 12
Nov,2025
12
Nov,2025
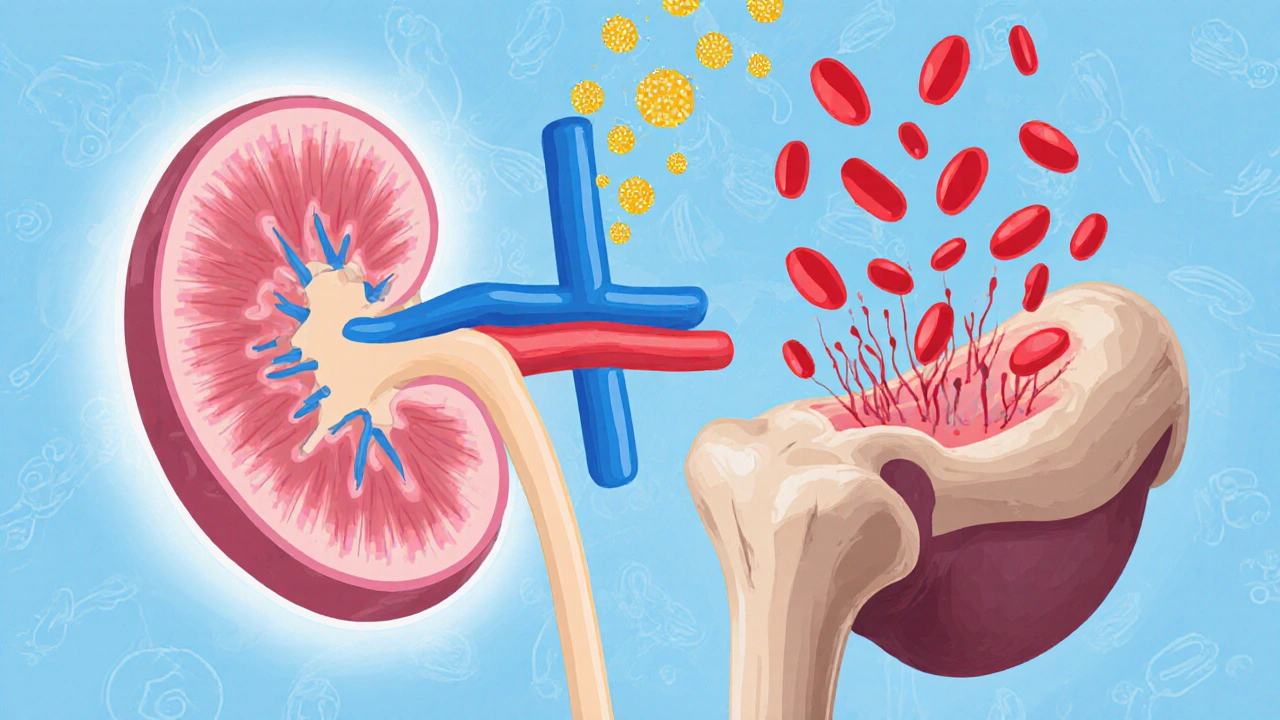
When your kidneys aren’t working right, they don’t make enough of a hormone called erythropoietin. That’s a big problem because this hormone tells your bone marrow to make red blood cells. Without enough of them, you get tired, short of breath, and weak - even if you’re sleeping well and eating fine. This isn’t just regular anemia. It’s anemia in kidney disease, a common and serious complication that affects more than half of all people with chronic kidney disease (CKD). The good news? We know how to treat it - and the treatment has changed a lot in the last 10 years.
Why Kidney Disease Causes Anemia
Your kidneys don’t just filter waste. They also produce erythropoietin, a hormone that signals your body to create red blood cells. When kidney function drops below 30%, erythropoietin production falls sharply. But that’s only half the story. In kidney disease, your body also struggles to use iron properly. Inflammation from damaged kidneys triggers a protein called hepcidin, which locks iron inside your liver and immune cells. Even if you have plenty of iron in your body, your bone marrow can’t get to it. So you end up with low red blood cells - not because you’re missing iron, but because your body won’t let you use it.
This is called functional iron deficiency. It’s different from the kind you get from heavy periods or poor diet. In kidney disease, taking an iron pill often does nothing. That’s why doctors don’t just reach for oral supplements anymore.
