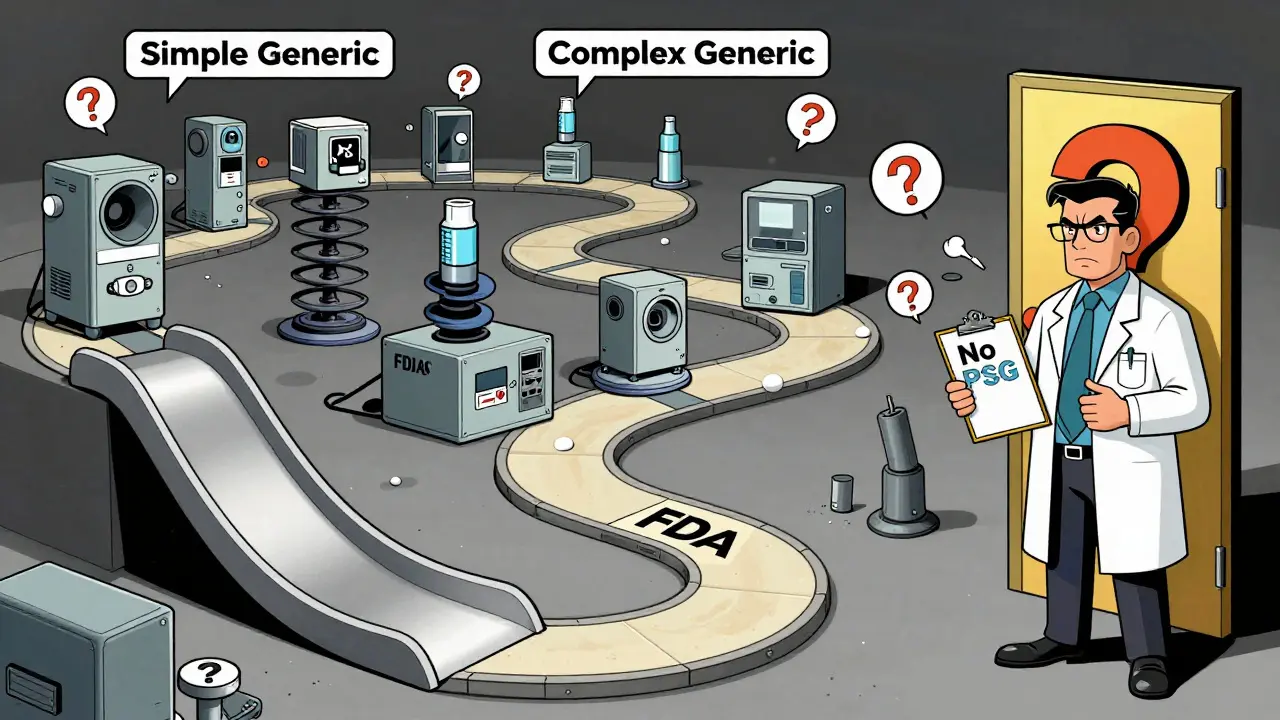
Not all generic drugs are created equal. While most generic pills you pick up at the pharmacy are simple copies of brand-name drugs-same active ingredient, same dose, same effect-some generics are far more complicated. These are called complex generic drugs. And they’re the reason why, even after a brand-name drug’s patent expires, you might still wait years before a cheaper version hits the market.
What Makes a Generic Drug "Complex"?
A complex generic drug isn’t just a pill with a different label. It’s a product where the active ingredient, how it’s made, or how it’s delivered to your body is scientifically tricky. The FDA defines these as drugs with:- Complex active ingredients-like peptides or long-chain polymers
- Advanced formulations-such as liposomes (tiny fat bubbles that carry medicine)
- Special delivery systems-like long-acting injections or inhalers that combine drug and device
- Drug-device combinations-where the medicine and the tool that delivers it (like an inhaler or auto-injector) are inseparable
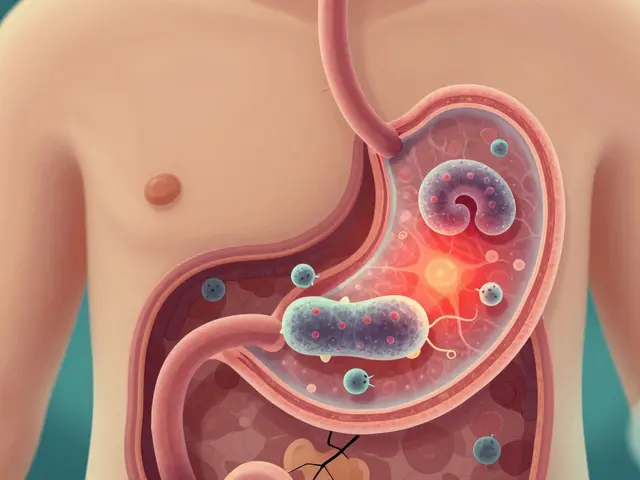
Take bupivacaine liposome injectable, for example. It’s a painkiller wrapped in microscopic fat bubbles that slowly release the drug over days. Making a generic version isn’t just about copying the chemical. You have to recreate the exact size, structure, and release pattern of those fat bubbles-or the drug won’t work the same way. And if the bubbles are even slightly off, the medicine could be ineffective-or even dangerous.
