 1
Dec,2025
1
Dec,2025
When it comes to cutting healthcare costs without sacrificing effectiveness, biosimilars are one of the most powerful tools available. But how they’re adopted, approved, and used varies wildly between Europe and the United States. Even though both regions are targeting the same goal-making expensive biologic drugs more affordable-their paths couldn’t be more different.
Europe Got a 9-Year Head Start
Europe didn’t just lead the biosimilar race; it built the entire track. The European Medicines Agency (EMA) approved the world’s first biosimilar, Omnitrope (a growth hormone), in 2006. That gave European doctors, hospitals, and payers nearly a decade to get comfortable with these drugs. By the time the U.S. approved its first biosimilar, Zarxio, in 2015, Europe already had over 50 biosimilars on the market.It wasn’t just about being first. Europe created a clear, science-based regulatory system. The EMA didn’t demand endless new clinical trials. Instead, they focused on rigorous analytical data, non-clinical studies, and targeted clinical trials only when needed. This "totality of evidence" approach made approval faster and cheaper for manufacturers.
That efficiency translated into real-world use. In countries like Germany, France, and the UK, hospital procurement systems started favoring biosimilars through competitive tenders. Pharmacists could substitute biosimilars for brand-name biologics without needing a doctor’s new prescription. In oncology and rheumatology, biosimilars now make up more than 80% of prescriptions in some European countries.
The U.S. Struggled to Catch Up
The U.S. passed the Biologics Price Competition and Innovation Act (BPCIA) in 2009, but it took six years just to get the first biosimilar approved. Why the delay? It wasn’t science. It was legal and economic roadblocks.Originator drug companies used patent thickets-layers of overlapping patents-to block competition. They sued biosimilar makers, dragged out negotiations through the so-called "patent dance," and settled deals that delayed market entry for years. Even when a biosimilar got FDA approval, it often couldn’t launch because of legal injunctions.
Then there was the interchangeability hurdle. The FDA required biosimilars to prove they could be switched back and forth with the original drug without risk. That meant costly and time-consuming clinical switching studies. Only a handful of biosimilars ever cleared that bar.
By 2024, the U.S. had approved just over 20 biosimilars. Europe had approved more than 100. And while biosimilars accounted for nearly half of all biologic prescriptions in parts of Europe, they made up less than 10% in the U.S. - despite having a much larger biologics market.
The Game Changed in June 2024
Everything started shifting in June 2024, when the FDA proposed a major rule change: no more mandatory switching studies for interchangeable biosimilars.This was huge. It meant the U.S. was finally moving toward the European model. If a biosimilar was shown to be highly similar to the reference product through analytical and clinical data, it could now be labeled interchangeable without running new patient-switching trials. That cut years off development timelines and slashed costs.
The change didn’t come out of nowhere. It was driven by pressure from payers, patients, and even some drugmakers who realized the old system was holding back competition. The Inflation Reduction Act of 2022 also helped by closing the Medicare Part D coverage gap, making biosimilars more attractive to insurers.
Now, biosimilar makers are rushing to file applications. More than a dozen Humira biosimilars have been approved, and several are finally launching in 2025 after years of patent battles. Pfizer, Merck, and Samsung Bioepis are all expanding their U.S. biosimilar pipelines.

Market Size: Europe Still Leads, But the U.S. Is Catching Fast
In 2024, Europe’s biosimilar market was valued at around $13 billion. The U.S. market was close behind at $10.9 billion. But growth rates tell a different story.Europe’s market grew at about 13% annually from 2020 to 2024. The U.S. grew at 11% over the same period. But projections for 2025-2034 show the U.S. accelerating faster: 17.5% to 18.5% CAGR, compared to Europe’s 17.3%. Why? Because the U.S. is catching up.