What Is Erythropoietin Therapy?
In 1989, doctors got a powerful new tool: synthetic erythropoietin. Made in labs, drugs like epoetin alfa and darbepoetin alfa mimic the natural hormone and trick your bone marrow into making more red blood cells. These are called erythropoiesis-stimulating agents, or ESAs. Today, they’re the backbone of treatment for anemia in CKD.
ESAs are given either as shots under the skin (subcutaneous) or into a vein (intravenous). For people on dialysis, IV is standard because it’s easier to give during treatment. For those not yet on dialysis, subcutaneous shots work just as well and are often preferred.
Most patients see their hemoglobin rise by 1 to 2 grams per deciliter within 2 to 6 weeks. That’s enough to go from feeling exhausted to being able to walk the dog, play with grandkids, or get through a workday without needing a nap.
But here’s the catch: pushing hemoglobin too high is dangerous. Studies like the TREAT trial showed that targeting levels above 13 g/dL increased stroke risk by 32%. That’s why current guidelines - like the 2025 KDIGO draft - recommend keeping hemoglobin between 10 and 11.5 g/dL. Higher than that, and the risk of clots, high blood pressure, and heart problems goes up. Lower than 10, and fatigue and poor quality of life return.
Iron Therapy: Why Oral Doesn’t Work and IV Does
Iron therapy is not optional. It’s required - before and during ESA treatment. If your iron levels are low, ESAs won’t work well. You’ll need higher doses, and you’ll still feel tired. That’s called ESA hyporesponsiveness, and it affects about 1 in 10 patients.
So why not just take an iron pill? Because in kidney disease, your gut barely absorbs oral iron. Studies show only 30-40% of the iron from a pill gets into your bloodstream. The rest passes through. Meanwhile, inflammation blocks what little does get absorbed.
That’s why intravenous (IV) iron is now standard. Iron sucrose, ferric carboxymaltose, and ferumoxytol are given directly into the vein. They bypass the gut entirely. One dose of 200 mg can raise ferritin levels in days. A full course of 1,000 mg over 4 weeks typically boosts hemoglobin by 1.5 g/dL - faster and more reliably than any pill.
Doctors check two numbers to decide if you need IV iron:
- Ferritin: Below 100 mcg/L means you’re out of iron. Between 100 and 500 mcg/L with low transferrin saturation (TSAT), you have functional deficiency.
- Transferrin Saturation (TSAT): Below 20-30% means your body can’t move iron to where it’s needed.
KDIGO 2025 recommends starting IV iron when ferritin is ≤500 mcg/L and TSAT ≤30%, even if you’re not severely low. Many nephrologists now give 400 mg monthly to hemodialysis patients as routine - not just when labs look bad.
Side effects? Some people get a metallic taste or feel flu-like after the infusion. Rarely, there’s an allergic reaction - but that happens in less than 1 in 500 treatments. The risk of iron overload is real, though. If ferritin climbs above 800 mcg/L, doctors hold off on more IV iron.

