 1
Dec,2025
1
Dec,2025
High blood pressure doesn’t always cause symptoms, but it’s quietly damaging your heart, kidneys, and arteries. If you’ve been told you need medication to bring it down, you’re not alone. About 108 million American adults have hypertension, and most will need more than one pill to get it under control. The good news? We’ve got a lot of options-and knowing how they work can help you pick the right one.
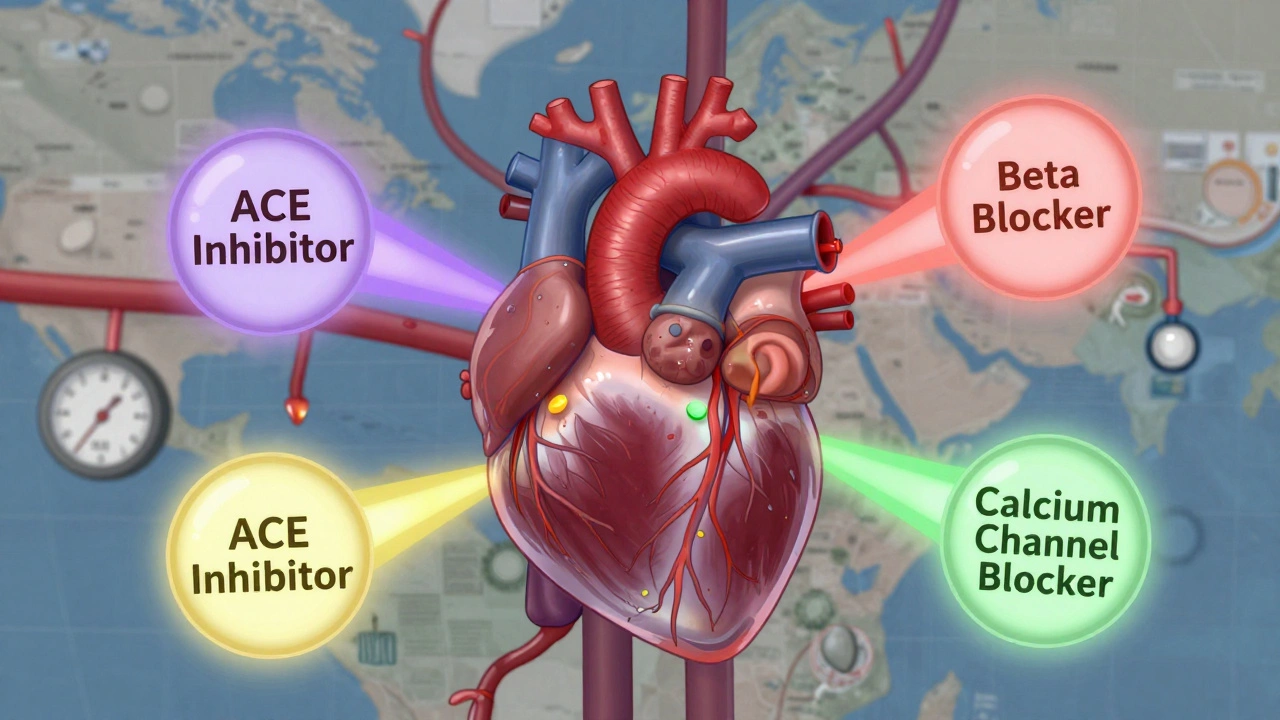
What Are ACE Inhibitors, and Why Do Doctors Prescribe Them?
ACE inhibitors are a class of blood pressure meds with names ending in “-il”: lisinopril, enalapril, ramipril. They work by blocking the enzyme that turns angiotensin I into angiotensin II-a chemical that tightens blood vessels and raises pressure. By stopping this, these drugs let your arteries relax, lowering your blood pressure and reducing strain on your heart.
They’re often the first choice if you have diabetes, chronic kidney disease, or heart failure. Why? Because they don’t just lower pressure-they protect your kidneys and slow down damage. Studies show they reduce protein leakage in urine and delay kidney failure in diabetic patients.