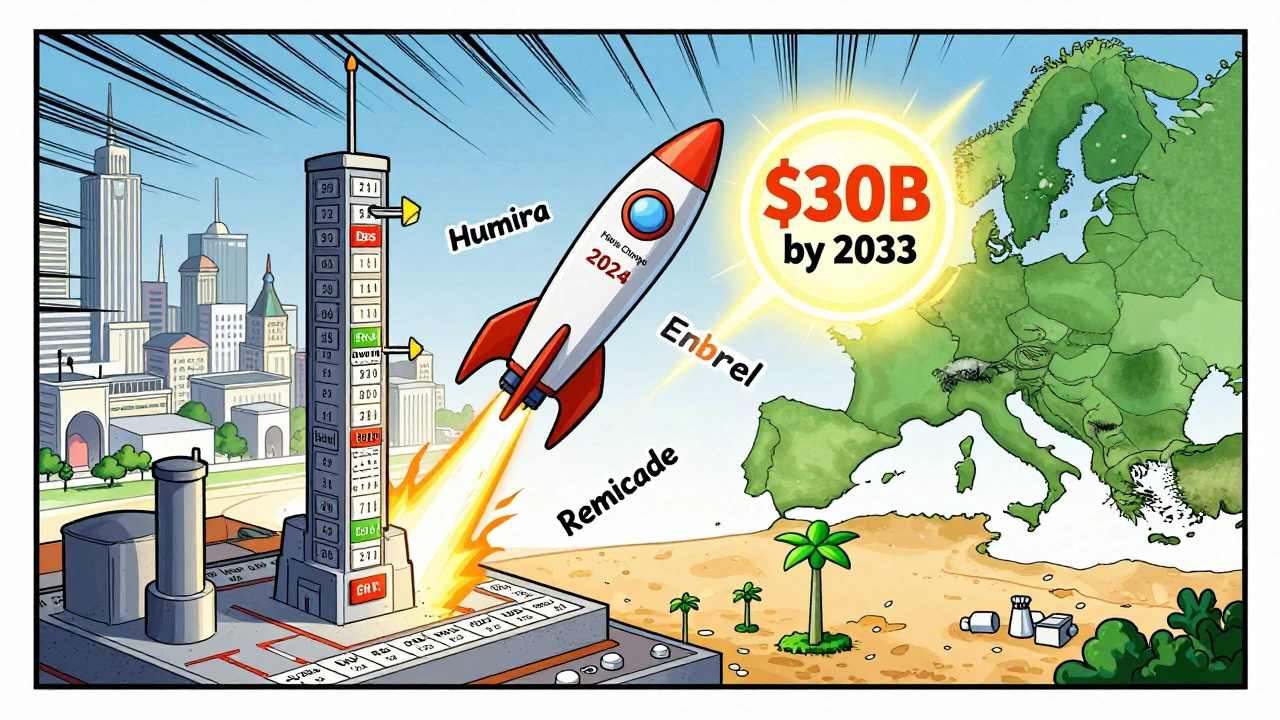
Europe’s market is mature. Most of the easy wins-like biosimilars for growth hormone and erythropoietin-are already in place. The U.S., by contrast, is just starting to tap into the big-ticket biologics: Humira, Enbrel, Remicade, Herceptin. These drugs each generate billions in annual sales. When their patents expire, biosimilars could save the U.S. healthcare system tens of billions.
By 2027, North America (mostly the U.S.) is projected to overtake Europe in total biosimilar revenue. By 2033, the U.S. market alone could hit $30 billion. Europe will keep growing, too-projected to reach $65 billion by 2034-but the U.S. is no longer playing catch-up. It’s becoming the new frontier.
Who’s Making These Drugs?
The top biosimilar makers are global, but their focus differs by region.In Europe, Sandoz (Novartis), Fresenius Kabi, and Amgen dominate. Germany, in particular, has become a biosimilar manufacturing hub. Companies there don’t just sell drugs-they build the entire supply chain, from cell lines to packaging.
In the U.S., Pfizer and Merck are leading the charge. Samsung Bioepis, a South Korean company, has made a major push into the American market with multiple biosimilars approved for rheumatoid arthritis and cancer. These companies aren’t just competing on price-they’re investing in manufacturing scale and distribution networks to win over insurers and hospitals.
Therapeutic Areas: Where the Action Is
The types of biosimilars approved and used also differ between the two markets.Europe led in autoimmune diseases: drugs for rheumatoid arthritis, Crohn’s disease, and psoriasis. These are chronic conditions where patients stay on the same drug for years, making substitution easier to manage.
The U.S. started with supportive care drugs like filgrastim (used to boost white blood cells after chemotherapy). These were simpler to adopt because they were used in short-term, hospital-based settings.
