 23
Dec,2025
23
Dec,2025
When your doctor suggests a cheaper version of your medication, you might hear the words biosimilar or generic. At first glance, they sound the same-both promise lower prices. But they’re not interchangeable. Choosing the wrong one could mean confusion, unnecessary worry, or even a treatment that doesn’t work as expected. Understanding the difference isn’t just about saving money-it’s about making sure your treatment stays safe and effective.
What’s the Real Difference?
Generics and biosimilars both cut costs, but they come from completely different scientific worlds.Generics are copies of small-molecule drugs. Think of them like a photocopy of a simple drawing. If the original is atorvastatin (Lipitor) for cholesterol, the generic is chemically identical-same atoms, same structure, same way it works in your body. The FDA requires generics to match the brand-name drug in strength, dosage, and how fast it enters your bloodstream. That’s called bioequivalence. And it’s proven with tests showing the drug behaves within 80-125% of the original. Over 11,000 generic drugs are approved in the U.S. alone.
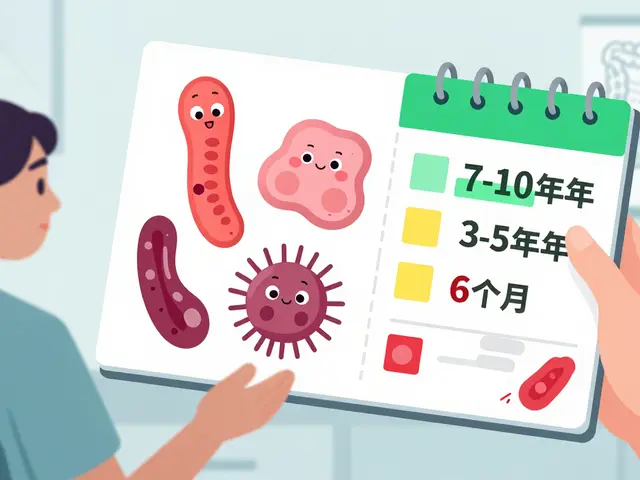
Biosimilars, on the other hand, are copies of large, complex biologic drugs made from living cells-like yeast, bacteria, or hamster ovary cells. These aren’t simple molecules. They’re proteins, sometimes bigger than a bread loaf in molecular size. Because they come from living systems, no two batches are exactly alike. Even tiny changes in temperature, pH, or cell culture can alter the final product. So biosimilars aren’t “identical”-they’re “highly similar.” The FDA requires hundreds of lab tests, animal studies, and clinical trials to prove there’s no meaningful difference in safety or effectiveness. As of 2023, only 46 biosimilars have been approved in the U.S., mostly for cancer, arthritis, and diabetes.
Cost Savings: Big Difference, Big Impact
Generics save you a lot. On average, they cost 80-85% less than the brand-name version. If your cholesterol pill costs $300 a month, the generic might be $50. That’s huge for people paying out of pocket.
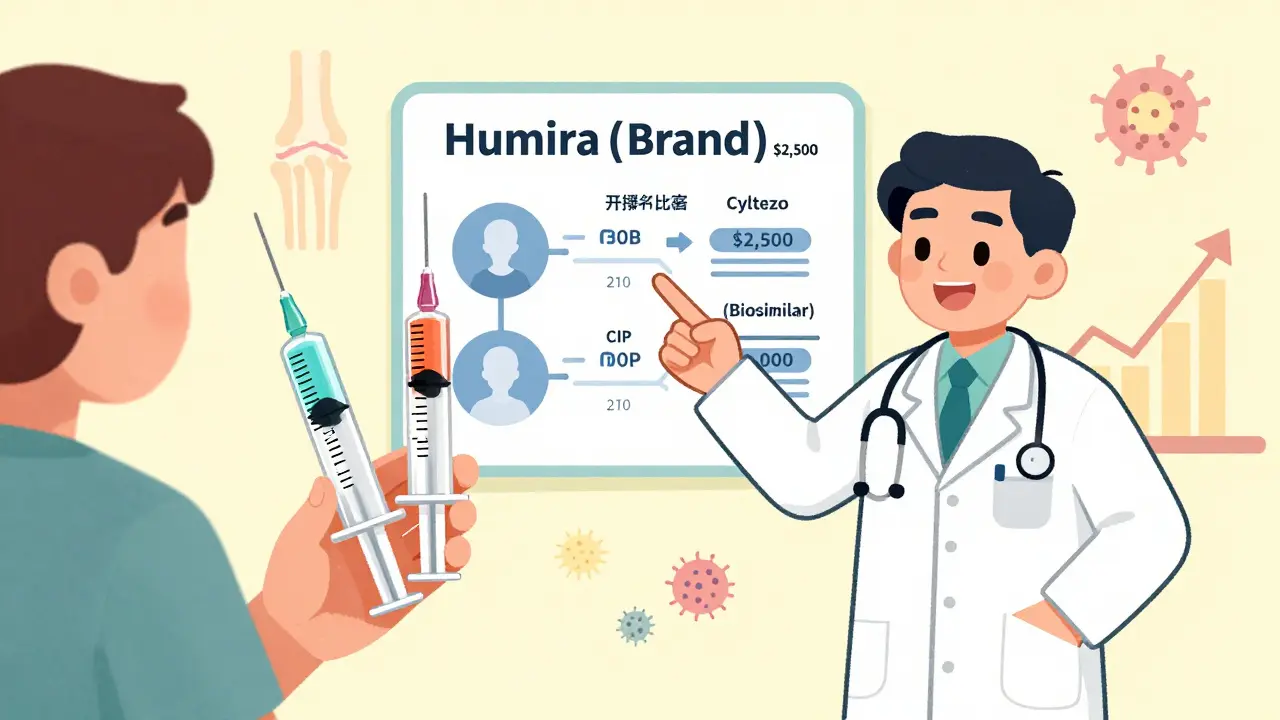
Biosimilars? They save less-around 15-20%. That’s still meaningful, especially when the original drug costs $10,000 a year. For example, the biosimilar version of adalimumab (Humira) might drop your monthly bill from $2,500 to $2,000. It’s not a 90% drop like generics, but for chronic conditions where you take the drug for years, it adds up. A 2023 RAND Corporation report found that biosimilars could save the U.S. healthcare system $34 billion by 2028.
Why the gap? Making a generic is cheap-around $2-3 million and takes 3-4 years. Making a biosimilar? It’s $100-250 million and takes 8-10 years. The science is harder. The equipment is more specialized. The testing is deeper. That’s why biosimilars cost more to produce-and why their price drop isn’t as steep.
Switching: Is It Safe?
If you’re stable on a brand-name drug, can you switch to a cheaper version without risk?