But there’s a catch. About 15-20% of people on ACE inhibitors develop a dry, hacking cough. It’s not dangerous, but it’s annoying. One user on Reddit said their cough kept them awake for months until they switched to losartan. Within three days, it vanished. That’s why many doctors will switch you to an ARB-angiotensin receptor blocker-if the cough sticks around.
Beta Blockers: Slowing Down the Heart
Beta blockers like metoprolol, atenolol, and carvedilol work by blocking adrenaline. They slow your heart rate, reduce how hard your heart pumps, and lower blood pressure. They’re not usually the first pick for high blood pressure alone-but they’re essential if you’ve had a heart attack, have heart failure, or suffer from angina.
They’re also used for anxiety-related spikes in blood pressure or irregular heart rhythms. But they’re not for everyone. Many people report feeling tired, sluggish, or even depressed on beta blockers. One review on Drugs.com called metoprolol “the pill that made me feel like a zombie.” If you’re active, athletic, or work long hours, this side effect can be a dealbreaker.
Another concern: beta blockers can hide signs of low blood sugar in diabetics. If you’re on insulin or other diabetes meds, your doctor needs to know. They might choose something else unless you have a strong reason to be on a beta blocker.
Calcium Channel Blockers: Relieving Vascular Tension
Calcium channel blockers like amlodipine, nifedipine, and diltiazem stop calcium from entering heart and blood vessel cells. This makes the vessels relax and widen. They’re especially effective in older adults and people of African or Caribbean descent, where other drugs sometimes underperform.
Amlodipine is the most common one. It’s taken once a day, lasts 24 hours, and works well with other meds. But it has its own side effect: ankle swelling. About 40% of users report puffiness in their feet or legs, especially after standing all day. It’s not dangerous, but it can be uncomfortable. Elevating your legs and wearing compression socks helps.
Here’s something important: grapefruit juice can boost the effect of some calcium channel blockers-like felodipine-by up to 300%. That means your blood pressure could drop too low. If you’re on one of these, skip the grapefruit. Orange juice? Fine.
Diuretics: The Old Workhorses Still Winning
Diuretics-often called water pills-are among the oldest and cheapest blood pressure drugs. Thiazide diuretics like hydrochlorothiazide and chlorthalidone make you pee more, which reduces fluid volume and lowers pressure. They’re recommended as first-line treatment by the American Heart Association, especially for people over 65.
But not all diuretics are equal. Chlorthalidone is more effective than hydrochlorothiazide at preventing heart attacks and strokes. One study found it reduced cardiovascular events by 18% more than hydrochlorothiazide at the same dose. Yet, many doctors still prescribe hydrochlorothiazide because it’s been around longer and is more familiar.
Side effects? Frequent bathroom trips, low potassium, dizziness. You’ll need blood tests every few months to check your electrolytes. If you’re on a diuretic, your doctor might also give you a potassium supplement or prescribe a potassium-sparing diuretic like amiloride to balance things out.

ARBs: The ACE Inhibitor Alternative
ARBs-angiotensin II receptor blockers-include losartan, valsartan, and irbesartan. They do almost the same thing as ACE inhibitors but block the receptor instead of the enzyme. That means they avoid the dry cough. If you couldn’t tolerate lisinopril, losartan is often the next step.
The LIFE study showed losartan was better than atenolol at reducing heart attacks, strokes, and death in people with high blood pressure and enlarged hearts. It’s also safer for people with kidney disease and is preferred over ACE inhibitors in some populations, like Black patients without kidney disease, according to recent guidelines.
ARBs are more expensive than ACE inhibitors, but generic versions are widely available. Valsartan, for example, costs less than $5 a month with a GoodRx coupon. They’re also used in combination pills like Diovan HCT (valsartan + hydrochlorothiazide) and Exforge (amlodipine + valsartan), which simplify your pill routine.
Combination Pills: One Pill, Two Drugs
Most people with high blood pressure need more than one medication. Taking two or three pills a day can be confusing-and many stop because of the hassle. That’s why combination pills are becoming the norm.
