KDIGO Guidelines: What They Are and How They Shape Kidney Care
When it comes to managing KDIGO guidelines, a set of evidence-based recommendations developed by the Kidney Disease: Improving Global Outcomes organization to standardize kidney disease care worldwide. Also known as Kidney Disease Outcomes Quality Initiative guidelines, they are used by nephrologists, primary care doctors, and patients to decide what treatments work best for kidney disease at every stage. These aren’t just suggestions—they’re the closest thing medicine has to a rulebook for treating chronic kidney disease, acute kidney injury, and related conditions like high blood pressure and mineral imbalances.
KDIGO guidelines directly influence how doctors handle chronic kidney disease, a long-term condition where kidneys slowly lose function, often without symptoms until it’s advanced. They tell you when to test for protein in urine, what blood pressure targets to aim for, and which medications to avoid or prefer. For example, they recommend ACE inhibitors or ARBs for most patients with proteinuria, even if their blood pressure is normal. They also warn against using certain drugs in people with reduced kidney function, like NSAIDs or certain diabetes meds, because they can make things worse. These rules aren’t made in a lab—they’re based on data from thousands of real patients across dozens of countries.
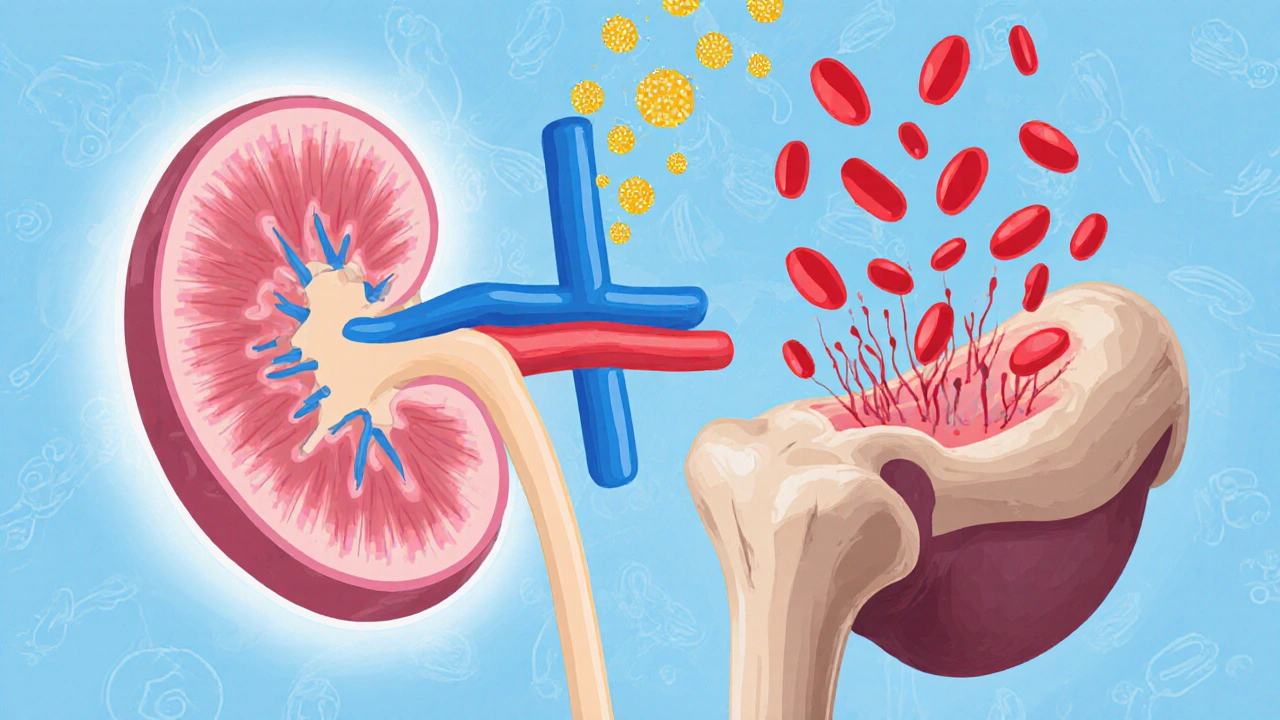
They also shape care for dialysis, a life-sustaining treatment for people whose kidneys have failed. KDIGO tells clinics how often to monitor blood levels, what kind of access (like fistulas vs. catheters) to prioritize, and how to reduce infection risk. Even something as simple as how to manage anemia in kidney patients—like when to start iron or erythropoietin—comes straight from these guidelines. And because kidney disease often overlaps with heart problems, diabetes, and bone disorders, KDIGO ties into other areas too. You’ll see connections in posts about statin use in kidney patients, drug interactions in dialysis, or how certain meds affect bone density in people with CKD.
These guidelines get updated regularly as new studies come out. That’s why you’ll find posts here comparing old and new recommendations, explaining why a drug like Vastarel might be used differently in kidney patients, or how genetic factors affect how people respond to kidney medications. KDIGO doesn’t just tell doctors what to do—it helps patients understand why their treatment plan looks the way it does. Whether you’re dealing with early-stage kidney disease, preparing for dialysis, or just trying to avoid it, these guidelines are the backbone of your care. Below, you’ll find real-world breakdowns of how they apply to medications, testing, and daily management—no jargon, no fluff, just what matters for your health.
Anemia in Kidney Disease: How Erythropoietin and Iron Therapy Work Together
Anemia in kidney disease is caused by low erythropoietin and poor iron use. Learn how IV iron and ESA therapy work together to safely raise hemoglobin, improve energy, and reduce risks - with updated 2025 guidelines.
View more