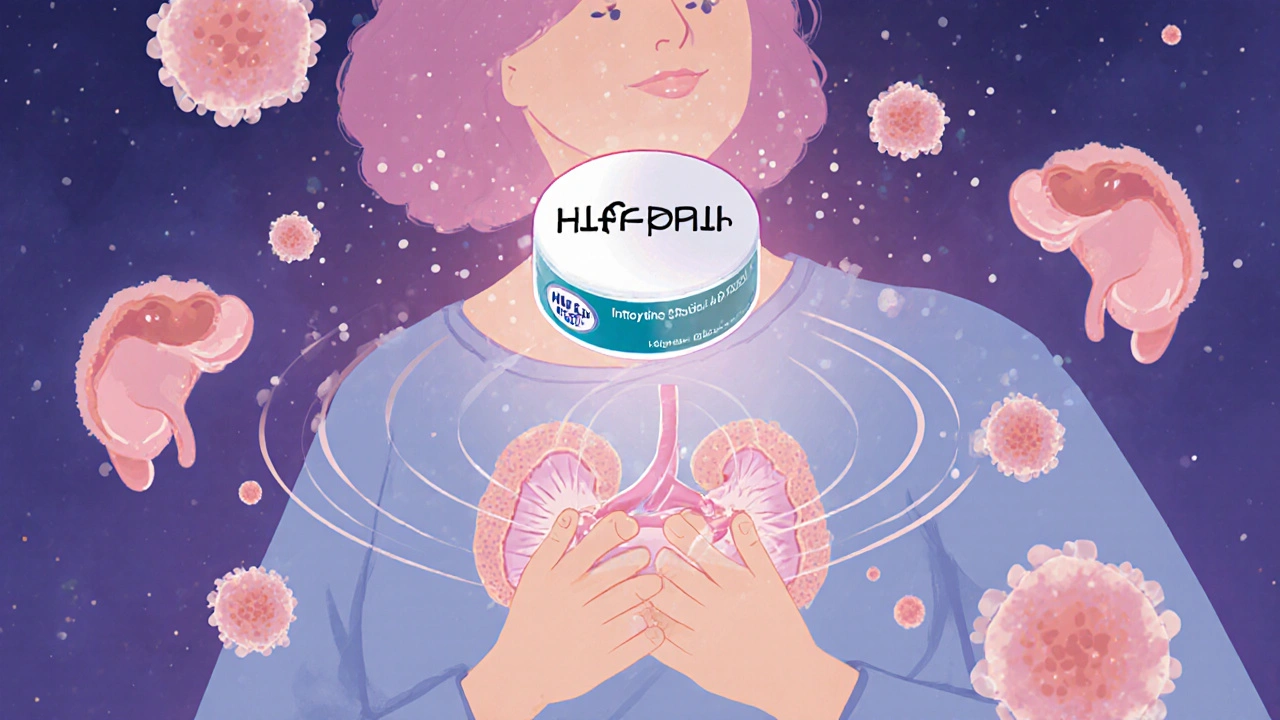
What Are HIF-PHIs? The New Oral Option
There’s a new player on the field: HIF-PH inhibitors. These are oral pills - roxadustat, daprodustat, and vadadustat - that work differently than ESAs. Instead of replacing the hormone, they trick your body into making more of it naturally. They also improve iron absorption and reduce hepcidin, so your body uses iron better.
Roxadustat got FDA approval in December 2023 after years of safety reviews. It’s the first oral HIF-PHI approved in the U.S. for CKD anemia. Early data shows it raises hemoglobin as well as ESAs, with fewer spikes in blood pressure and possibly lower cardiovascular risk.
But it’s not perfect. There are still concerns about tumor growth in people with a history of cancer - which is why the FDA put it on hold from 2018 to 2020. It’s also more expensive than ESAs. Right now, it’s used mostly for patients who can’t tolerate injections or have unstable blood pressure.
For now, ESAs remain the first choice. But HIF-PHIs are changing the game. In the next 5 years, they could become the go-to for many patients - especially those not on dialysis.
How Treatment Works in Real Life
Here’s what a typical treatment plan looks like:
- Diagnose: Check hemoglobin. If it’s below 13 g/dL for men or 12 g/dL for women, test ferritin and TSAT.
- Fix iron first: If ferritin is under 500 mcg/L and TSAT under 30%, start IV iron. Don’t wait.
- Start ESA if needed: If after 4-8 weeks of iron, hemoglobin is still below 10 g/dL, begin ESA therapy.
- Monitor and adjust: Check hemoglobin every 2-4 weeks. Adjust ESA dose by 25% up or down based on trends. Don’t rush to hit 12 g/dL.
- Reassess every 3 months: Look at iron stores, inflammation markers, and how you’re feeling. Are you sleeping better? Can you walk up stairs without stopping?
Many patients report feeling like themselves again within 4 weeks. One 62-year-old man with diabetes and CKD saw his hemoglobin jump from 8.2 to 10.5 g/dL in 8 weeks - just with weekly IV iron and a low dose of darbepoetin. He started playing golf again.
But not everyone responds. About 10% of patients don’t improve even with iron and ESA. That’s called ESA hyporesponsiveness. Causes? Undiagnosed inflammation, aluminum toxicity (rare now), vitamin B12 or folate deficiency, or blood loss. Your doctor will dig deeper if you’re not improving.