Fixed-dose combinations like Lotrel (amlodipine + benazepril), Benicar HCT (olmesartan + hydrochlorothiazide), and Tekamlo (aliskiren + amlodipine) pack two drugs into one tablet. Studies show patients are 26% more likely to stick with their treatment when they take a single pill instead of multiple ones.
These combos are especially helpful if you have stage 2 hypertension (140/90 or higher). The American Heart Association now recommends starting with two drugs at once in these cases, rather than waiting to add more later. It gets you to your goal faster and reduces long-term risk.
What Doesn’t Work for Everyone
Not all blood pressure meds work the same for every person. Race, age, weight, and other health conditions matter.
For example, ACE inhibitors and ARBs are less effective in Black patients without kidney disease. Calcium channel blockers and diuretics work better here. Why? Research suggests differences in how the body handles sodium and hormones like renin.
Obesity also changes things. Hydrochlorothiazide works less well in people with normal weight, but calcium channel blockers don’t care about BMI. That’s why your doctor doesn’t just pick a drug based on price or popularity-they tailor it to you.
And don’t forget: some meds interact with other conditions. Beta blockers can make asthma worse. Diuretics can cause gout flares. ARBs and ACE inhibitors can raise potassium too high if you have kidney disease. Your doctor needs your full medical history to avoid dangerous mix-ups.
Cost, Adherence, and Real-World Challenges
Most of these drugs are generic and cheap. Lisinopril? $4 a month. Amlodipine? $5. Chlorthalidone? $6. But brand-name combos like Exforge can cost $350 without insurance. Always ask for the generic version. Use GoodRx or your pharmacy’s discount program.
Still, only 54% of people with high blood pressure get it under control. Why? Side effects, forgetfulness, or not understanding why the pill matters. One study found that people who took a single-pill combo were far more likely to stick with treatment than those juggling multiple pills.
If you’re struggling to take your meds, talk to your doctor. They can simplify your regimen, switch to a better-tolerated drug, or adjust the dose. Don’t just quit. Uncontrolled blood pressure increases your risk of stroke, heart attack, and kidney failure.
What’s New in 2025?
There’s exciting progress beyond pills. In late 2023, the FDA approved the first implantable device for resistant hypertension: renal denervation. It uses radiofrequency energy to calm overactive nerves around the kidneys, lowering pressure without drugs. Early results show a 8.5 mmHg drop in systolic pressure compared to sham procedures.
Researchers are also testing genetic tests to predict which drug will work best for you. One study in Nature Medicine found specific gene patterns linked to better responses to calcium channel blockers versus ACE inhibitors. Personalized treatment might be the next big leap.
And the targets? They’re getting lower. The 2023 STEP trial showed that keeping systolic pressure between 110-130 mmHg in adults 60-80 reduced heart problems by 26%. That’s more aggressive than before-but it’s working.
For now, though, the best treatment is still the one you’ll take every day. Whether it’s amlodipine, lisinopril, or a combo pill, consistency beats perfection.
What’s the most common blood pressure medication?
Lisinopril (an ACE inhibitor) is the most prescribed, followed by amlodipine (a calcium channel blocker) and hydrochlorothiazide (a diuretic). These three make up nearly 60% of all hypertension prescriptions in the U.S. They’re cheap, effective, and well-studied.
Can I stop taking blood pressure meds if my pressure normalizes?
No-not without your doctor’s approval. High blood pressure is usually a lifelong condition. Medications don’t cure it; they manage it. Stopping suddenly can cause your pressure to spike dangerously, increasing your risk of stroke or heart attack. Some people can reduce or stop meds after major lifestyle changes (weight loss, low-sodium diet, exercise), but that’s done gradually and under medical supervision.
Why do some people get a cough from ACE inhibitors?
ACE inhibitors cause a buildup of bradykinin, a substance that irritates the airways. This leads to a dry, persistent cough in about 15-20% of users. It’s not an allergy-it’s a side effect. Switching to an ARB like losartan usually fixes it within days, since ARBs don’t affect bradykinin levels.
