 16
Jan,2026
16
Jan,2026
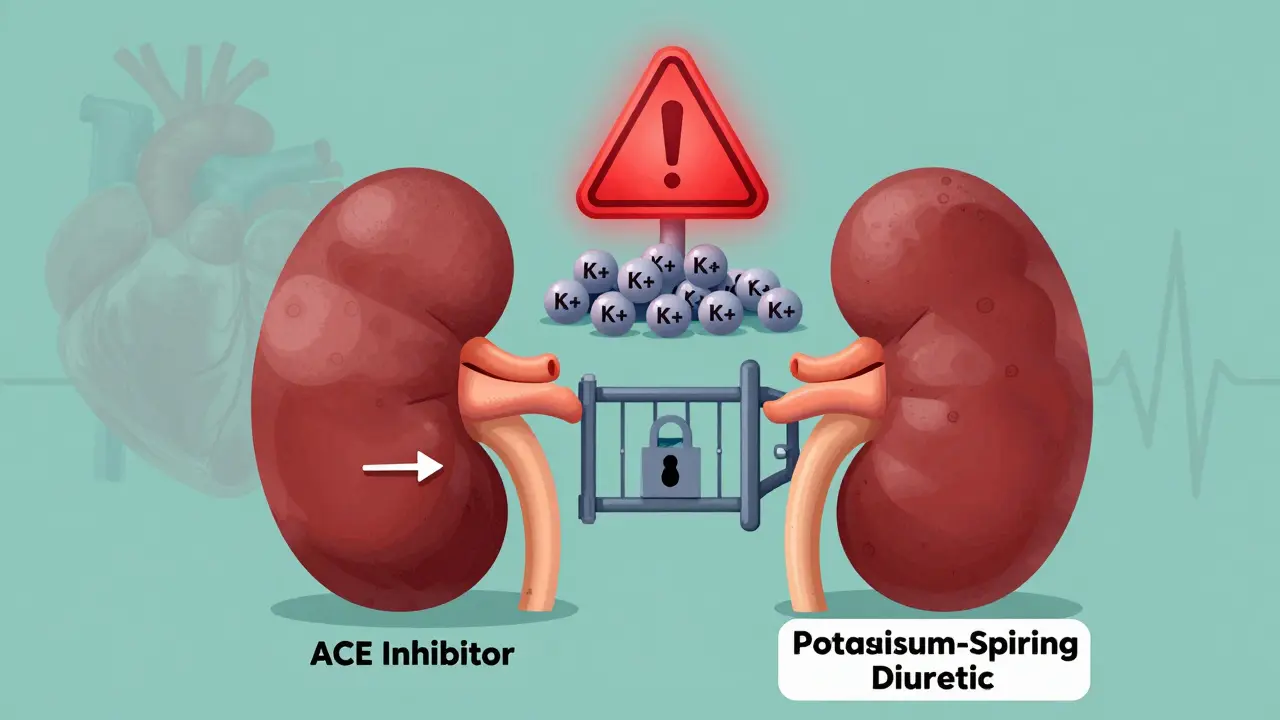
When you take an ACE inhibitor for high blood pressure or heart failure, you’re getting a powerful tool that protects your heart and kidneys. But if your doctor adds a potassium-sparing diuretic-like spironolactone or eplerenone-to that mix, you might be walking into a hidden danger zone: hyperkalemia. That’s when your blood potassium levels climb too high, and it can stop your heart without warning.
How These Two Drugs Work Together-And Why That’s Dangerous
ACE inhibitors, such as lisinopril or enalapril, lower blood pressure by blocking the angiotensin-converting enzyme. This reduces angiotensin II, which in turn lowers aldosterone. Aldosterone is the hormone that tells your kidneys to push out potassium. Less aldosterone? Less potassium gets flushed out. Your body holds onto it. Now add a potassium-sparing diuretic. These drugs-spironolactone, eplerenone, amiloride, triamterene-don’t make you pee more salt and water like hydrochlorothiazide does. Instead, they block the same final step in the kidney that aldosterone controls. Spironolactone and eplerenone block the aldosterone receptor. Amiloride and triamterene plug the sodium channels that help pull potassium out. So now you’ve got two drugs hitting the same exit door for potassium, from two different angles. The result? Your kidneys stop letting potassium leave. And if you’re already older, have diabetes, kidney disease, or heart failure, your kidneys aren’t working at full strength to begin with. That’s when potassium starts building up like traffic on a highway with no exits.Who’s at the Highest Risk?
Not everyone on this combo will get high potassium. But some people are sitting right on the edge. The Cleveland Clinic gives doctors a simple scoring system to spot them:- eGFR under 60 (kidney function down) = 2 points
- Baseline potassium over 4.5 mmol/L = 2 points
- Diabetes = 1 point
- Heart failure = 1 point
- On a potassium-sparing diuretic or ACE inhibitor = 2 points
What Does High Potassium Actually Do to Your Body?