For generics: absolutely. A landmark 2019 JAMA study looked at 47 trials involving heart medications and found no difference in outcomes between brand-name and generic versions. Patients had the same number of heart attacks, strokes, or side effects. Generics have been used for decades. Doctors trust them.
For biosimilars: the data is strong, but newer. A 2022 review of 128 studies involving over 38,000 patients with rheumatoid arthritis found no difference in effectiveness or safety between the original infliximab and its biosimilar. The American College of Rheumatology now recommends biosimilars as a first-line option. But concerns linger-especially in sensitive areas like inflammatory bowel disease or cancer.
One real-world concern is immunogenicity: your body might react to tiny differences in the protein structure and create antibodies. This could make the drug less effective-or cause side effects like rashes or fatigue. So far, approved biosimilars haven’t shown higher rates of this. The FDA’s adverse event database shows biosimilar infliximab has a slightly lower rate of side effects than the original (0.12 vs. 0.15 per 100 patient-years).
Still, patients report anxiety. A 2022 National Psoriasis Foundation survey found 42% of patients were nervous about switching. One Reddit user wrote: “I was scared to switch to the biosimilar insulin. My doctor spent 20 minutes explaining it. Now I’m saving $1,200 a year and feel fine.” Education matters.
Who Decides? Pharmacists, Doctors, and Rules
Can your pharmacist switch your drug without asking your doctor?
For generics: yes, in 49 states. If your prescription says “Lipitor,” your pharmacist can give you atorvastatin unless your doctor writes “dispense as written.” It’s automatic.
For biosimilars: it’s complicated. Only “interchangeable” biosimilars can be swapped without the doctor’s permission. As of 2024, only a handful have received this status-like Semglee (insulin glargine) and Cyltezo (adalimumab). Even then, 28 states require the pharmacist to notify your doctor within 72 hours. Some states require written consent. Others don’t allow substitution at all.
Doctors also play a role. A 2023 AMA survey found only 58% of non-specialist physicians felt confident prescribing biosimilars. Many still default to the brand-name because they’re unfamiliar with the data. That’s changing, but slowly.
Where Are Biosimilars Used? Where Generics Don’t Work
Generics work great for pills: blood pressure meds, antidepressants, antibiotics, thyroid drugs. If it’s a small molecule, there’s likely a generic.
Biosimilars? They’re for biologics-injectables and infusions you can’t replicate with chemistry. Think:
- Trastuzumab (Herceptin) for HER2+ breast cancer
- Adalimumab (Humira) for rheumatoid arthritis
- Bevacizumab (Avastin) for colon cancer
- Insulin glargine (Lantus) for diabetes
There are no generics for these. You can’t chemically copy a protein made by living cells. That’s why biosimilars exist-they’re the only affordable option.