Which blood pressure medication has the least side effects?
There’s no universal answer-it depends on your body. Amlodipine tends to have fewer severe side effects than beta blockers or ACE inhibitors. But ankle swelling is common. Diuretics can cause frequent urination and electrolyte issues. The best choice is the one that works for your health profile and that you can take consistently. Talk to your doctor about your lifestyle, symptoms, and concerns.
How long does it take for blood pressure meds to work?
Some drugs start working within hours, but it usually takes 2-4 weeks to see the full effect. For example, amlodipine reaches peak levels in 6-12 hours, but it can take up to two weeks for your blood pressure to stabilize. Your doctor will likely check your pressure every 2-4 weeks and adjust the dose until you reach your target. Don’t expect instant results.
Are natural remedies enough to replace blood pressure meds?
Lifestyle changes-like losing weight, cutting salt, exercising, and reducing alcohol-can significantly lower blood pressure. In some cases, they can reduce or even eliminate the need for meds. But if your pressure is 140/90 or higher, especially with other risks like diabetes or heart disease, meds are usually necessary. Natural remedies support treatment-they don’t replace it.
What to Do Next
If you’re on blood pressure medication, keep taking it-even if you feel fine. Track your pressure at home with a validated monitor. Write down your readings and bring them to your next appointment. If you’re having side effects, don’t suffer in silence. There’s almost always another option.
Ask your doctor:
- Is this the best drug for my age, race, and other health conditions?
- Can we try a combination pill to simplify my routine?
- Are there cheaper generics available?
- What side effects should I watch for?
High blood pressure is manageable. The right medication, taken consistently, can add years to your life-and life to your years.





Man, I was on lisinopril for two years and that dry cough was *unreal*. Like, I’d wake up at 3 a.m. hacking like I was trying to dislodge a dead bird. Switched to losartan and boom - silence. Not even a sniffle. I thought I’d never sleep through the night again. ACE inhibitors are great, but if your throat’s on fire, just ask for the ARB. No shame.
Also, grapefruit juice? Don’t even think about it with amlodipine. I learned that the hard way after a weekend brunch with my cousin. Ended up dizzy on the couch for six hours. Orange juice? Perfect. Grapefruit? Enemy number one.
ARBs are the MVP of hypertension meds 😌💊 No cough? Yes please. Also, chlorthalidone > HCTZ - why are we still prescribing the weaker one?? My doc switched me after I showed them the study. BP dropped 15 points in a week. Also, combo pills? Game changer. One pill, no more alphabet soup in my pill organizer. 🙌
Mostly just take amlodipine. Works. No drama.
Thank you for writing this. As someone who’s been on three different meds over five years, I know how overwhelming this can be. I started on lisinopril, got the cough, switched to losartan, then developed ankle swelling from amlodipine - so we went to chlorthalidone + a tiny bit of spironolactone. It’s not perfect, but my BP’s stable and I’m not feeling like a zombie.
Don’t give up. There’s a combo out there for you. And yes, the single-pill combos? Worth every penny. My pharmacy gives them to me for $7 a month with GoodRx. That’s less than my morning coffee.
Also - if you’re active, skip beta blockers unless you *really* need them. I tried metoprolol once. Felt like I was dragging a sofa uphill just to walk to the mailbox.
It’s fascinating how much physiology varies between populations. The fact that ACE inhibitors are less effective in Black patients without kidney disease isn’t just anecdotal - it’s backed by decades of pharmacogenomic research. Renin-angiotensin system activity tends to be lower in this group, making diuretics and CCBs more reliable. It’s not about race per se, it’s about underlying physiological patterns that correlate with ancestry and sodium handling.
And honestly? We’ve been slow to adopt this in clinical practice. Too many docs still default to lisinopril because it’s ‘the standard.’ But if you’re Black and on an ACE inhibitor with no improvement? Push for amlodipine or chlorthalidone. You might be surprised how much better you feel.