What Doctors Are Saying
There’s been a major shift in thinking. Ten years ago, many doctors aimed for hemoglobin levels of 12-13 g/dL - thinking more red cells meant more energy. Now, we know that’s harmful. The KDIGO 2025 guidelines, backed by 27 clinical trials, say clearly: don’t push it above 11.5 g/dL.
Dr. Marcello Tonelli, who led the KDIGO guideline group, put it bluntly: “The old goal of normalizing hemoglobin is outdated. We’re not curing anemia - we’re managing it safely.”
And it’s working. Since 2011, when Medicare started bundling anemia care into dialysis payments, ESA use dropped 35%. Fewer patients are being pushed too high. Fewer strokes. Fewer heart attacks.
Still, a 2018 study found that 22% of U.S. dialysis patients still have hemoglobin above 11 g/dL. Why? Habit. Lack of awareness. Fear of fatigue. But the data is clear: lower is safer.
What to Expect as a Patient
If you’re starting treatment:
- You’ll get IV iron every 1-4 weeks - usually during dialysis or at an infusion center.
- ESA injections might be weekly or every other week. Some patients learn to give themselves shots at home.
- You’ll have blood tests every 2-4 weeks until things stabilize.
- You might feel a bit tired at first as your body adjusts. That’s normal.
- Keep track of your blood pressure. ESAs can raise it. Your doctor may need to adjust your hypertension meds.
Side effects to watch for:
- High blood pressure (most common)
- Headache, dizziness
- Injection site pain or redness
- Metallic taste or nausea after IV iron
- Flu-like symptoms after infusion
If you feel unusually short of breath, have chest pain, or notice swelling in your legs, call your doctor. These could be signs of a clot or heart issue.
The Future of Anemia Treatment
What’s next? Personalized medicine. Researchers are testing machine learning models that predict exactly how much ESA or iron you need based on your weight, age, inflammation levels, and past responses. One Mayo Clinic pilot cut ESA dose variability by 22%.
Another promising area? Minihepcidins - drugs that block the hepcidin protein and free up iron. These could make IV iron even more effective or reduce how often you need it.
For now, the standard remains: fix iron first, use ESA carefully, keep hemoglobin between 10 and 11.5, and listen to how you feel. Not what the number says - what your body tells you.
Key Takeaways
- Anemia in kidney disease is caused by low erythropoietin and poor iron use - not just low iron.
- Oral iron rarely works. IV iron is the standard of care for most CKD patients.
- ESAs raise hemoglobin but must be used carefully. Never aim above 11.5 g/dL.
- HIF-PHIs like roxadustat are new oral options with potential benefits, but not for everyone.
- Regular monitoring and individualized treatment beat one-size-fits-all targets.
Can I treat anemia in kidney disease with just iron pills?
No. Oral iron is poorly absorbed in kidney disease due to inflammation and high hepcidin levels. Studies show only 30-40% of the iron from pills reaches your bloodstream. IV iron is far more effective and is the recommended first-line treatment for most patients with chronic kidney disease.
Why is my hemoglobin target 10-11.5 g/dL and not higher?
Studies like the TREAT trial showed that pushing hemoglobin above 11.5 g/dL increases the risk of stroke, heart attack, and blood clots. While higher levels might seem better for energy, the dangers outweigh the benefits. Current guidelines from KDIGO and other major organizations recommend staying within 10-11.5 g/dL to balance quality of life and safety.
What happens if I miss an IV iron dose?
Missing one dose won’t cause immediate problems, but it can lead to ESA hyporesponsiveness over time. If your iron stores drop, your body won’t respond well to erythropoietin therapy, and your hemoglobin may fall. Your doctor will likely check your ferritin and TSAT levels and reschedule your infusion as soon as possible.
Are HIF-PHIs better than ESAs?
HIF-PHIs like roxadustat offer the advantage of being oral pills and may improve iron use better than ESAs. They also tend to cause less spike in blood pressure. However, they’re newer, more expensive, and carry concerns about tumor growth in people with cancer history. ESAs remain the first-line treatment for most patients, but HIF-PHIs are a strong alternative - especially for those who dislike injections or have unstable blood pressure.
How long does it take to feel better after starting treatment?
Most patients report improved energy and less shortness of breath within 2 to 4 weeks of starting IV iron and/or ESA therapy. Full benefits usually appear by 6 to 8 weeks. If you don’t feel better after 8 weeks, your doctor will check for other causes like inflammation, vitamin deficiencies, or blood loss.




