FDA Exclusivity: What It Means for Generic Drugs and Your Medication Choices
When you hear FDA exclusivity, a period of market protection granted by the U.S. Food and Drug Administration to brand-name drug makers to incentivize innovation. Also known as drug market exclusivity, it doesn't mean a patent—it's a separate legal shield that blocks generics from entering the market, even after the patent expires. This is why your prescription might cost $300 one month and $30 the next—because FDA exclusivity just ran out.
FDA exclusivity isn't one-size-fits-all. It comes in different flavors: new chemical entity exclusivity, a five-year protection for drugs with active ingredients never approved before, or orphan drug exclusivity, seven years for drugs treating rare diseases affecting fewer than 200,000 Americans. Then there’s pediatric exclusivity, an extra six months added if the manufacturer studies the drug in children. These aren’t just legal jargon—they directly impact how fast you can get a cheaper version of your medicine.
Complex generics, like inhalers or injectables, often face extra hurdles even after exclusivity ends. Proving they work the same as the brand isn’t just about matching ingredients—it’s about matching how the drug behaves in your body. That’s why some generics take years to appear, even when the exclusivity clock hits zero. The FDA doesn’t approve them until they meet strict bioequivalence standards, which is why some drug manufacturers fight for years over small formulation differences.
You’ll see this play out in posts about drugs like bupropion, trimetazidine, or carbimazole. When a brand like Wellbutrin or Vastarel loses exclusivity, cheaper versions flood the market. But not all generics are equal. Some work great. Others cause side effects because they’re not exact copies. That’s why reading FDA safety communications and understanding drug interactions becomes critical when switching from brand to generic.
FDA exclusivity isn’t about keeping drugs expensive—it’s meant to reward innovation. But the system has gaps. Some companies extend exclusivity by making tiny changes to old drugs, a tactic called "evergreening." Others delay generics by filing lawsuits or exploiting loopholes. That’s why knowing when exclusivity ends helps you plan ahead. If your medication is due to go generic soon, talk to your doctor now. Ask about alternatives. Check if your insurance will cover the new version.
What you’ll find below are real-world examples of how FDA exclusivity shapes your options. From how long it takes for a generic version of raltegravir to hit shelves, to why some statins still cost more than others, these posts show you how the system works—and how to use it to your advantage. No fluff. No theory. Just what you need to know before your next prescription.
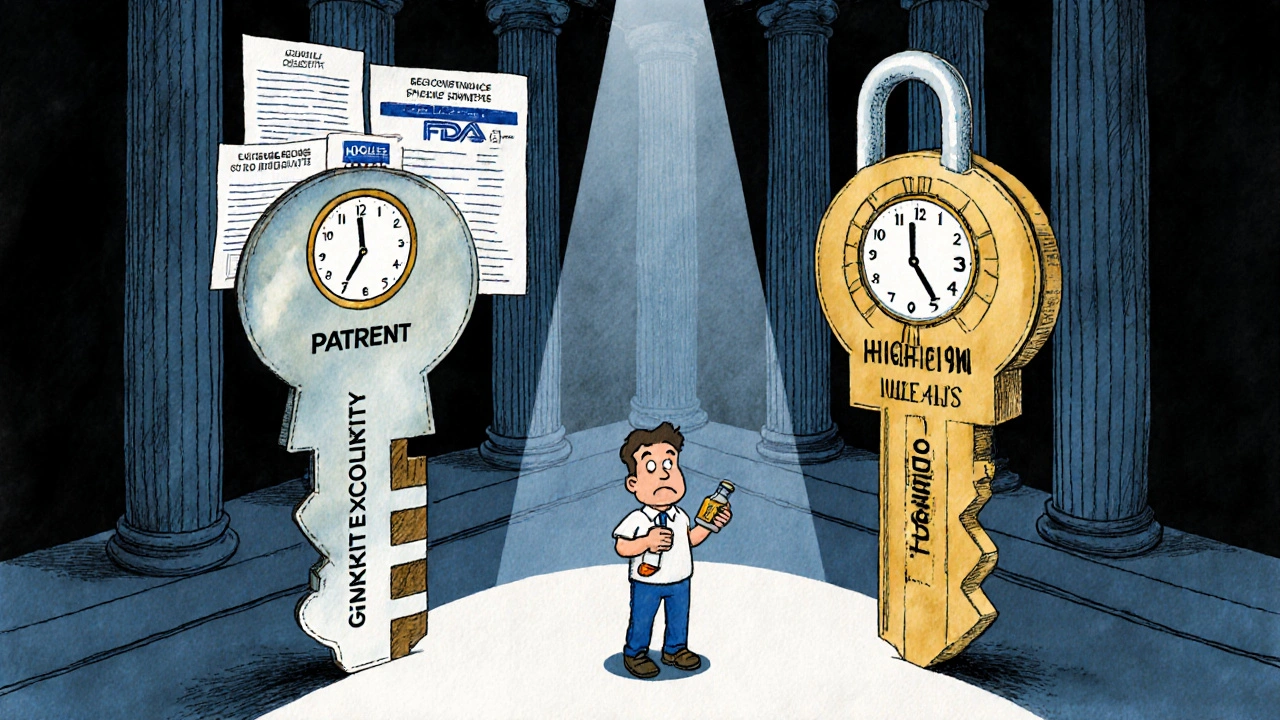
Patent Exclusivity vs Market Exclusivity: What’s the Real Difference for Drug Prices?
Patent exclusivity and market exclusivity are two different legal tools that protect brand-name drugs. One comes from the patent office, the other from the FDA. Understanding the difference explains why some drugs stay expensive long after patents expire.
View more