Also - don’t underestimate the psychological burden of pill fatigue. Taking four meds a day is exhausting. That’s why fixed-dose combinations aren’t just convenient - they’re lifesaving in terms of adherence. I’ve seen patients who were non-compliant for years suddenly thrive after switching to a single-pill combo. It’s not magic. It’s just simpler.
I’m 68 and was diagnosed with hypertension at 62. I was terrified. Thought I was going to have a stroke tomorrow. My doctor put me on lisinopril - cough city. Then losartan - better, but I still felt weird. Then we tried amlodipine - ankle swelling made me look like I was wearing water wings.
Finally, chlorthalidone + a low-dose amiloride. Perfect. No cough, no puffiness, no dizziness. I take it in the morning, and by 4 p.m., I forget I’m even on meds. I track my BP with my Apple Watch - it’s down to 118/74.
Don’t settle. Keep talking to your doctor. There’s a combo out there that won’t make you feel like a side effect catalog. And yes - yes - get the generic. I pay $4.50 a month. That’s less than a bag of chips.
You’ve got this. You’re not broken. You’re just managing a chronic condition. Like diabetes. Like thyroid. It’s not a failure. It’s a lifestyle upgrade.
so i just found out grapefruit ruins amlodipine?? 😱 i’ve been drinking it every morning for 3 years… i think my bp is low bc i keep fainting when i stand up… oops. gonna switch to orange juice. also, why is chlorthalidone so underrated? my doc acts like it’s some rare alien drug. it’s cheaper than my dog’s flea meds lol
Ugh. I can’t believe people still take HCTZ. It’s 2025. We have data. We have studies. We have *science*. And yet, doctors are still prescribing a weaker, outdated diuretic like it’s 1998?!!
Chlorthalidone reduces heart attacks by 18% MORE. That’s not a suggestion. That’s a medical emergency in prescribing practices.
And beta blockers for anxiety? Please. You’re not helping anyone by making them feel like a sloth. I had a friend on metoprolol - she quit her job because she couldn’t get out of bed. That’s not treatment. That’s chemical sedation dressed up as medicine.
And don’t get me started on the ‘natural remedies’ crowd. No, lemon water and deep breathing won’t fix 160/100. That’s not holistic - that’s dangerous.
There’s an interesting philosophical tension here: we treat hypertension as a disease to be eradicated, yet it’s often a physiological adaptation - a response to systemic inflammation, endothelial dysfunction, or chronic stress. The drugs don’t cure the root; they mask the symptom. But is that wrong? If masking the symptom prevents stroke, kidney failure, and early death, then perhaps ‘masking’ is the most ethical intervention we have.
And yet - we don’t ask why the body is raising pressure in the first place. We don’t prioritize diet, sleep, or social connection with the same urgency as we do pill prescriptions. Is that because pills are quantifiable? Because they’re profitable? Because they’re easier than asking someone to change their life?
Maybe the real breakthrough isn’t a new drug - it’s a healthcare system that sees blood pressure as a signal, not a villain.
Oh honey. You’re talking about lisinopril like it’s the holy grail. Darling, I’m on a custom compounded triple combo - losartan, amlodipine, and chlorthalidone - in one capsule, flavored like peach. My compounding pharmacy charges $12 a month. It’s *artisanal*. The CVS generics? So… pedestrian. And don’t even get me started on people who take ‘generic’ like it’s a virtue. It’s not about price - it’s about bioavailability, fillers, and the *aesthetic* of your regimen.
I also use a Fitbit that syncs with my Apple Health and sends my BP trends to my integrative cardiologist via encrypted portal. We’re not just managing hypertension - we’re curating a *lifestyle experience*.
And yes, I do meditate for 20 minutes before bed. With Himalayan salt lamps. You’re welcome.
Actually, I just switched to the new renal denervation device last month. No pills. Just a tiny catheter procedure. BP dropped 12 points in a week. No cough, no swelling, no weird food restrictions. It’s not for everyone - only if meds aren’t working - but if you’ve tried everything and still can’t get below 140/90? Talk to your doc about it. It’s FDA-approved, covered by Medicare, and honestly? It feels like cheating.