Drug Interaction: What You Need to Know to Stay Safe
When you take more than one medication, your body doesn’t always treat them like separate guests—it sees them as a party where someone might sneak in a dangerous mix. A drug interaction, a change in how a drug works when combined with another drug, food, or supplement. Also known as medication interaction, it can make a drug stronger, weaker, or trigger side effects you never saw coming. This isn’t just a footnote on a prescription label—it’s a real risk that sends tens of thousands to the ER every year.
Think about antidepressants, medications used to treat depression and anxiety like SSRIs. Mixing them with alcohol or certain painkillers can spike serotonin levels to dangerous levels. Or consider NSAIDs, nonsteroidal anti-inflammatory drugs like ibuprofen and naproxen—common for headaches or sore muscles. Take them with blood pressure meds, and they can cancel out the treatment, leaving your heart vulnerable. Even something as simple as grapefruit juice can wreck how your body breaks down statins, turning a routine heart pill into a liver or muscle hazard.
These aren’t rare edge cases. The FDA’s FAERS database, a public system that collects reports of adverse events from patients and doctors shows that over 70% of adults take at least one prescription drug, and nearly 40% take three or more. That’s a lot of chances for something to go wrong. Your pharmacist isn’t just handing out pills—they’re your last line of defense. They see your full list of meds, including OTC stuff like antihistamines and acetaminophen, and know which combinations are ticking time bombs.
You don’t need to be a scientist to protect yourself. Start by keeping a simple list: every pill, patch, vitamin, or herbal tea you take. Bring it to every appointment. Ask: "Could this interact with anything else I’m on?" If your prescription comes with a sticker that says "Avoid alcohol" or "May cause dizziness," don’t ignore it. Those aren’t suggestions—they’re warnings backed by real cases of people ending up in the hospital.
Some interactions are obvious—like mixing opioids with sleeping pills. Others sneak up on you. A common cold medicine with diphenhydramine might make your anxiety meds less effective. A daily magnesium supplement could reduce how well your antibiotic works. And if you’re on blood thinners, even a sudden change in your leafy green intake can throw off your dosage. It’s not about fear—it’s about awareness.
The posts below give you real, practical tools to stay in control. You’ll find guides on how to read your prescription labels, what those weird symbols mean, how to check for interactions yourself using free FDA tools, and why pharmacists are your secret weapon against dangerous mixes. You’ll also see how things like fluoxetine, statins, and blood pressure meds behave when they meet other substances. No fluff. No jargon. Just what you need to know before you swallow that next pill.
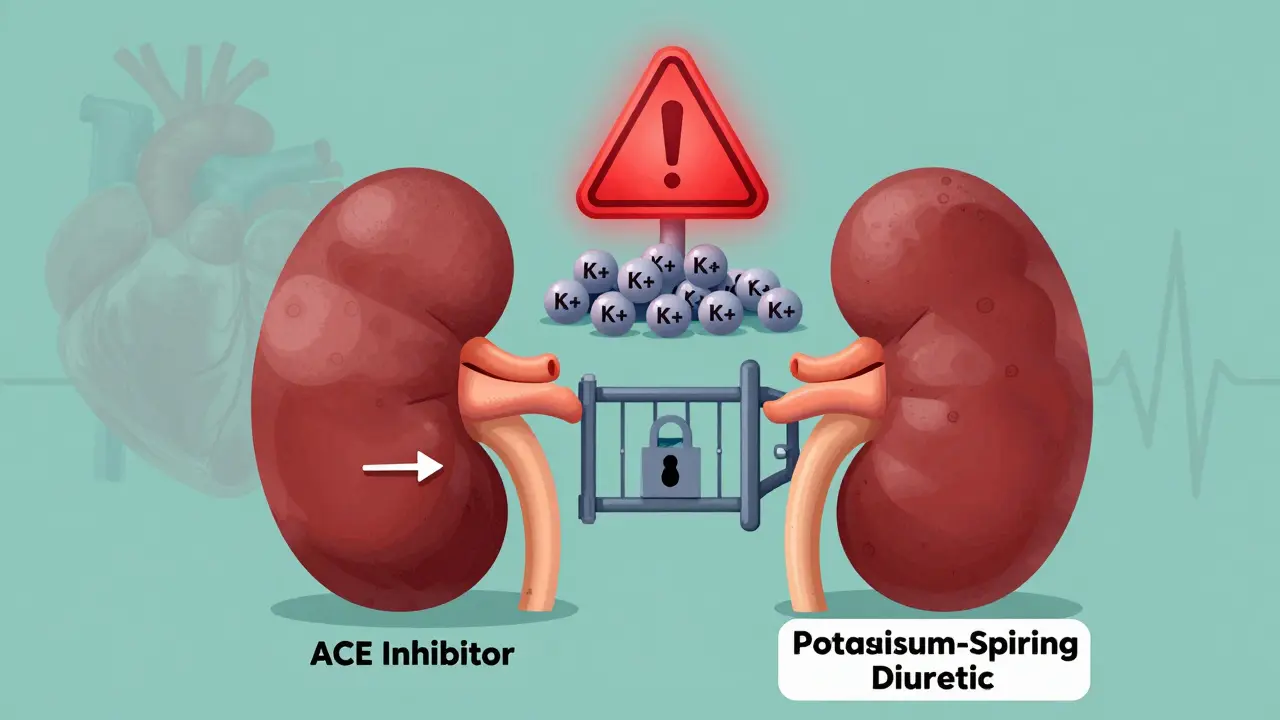
ACE Inhibitors and Potassium-Sparing Diuretics: Understanding the Hyperkalemia Risk
Combining ACE inhibitors with potassium-sparing diuretics can dangerously raise potassium levels, leading to life-threatening heart rhythm problems. Learn who’s at risk, how to monitor it, and what to do if your levels climb too high.