For example, a Stage IV colon cancer patient in a 2023 forum wrote: “My oncologist switched me to the bevacizumab biosimilar. My tumor markers stayed stable. My out-of-pocket cost dropped from $450 to $75 per infusion.” That’s life-changing.
What You Should Do
If you’re prescribed a new medication:
- Ask: Is this a brand, generic, or biosimilar?
- If it’s a pill: generics are safe and standard. No need to worry.
- If it’s an injection or infusion: ask if a biosimilar is available. Ask if it’s interchangeable.
- Ask your doctor: “Has this been studied in patients like me?”
- Ask your pharmacist: “Can you substitute this? What’s the process?”
- Check the FDA’s Purple Book for biosimilars and Orange Book for generics.
Don’t assume cheaper means riskier. The FDA holds both to high standards. But don’t assume they’re the same either. The science is different. The savings are different. The rules are different.
What’s Next?
The Inflation Reduction Act of 2022 removed financial penalties for doctors who use biosimilars in Medicare. That’s pushing more hospitals and insurers to adopt them. By 2027, biosimilars could make up 45% of all biologic prescriptions, up from 22% today.
New biosimilars are coming fast. The first for Stelara (ustekinumab), used for psoriasis and Crohn’s disease, could hit the market in 2024. That could save $5 billion a year in the U.S.
But challenges remain. Patent lawsuits delay biosimilar entry by nearly five years on average. Many patients still don’t know what a biosimilar is. And not all insurance plans cover them equally.
The bottom line: if you’re on a biologic, ask about the biosimilar. If you’re on a pill, take the generic. Both are safe. Both save money. But only one is the right choice for your drug type.
Real Stories, Real Results
One rheumatoid arthritis patient in Melbourne switched to an adalimumab biosimilar in 2023. “I saved over $8,000 a year,” she said. “My joints still feel the same. My doctor showed me the data. That’s all I needed.”
A cancer patient in Sydney switched to a trastuzumab biosimilar. “I was terrified,” he said. “But my oncologist said, ‘We’ve seen this work in over 100 people here.’ I trusted that.” His tumor stayed stable. His bills dropped by 80%.
Not everyone feels this way. Some fear the unknown. Some worry about side effects. But the science is clear: approved biosimilars work. And for many, they’re the only way to afford treatment.
Are biosimilars as safe as the original biologic drugs?
Yes. The FDA requires biosimilars to undergo extensive testing-including analytical studies, animal trials, and clinical trials-to prove they have no clinically meaningful differences in safety, purity, or potency. Real-world data from over 38,000 patients shows no increase in side effects or treatment failure compared to the original biologic. The FDA’s adverse event reporting system confirms biosimilars have safety profiles nearly identical to their reference products.
Can I switch from a brand-name biologic to a biosimilar without my doctor’s approval?
Only if the biosimilar is designated as “interchangeable” by the FDA and your state allows pharmacy-level substitution. As of 2024, only a few biosimilars (like Semglee and Cyltezo) have this status. Even then, 28 states require the pharmacist to notify your doctor within 72 hours. Always check your state’s laws and ask your pharmacist before any switch.
Why are biosimilars more expensive to develop than generics?
Biosimilars are made from living cells, which creates complex, large molecules that can’t be perfectly copied. Manufacturing requires precise control of temperature, pH, and cell culture conditions. The development process involves hundreds of lab tests, animal studies, and clinical trials-costing $100-250 million and taking 8-10 years. Generics are simple chemical compounds made in labs for $2-3 million over 3-4 years.
Do biosimilars work the same for all conditions?
Biosimilars are approved for specific uses based on clinical data. For example, a biosimilar for rheumatoid arthritis may not be approved for Crohn’s disease unless tested for that condition. Each biosimilar is approved only for the same conditions as its reference product, based on the totality of evidence. Always confirm the approved uses with your doctor or pharmacist.
Can I trust a biosimilar if it’s cheaper?
Yes. Cost doesn’t reflect quality here. Biosimilars are not “cheap knockoffs.” They go through the same rigorous FDA approval process as the original biologic, just with a different pathway. The lower price comes from reduced development costs compared to the original, not from cutting corners. The FDA, WHO, and European Medicines Agency all confirm biosimilars are safe and effective.
What’s the difference between interchangeable and non-interchangeable biosimilars?
An interchangeable biosimilar has been proven to produce the same clinical result as the reference product in any patient, and switching between them won’t increase safety risks. It can be substituted at the pharmacy without the prescriber’s permission. A non-interchangeable biosimilar is still safe and effective but requires a new prescription each time you switch. Only a few biosimilars have achieved interchangeable status so far.
Why aren’t more doctors prescribing biosimilars?