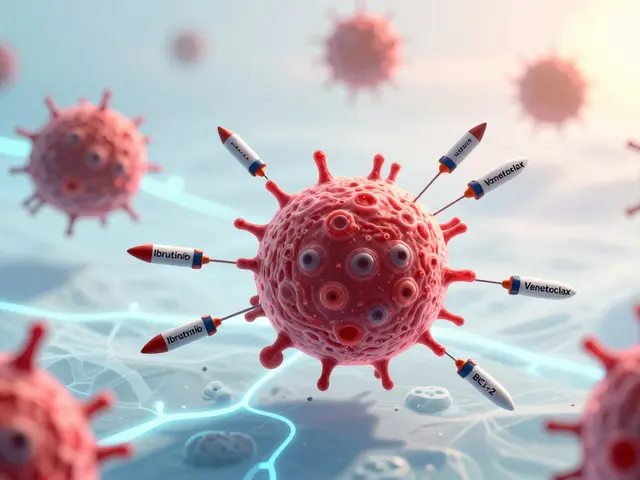
Now, the U.S. is moving into the same high-value areas as Europe. With Humira biosimilars finally hitting the market in 2025, dermatology and gastroenterology are about to see a major shift. Oncology biosimilars-like those for trastuzumab and bevacizumab-are also gaining traction, especially as more hospitals adopt biosimilar formularies.
What’s Holding Both Markets Back?
Even with progress, challenges remain.Manufacturing complex biologics is still incredibly difficult. A tiny change in cell culture conditions can alter the final product. That’s why regulators demand so much data. Even small differences can raise safety questions.
Physician and patient education is another hurdle. Many doctors still think biosimilars are "generic versions"-which they’re not. Biologics are made from living cells, not chemicals. Patients worry about switching from a drug they’ve been on for years. Clear communication and real-world data are key to building trust.
And then there’s pricing. While biosimilars launch at 15-30% discounts, they don’t always lead to lower prices for patients. Insurers sometimes just pocket the savings instead of passing them on. Without policies that force transparency or require savings to be shared, the full cost benefit won’t be realized.
The Big Picture: Cost Savings Are Real
The bottom line? Biosimilars are saving billions. In Europe, they’ve cut biologic spending by an estimated 25-40% in key therapeutic areas. In the U.S., the potential is even bigger. IQVIA estimates that biosimilars could save the American healthcare system $232 billion between 2025 and 2034, just from the biologics coming off patent.That’s not just good for budgets. It’s good for patients. More people can get access to life-changing treatments. More hospitals can afford to treat more patients. More insurers can cover more drugs without raising premiums.
Europe showed it could be done. The U.S. is now proving it can do it faster.
Are biosimilars the same as generics?
No. Generics are exact chemical copies of small-molecule drugs, like aspirin or metformin. Biosimilars are highly similar versions of complex biologic drugs made from living cells-like antibodies or proteins. They’re not identical, but they have no clinically meaningful differences in safety or effectiveness. The FDA and EMA require extensive testing to prove this similarity.
Why did Europe adopt biosimilars faster than the U.S.?
Europe had a head start with its 2006 regulatory framework and simpler approval process. It also had centralized hospital procurement systems that pushed biosimilars through tenders. Pharmacists could substitute them automatically. In the U.S., patent lawsuits, complex payer systems, and strict interchangeability rules slowed adoption for nearly a decade.
What changed in the U.S. in June 2024?
The FDA dropped the requirement for switching studies to get interchangeable status. Previously, manufacturers had to prove patients could safely switch back and forth between the biosimilar and the original drug. That added years and millions in costs. Removing that barrier makes it easier and cheaper for companies to launch interchangeable biosimilars-mirroring Europe’s approach.
Which countries in Europe lead in biosimilar use?
Germany, France, and the UK are the leaders. Germany is also the biggest manufacturing hub, with companies like Fresenius Kabi and Sandoz operating major production sites. These countries use hospital tenders, mandatory substitution policies, and physician education to drive high adoption rates-often over 80% in key therapeutic areas like rheumatology and oncology.
Will biosimilars lower drug prices for patients?