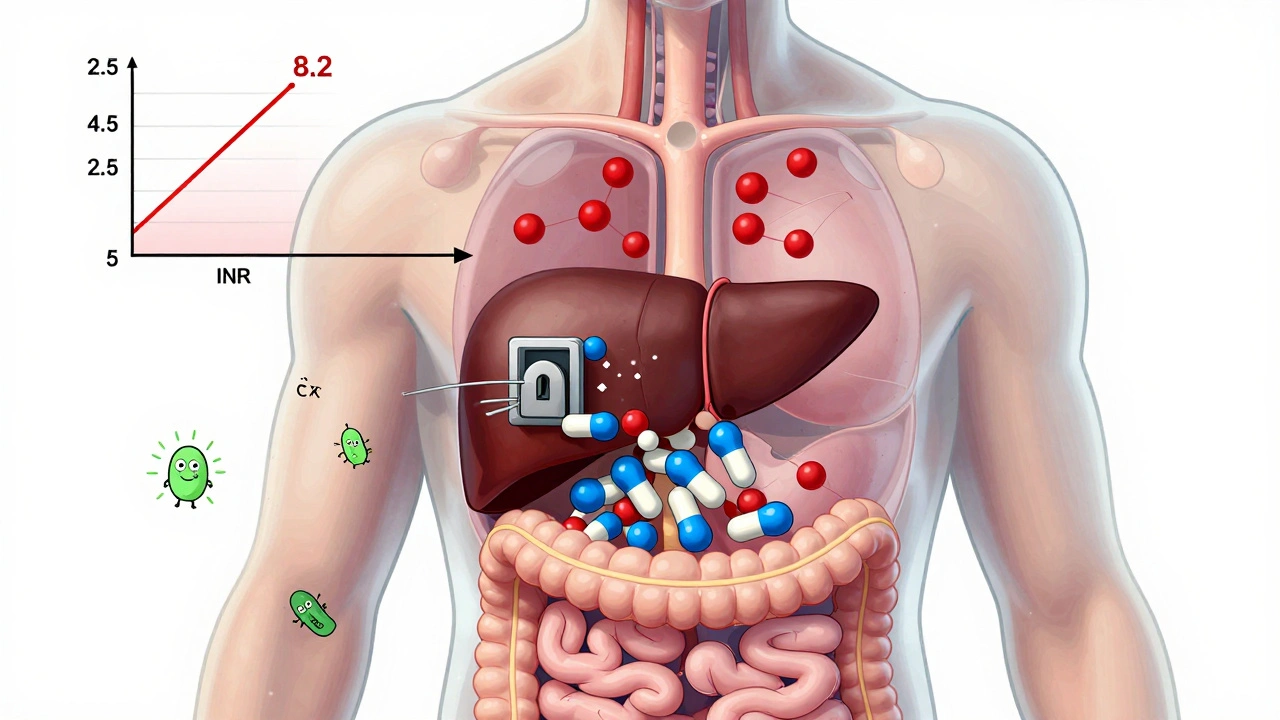
View moreWarfarin and Antibiotics: How Common Drugs Can Spike Your INR Risk
Warfarin and certain antibiotics can dangerously raise your INR, increasing bleeding risk. Learn which antibiotics are risky, why the delay matters, and how to protect yourself with timely testing.
View more