Why Is Approval So Hard?
For simple generics, the FDA uses a straightforward path: the Abbreviated New Drug Application (ANDA). You prove your version is bioequivalent to the brand-name drug-meaning it gets into the bloodstream at the same rate and amount. Easy, right? Not for complex drugs.For these, bioequivalence isn’t as simple as measuring blood levels. A liposomal injection might release medicine over 72 hours. You can’t just check blood samples at one point-you need to map the entire release curve. That requires specialized lab equipment, advanced modeling, and sometimes even animal studies. And even then, the FDA might not have clear rules on how to prove it’s the same.
Then there’s the device part. Take an asthma inhaler. The medicine inside might be identical to the brand. But if the nozzle shape, spray pressure, or even the button’s resistance is slightly different, the FDA may say it’s not equivalent-even if patients can’t tell the difference. Why? Because the device affects how much medicine actually reaches the lungs. A tiny change can mean less medicine gets where it needs to go.
One study reviewed 24 global research papers and found the biggest hurdles were:
- Analytical challenges (19 papers)-figuring out how to measure and compare complex ingredients
- Regulatory uncertainty (21 papers)-no clear guidance from the FDA on what’s acceptable
- Formulation and manufacturing (17 papers)-recreating the exact process without the brand’s secrets
It’s not just science. It’s a guessing game. Without a Product-Specific Guideline (PSG)-a detailed roadmap the FDA publishes for each drug-companies are flying blind. As of 2023, the FDA had issued over 1,700 PSGs, but many complex drugs still don’t have one. That means developers spend years trying to guess what the FDA wants, only to have their application rejected for reasons they didn’t see coming.
How Long Does It Really Take?
A regular generic drug might take 2-3 years and $5-10 million to develop. A complex generic? That jumps to 5-7 years and $20-50 million. And even then, success isn’t guaranteed.Since 2015, the FDA has approved just 15 complex generic drugs. In the same period, over 1,000 simple generics got approved. That’s not because companies aren’t trying. It’s because the science and regulatory path are so uncertain that many just walk away.
Some companies try the 505(b)(2) route-a hybrid path meant for modified drugs. But it’s expensive, requires new clinical data, and still doesn’t guarantee approval. It’s not a shortcut. It’s a detour.
Even when a company finally submits an application, review times can stretch beyond 10 months. The FDA promised to cut review times to 10 months for original generic applications, but complex ones often fall outside that timeline because they need extra expert review.
What’s the FDA Doing About It?
The FDA knows the problem. In 2017, they updated their rules under GDUFA II to give more resources to complex drug reviews. They created the Pre-ANDA Meeting Program, where companies can meet with FDA scientists before submitting an application. By 2023, over 1,200 of these meetings had taken place.They’ve also published more Product-Specific Guidelines-over 200 new ones between 2022 and 2023. And they’ve hired 128 new reviewers specifically for generic drugs.
The approval of the bupivacaine liposome injectable in 2019 was a turning point. It showed that with close collaboration, clear guidance, and advanced science, complex generics can be approved. But it took years of back-and-forth, multiple rounds of testing, and FDA scientists working directly with the manufacturer.
Still, the agency admits it’s a work in progress. Their 2025 research plan includes developing new ways to test bioequivalence for complex products-using things like artificial intelligence to predict how a drug behaves in the body without running full clinical trials.
Why This Matters to Patients
You might wonder: why should I care if a generic takes longer to approve? Because these drugs aren’t just niche products. They’re often the only treatment for chronic conditions-like severe pain, asthma, or certain cancers. When a brand-name drug like a long-acting injectable for pain or an inhaler for COPD goes off-patent, patients expect cheaper options. But without generic competition, prices stay high.Right now, over $75 billion in branded complex drugs are set to lose patent protection by 2028. That’s a huge opportunity for lower-cost alternatives. But if regulatory hurdles don’t change, most of those drugs will still be priced at brand levels for years.