They have the potential to, but it’s not guaranteed. Biosimilars typically launch at 15-30% lower prices than the original biologic. But if insurers don’t pass those savings to patients through lower copays, or if manufacturers raise prices on the original drug to offset competition, patients may not see direct benefits. Policies that require transparency and cost-sharing are needed to ensure savings reach the people who need them.
What’s next for biosimilars in the U.S.?
The next wave includes biosimilars for high-revenue biologics like Humira, Enbrel, and Stelara. With patent protections ending in 2023-2025, over a dozen Humira biosimilars are now entering the market. Expect faster approvals, more interchangeable designations, and increased use in outpatient clinics. The U.S. is no longer lagging-it’s becoming the fastest-growing biosimilar market in the world.



Ugh, another boring Pharma report. Can we talk about something that actually matters? Like, I dunno, my rent? 😩
The regulatory divergence between the EMA and FDA has historically reflected fundamentally different risk-benefit paradigms. The EMA’s totality-of-evidence framework prioritizes analytical comparability and pharmacovigilance, whereas the U.S. system, until recently, imposed additional clinical interchangeability requirements that introduced unnecessary barriers to market entry. The June 2024 FDA guidance represents a paradigm shift toward evidence-based, risk-proportionate regulation - aligning with international standards and enhancing biosimilar accessibility.
Europe? Pfft. They’ve been doing biosimilars since 2006 because they’re basically socialists who think drugs should be handed out like free baguettes. Meanwhile, the U.S. actually values innovation - even if it costs more, at least it’s *ours*. 🇺🇸
I’ve been thinking about this a lot - especially how the U.S. kept delaying biosimilars not because of science, but because of legal games and patent thickets. It’s frustrating, because the data has always been there. The real question is: why did it take so long for the system to catch up to the science? And now that it has, will we actually let it work? Or will someone find a new way to slow it down again?
Let’s be honest - the FDA’s new rule isn’t a breakthrough. It’s a surrender. The U.S. spent 15 years building a fortress around biologics, and now, with Humira’s patent cliff looming, they’re just tearing down the walls. This isn’t progress - it’s panic dressed up as policy.
It’s so encouraging to see the U.S. finally moving toward a system that prioritizes patient access over corporate litigation. The fact that we’re now seeing multiple Humira biosimilars launch after years of delays gives me real hope - not just for cost savings, but for a healthcare system that finally starts putting people before profits. This is the kind of change that takes time, but when it happens, it changes lives.
man i just read this whole thing and i’m like… wow. europe was just chillin’ with their biosimilars like it was no big deal, and us? we were stuck in a courtroom drama with patent dances and lawsuits like it was a netflix series 😅
HOW DARE THEY?! The U.S. is being sabotaged by Big Pharma?! And now they’re just gonna let biosimilars in?! WHAT ABOUT THE PATIENTS?! THE INNOVATION?! THE DRAMA?! This isn’t just policy - it’s a betrayal!!!
The regulatory alignment is long overdue but the real challenge now is implementation - hospitals still have entrenched formularies, payers don’t always incentivize biosimilars, and prescribers need education. The science is there, but the system hasn’t fully adapted yet. We’re at the tipping point - not the finish line.
Let’s not romanticize Europe’s adoption. Their 80% uptake in rheumatology isn’t due to superior policy - it’s because they have centralized, top-down procurement systems that crush competition. The U.S. market is messier, yes - but it’s also more dynamic. The real win isn’t market share - it’s whether innovation continues to thrive under biosimilar pressure.
One thing I’m curious about: how will biosimilar pricing evolve once multiple competitors enter the Humira space? Will we see price erosion like we did with insulin? Or will manufacturers engage in strategic pricing to maintain margins? The data from Europe suggests deep discounts, but U.S. payer dynamics are more fragmented - could that slow the drop?
USA thinks it's better than everyone. But look at the numbers - Europe saved billions. USA? Still arguing over who gets to patent a protein. Sad.
It’s poetic, really - Europe built the cathedral, and now America’s finally showing up with a ladder and a hammer. But let’s not forget: the bricks were laid with patient trust, not just regulatory efficiency. The real question isn’t who’s faster - it’s who’s more humane.
Europe? Yeah they got a head start… but we’re gonna crush them. Biosimilars? Just a stepping stone to American dominance. We don’t copy - we improve. And we do it better. #AmericaFirst #BiotechSupremacy