man i remember when my mom was on dialysis and they kept giving her iron pills like it was gonna fix everything. she’d get so frustrated because she was still so tired. then they switched to IV iron and it was like night and day. she started walking around the block again, even got back into her garden. i wish more people knew how big a difference this makes. it’s not just a lab number - it’s your life back.
IV iron > pills. end of story.
as someone who’s been through this with my dad - the shift from chasing hemoglobin numbers to focusing on quality of life is huge. i used to think ‘higher is better’ until i saw him have a stroke scare because his doc pushed him to 12.8. now they keep him at 10.7 and he’s got more energy than he has in years. it’s not about fixing numbers, it’s about letting people live. glad the guidelines finally caught up.
the part about hepcidin locking up iron was a lightbulb moment for me. i always thought anemia meant ‘not enough iron’ - but in kidney disease, it’s more like ‘iron’s trapped in the basement and the door’s locked’. that’s why pills don’t work. and now they’ve got these new oral drugs that basically pick the lock? mind blown. i’ve been reading up on roxadustat - it’s wild that we’re finally moving away from needles. i just hope insurance covers it. my cousin’s on it and she’s paying $800 a month out of pocket.
you ever wonder if all this is just big pharma keeping people hooked? IV iron, ESAs, HIF-PHIs - all expensive. what if the real fix was just clean water, less processed food, and less stress? but no, we need fancy drugs and monthly infusions. and don’t get me started on how they say ‘don’t push hemoglobin above 11.5’ - but then they still test it every two weeks like it’s some kind of race. i think they’re more scared of lawsuits than patients getting tired.
let’s be real - this entire post reads like a pharmaceutical ad. ‘IV iron is standard’? sure, if you’re getting paid per infusion. ‘ESAs must be used carefully’? yeah, because they cause hypertension, strokes, and clots. and now we’re supposed to believe roxadustat is the golden child? the FDA held it for two years for a reason. this isn’t medicine - it’s a revenue stream disguised as care. and don’t even get me started on ‘monitoring every 2-4 weeks.’ who has that kind of time? or money?
iv iron? sounds like a scam. my uncle got it and he got dizzy and threw up for a week. why not just eat more spinach? or take a vitamin? i think doctors just wanna give shots so they can bill more. also why do they keep changing the rules? first it was 12, now it’s 11.5, next year it’ll be 9.5. who even knows what’s real anymore?
thank you for writing this. my sister’s been on dialysis for 3 years and this is the first time someone explained it in a way that didn’t make me feel dumb. i used to panic every time her hemoglobin dipped, but now i understand it’s not about hitting a number - it’s about her feeling okay. we’ve been doing weekly IV iron and she’s finally sleeping through the night. she even started knitting again. small wins matter.
what’s the data on long-term iron overload with monthly IV iron? i’ve read that ferritin above 800 is a red flag, but what happens if someone’s on it for 5+ years? do we know the risks of cumulative iron exposure in the liver or heart? just curious if there’s any longitudinal studies.
the phrase ‘functional iron deficiency’ is technically inaccurate - it’s not a deficiency, it’s a dysregulation. iron is present, but sequestered by hepcidin-mediated blockade. precision in language matters, especially in clinical contexts. also, the 2025 KDIGO draft has not been formally published - citing it as if it’s final is misleading. please clarify sources.
As a nephrologist with over two decades of experience managing anemia in chronic kidney disease, I feel compelled to offer some context that may not be immediately apparent from this otherwise well-written summary. While the narrative emphasizes the efficacy of IV iron and ESA therapy, we must also acknowledge the systemic challenges that patients face - particularly those in underserved communities where access to infusion centers is limited, transportation is unreliable, and insurance prior authorizations delay treatment by weeks. The ideal algorithm presented here - diagnose, fix iron, start ESA, monitor - assumes a level of healthcare infrastructure that simply doesn’t exist for many. Furthermore, while HIF-PHIs represent a promising frontier, their cost and the lingering oncological concerns mean they are not yet viable for broad population use. We are making progress, yes - but we must not confuse clinical guidelines with equitable care. The real innovation isn’t just in the drugs - it’s in how we deliver them.