Patients with chronic illnesses can’t wait five years for a generic. And insurance companies can’t keep paying $1,000 a dose when a generic version could cost $200-if it ever gets approved.

What’s Next?
Experts believe technology will help. Machine learning can predict how a liposome behaves in the body. AI can analyze thousands of data points from manufacturing batches to spot subtle differences. Quality-by-design approaches-where the product is built to meet standards from the start, not tested after-could cut review times by up to 45%.But tech alone won’t fix this. The FDA needs to publish guidance faster. Congress needs to keep funding the generic drug program. And manufacturers need to be willing to invest in science that’s risky and slow.
The system isn’t broken-it’s just outdated. The rules were built for aspirin and antibiotics. Now we’re dealing with drugs that behave like living systems. It’s time the approval process caught up.
Why Aren’t More Companies Trying?
It’s not just the science. It’s the risk. A company spends $40 million and seven years developing a complex generic. They submit the application. The FDA asks for more data. Another year. More tests. More money. Then, after eight years, they get rejected because the nozzle on the inhaler was 0.1mm too thick.That kind of risk scares investors. Big pharma avoids it. Smaller companies don’t have the cash. So even when a drug’s patent expires, the market stays dominated by the brand-because no one wants to be the one who loses millions trying to copy it.
The result? Patients pay more. Doctors have fewer options. And the promise of generics-affordable, accessible medicine-stalls on the science.




Man, this is wild. Complex generics aren't just 'copy-paste' like regular generics. Liposomes? Delivery systems? You're not just matching a molecule-you're replicating a nano-engineered delivery mechanism. The FDA's got zero standardized assays for most of this. I've seen labs spend millions just to characterize particle size distribution with dynamic light scattering, and still get rejected because the polydispersity index was 0.18 instead of 0.17. It's not science-it's alchemy with regulatory paperwork.
Why are we even making this hard? If the medicine works, who cares if the bubble is 0.1mm off? Americans overthink everything. In the UK, we just check if it kills the pain. Simple.
They're hiding something. The FDA and Big Pharma are in cahoots. Why else would they make it impossible to copy these drugs? It's all about keeping prices high. They don't want you to get cheap medicine. They want you addicted to $1000 doses. The 'science' is just a cover. Look at the timeline-always delays. Always. Coincidence? I think not.
It's fascinating how the regulatory framework remains fundamentally rooted in 20th-century pharmacokinetics while the therapeutics have evolved into precision nanomedicine. The disconnect isn't inefficiency-it's epistemological. We're applying linear, batch-tested paradigms to stochastic, system-level delivery mechanisms. Until we reframe bioequivalence as a dynamic systems problem, we're just rearranging deck chairs on the Titanic.
As someone who's worked with inhaler formulations in India and then moved to the U.S., I can tell you-this isn't just a U.S. problem. But the U.S. has the resources to fix it. What's missing is political will. In places like Brazil and Thailand, they've cracked simpler complex generics by partnering with academic labs and using open-source analytical models. The FDA could do the same. They just need to stop treating manufacturers like suspects and start treating them like partners. This isn't about control-it's about access. And access is a human right, not a patent privilege.
There's a deeper philosophical tension here. The Enlightenment ideal of reproducibility-the belief that if you replicate the components, you replicate the outcome-collides with the postmodern reality of emergent biological systems. A liposome isn't a molecule; it's a dynamic, self-assembling structure whose behavior emerges from context. To demand bioequivalence by chemical assay is to demand that a symphony be judged by the pitch of a single violin. We need new epistemologies. Not just new regulations. Not just new tools. New ways of knowing.
lol so the FDA is just being lazy? nah. theyre just protecting big pharma. every time someone tries to make a generic they get shut down for something dumb like the button on the injector being too stiff. meanwhile the brand name drug costs 10k and no one says anything. its all rigged. and dont even get me started on how the FDA hires people who used to work for pfizer. total circus
Just read a paper from the NIH last month-AI models trained on manufacturing data from 12,000 liposome batches predicted FDA rejection with 89% accuracy before submission. Imagine if we used that to guide development instead of punishing failure. We could cut approval time in half. But the system rewards caution over innovation. We’re stuck in a feedback loop of risk aversion. It’s not that we can’t solve this. It’s that we’ve forgotten how to try.