Many doctors, especially non-specialists, haven’t been trained on biosimilars. A 2023 AMA survey found only 58% of non-specialist physicians felt confident prescribing them. Others worry about patient anxiety or unclear insurance rules. But awareness is growing. The FDA, professional societies, and manufacturer education programs are helping bridge the gap.
Do biosimilars require special storage?
Yes. Most biosimilars are proteins and require refrigeration (2-8°C) to stay stable. They can’t be left at room temperature like many generics. This affects how they’re shipped, stored in pharmacies, and even how patients transport them. Always check the label and ask your pharmacist about proper handling.
Are there any long-term risks with switching between biosimilars and the original drug?
Current data shows no increased risk. Studies tracking patients who switched multiple times between reference biologics and biosimilars found no rise in side effects or loss of effectiveness. However, long-term data beyond five years is still limited. Ongoing monitoring through registries and post-marketing studies continues to track safety. So far, the evidence supports safe switching.
How do I find out if my medication has a biosimilar or generic version?
For generics, check the FDA’s Orange Book online. For biosimilars, use the FDA’s Purple Book. You can also ask your pharmacist or use apps like GoodRx or RxSaver, which list available alternatives and prices. If you’re unsure, your doctor or pharmacist can look up your medication’s status and tell you what’s available.
Final Thought
You don’t need to be a scientist to choose wisely. If it’s a pill, take the generic. If it’s an injection for cancer, arthritis, or diabetes, ask about the biosimilar. Both are proven, both are safe, and both help you afford the treatment you need. The key isn’t which one is cheaper-it’s which one is right for your drug.




Generics are just as good as brand-name drugs, period. I’ve been on generic metformin for eight years and my blood sugar’s better than when I was on the brand. People act like generics are some kind of scam, but the FDA doesn’t approve junk. If your doctor says it’s bioequivalent, trust the science, not the marketing.
Let’s be clear: biosimilars are not ‘highly similar’-they’re ‘close enough for government work.’ The FDA’s standards are laughably lax compared to the EMA. And don’t get me started on the ‘interchangeable’ designation-that’s a regulatory loophole dressed up as patient safety. We’re talking about proteins that fold differently depending on the phase of the moon, and now pharmacists are allowed to swap them like candy? This isn’t medicine-it’s pharmaceutical roulette.
I switched to a biosimilar for my Humira and now I can’t feel my toes. My doctor says it’s coincidence but I know better. They’re cutting corners. The company that makes it uses a different kind of hamster. I read a blog that said they’re testing on Syrian hamsters now instead of Chinese and that’s why the antibodies are attacking my nerves. I’m going to the FDA. Someone needs to stop this
In Nigeria we don't have access to biosimilars or generics because of import taxes and corruption. The brand-name drugs cost three times our monthly salary. We use traditional herbs or go without. Your discussion about cost savings is irrelevant to us. You talk about FDA approval like it's universal truth. What about the 80% of the world that doesn't have an FDA? Your privilege is showing.
I appreciate the breakdown. I was nervous about switching my insulin to Semglee, but after reading the data and talking to my endo, I did it. No side effects, no issues. My co-pay dropped from $300 to $45. It’s not about fear-it’s about information. If your doctor doesn’t explain it clearly, ask for a pharmacist consult. Most hospitals have them for free.
Have you ever wondered why the same companies that make the original biologics also make the biosimilars? It’s not a coincidence. It’s a monopoly disguised as competition. The FDA approves these because they’re owned by the same parent corporations-Pfizer, Novo Nordisk, AbbVie-they’re playing both sides. The ‘savings’ are just a redistribution of profits. Meanwhile, the real patients? They’re still paying $2,000 a month because insurance won’t cover the biosimilar unless you jump through 17 hoops. This isn’t progress-it’s corporate theater.
Think about it: if you can’t replicate a protein made by a living cell with perfect precision, then what does that say about the nature of medicine itself? We’re trying to control the uncontrollable. The body doesn’t care about FDA classifications-it reacts to energy fields, to subtle vibrations in the molecular structure. Biosimilars are like playing a vinyl record on a digital player-it sounds close, but the soul is missing. We’re reducing life to a spreadsheet. And for what? To save $500 a year? What are we becoming?
OMG I just switched to the biosimilar for my RA med and my skin is breaking out and I think it’s because of the preservatives?? I’m so scared I’m gonna die 😭 I asked my pharmacist and she said it’s fine but I Googled it and now I’m convinced I’m being poisoned. Also my cat sneezed yesterday and I think it’s connected??
The FDA’s approval process for biosimilars is rigorous and scientifically sound. The data from clinical trials is publicly available and peer-reviewed. Concerns about immunogenicity are valid but have been addressed through post-marketing surveillance. The cost savings are not trivial-they enable access to life-sustaining therapy for millions. Dismissing biosimilars based on fear or misinformation undermines public health.