Potassium isn’t just a mineral. It’s what makes your heart beat. Too little, and your heart stumbles. Too much, and it can go haywire. Hyperkalemia is defined as serum potassium above 5.0 mmol/L. Levels above 6.0 mmol/L are dangerous. At that point, your heart’s electrical system starts misfiring. You might not feel anything at first. No chest pain. No shortness of breath. Just a silent, slow creep toward cardiac arrest. Electrocardiogram (ECG) changes show up before symptoms: tall, peaked T-waves, flattened P-waves, widened QRS complexes. If potassium keeps rising, you can get ventricular fibrillation or asystole-both fatal without immediate treatment. And here’s what most people don’t realize: many of these deaths are preventable. A 1998 study of over 1,800 patients found 11% developed hyperkalemia on ACE inhibitors alone. That number climbs even higher when combined with potassium-sparing diuretics. Yet, only 57% of patients with high potassium had their levels rechecked within 30 days. That’s a dangerous gap.
Why Do Doctors Still Prescribe This Combo?
It sounds counterintuitive. Why risk your life with a combo that can stop your heart? Because the benefits are huge. For people with heart failure or diabetic kidney disease, ACE inhibitors reduce death risk by up to 26%. Spironolactone cuts heart failure hospitalizations by nearly 30%. Stopping them because of high potassium can be just as deadly as the high potassium itself. That’s why the goal isn’t to avoid the combo-it’s to manage it safely. The American Heart Association and European Society of Cardiology both say: monitor, don’t avoid.How to Stay Safe: Monitoring and Management
If you’re on this combo, here’s what you need to do:- Get your first potassium test 1 to 2 weeks after starting the combo.
- Test again at 4 weeks, then every 3 to 6 months if stable.
- If your eGFR is under 60, test monthly for the first 3 months.
- If your potassium hits 5.0-5.5 mmol/L, your doctor should check your diet, kidney function, and meds.
- If it’s above 5.5 mmol/L, they might switch you to a thiazide or loop diuretic (like furosemide) to help flush out potassium.

New Tools to Fight Hyperkalemia
The game has changed in the last five years. Two new drugs-patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma)-are potassium binders. They work in your gut to trap potassium before it enters your bloodstream. In trials, they brought potassium down by 0.8-1.2 mmol/L in 48 hours and let 89% of patients stay on their heart-protecting meds. Even better, SGLT2 inhibitors like dapagliflozin (Farxiga) are now used alongside ACE inhibitors in patients with kidney disease. The DAPA-CKD trial showed they reduce hyperkalemia risk by 32%, likely by improving kidney function and promoting potassium excretion. And in the near future, wearable potassium monitors and genetic tests for WNK1 gene variants may let doctors predict who’s most likely to develop high potassium-before it happens.What to Do If You’re on This Combo
Don’t panic. Don’t stop your meds. But do take action:- Ask your doctor for a potassium test within 2 weeks of starting the combo.
- Keep a food diary for a week-note bananas, potatoes, oranges, salt substitutes, and processed snacks.
- Know your eGFR and creatinine numbers. If your kidney function is declining, ask if your meds need adjusting.
- If your potassium is high, ask about switching from spironolactone to triamterene (lower risk) or adding a low-dose thiazide.
- Ask if you’re a candidate for a potassium binder like Lokelma if you need to stay on your current regimen.
The Bottom Line
ACE inhibitors and potassium-sparing diuretics are lifesavers-for the right people. But they’re also ticking time bombs if you don’t monitor them. Hyperkalemia doesn’t come with a warning siren. It sneaks up quietly. But it’s not unpredictable. With smart testing, diet tweaks, and new medications, you can keep your heart protected without putting your life at risk.The key isn’t avoiding the combo. It’s managing it like a pro.
Can I take potassium supplements if I’m on ACE inhibitors and potassium-sparing diuretics?
No. Taking potassium supplements while on ACE inhibitors and potassium-sparing diuretics is extremely dangerous. These medications already reduce how much potassium your kidneys remove. Adding supplements can push your blood potassium into the life-threatening range (above 6.0 mmol/L). Always check with your doctor before taking any supplement, even over-the-counter ones labeled as "natural."
Is it safer to use ARBs instead of ACE inhibitors with potassium-sparing diuretics?
ARBs (like losartan or valsartan) carry a similar risk of hyperkalemia as ACE inhibitors-sometimes even higher in certain studies. One 2009 study found more cases of hyperkalemia with ARBs, but that was because more ARB users were also on potassium-sparing diuretics. The real issue isn’t the class-it’s the combination. Whether you’re on an ACE inhibitor or ARB, adding a potassium-sparing diuretic increases your risk. Monitor potassium levels regardless of which drug you’re on.
How often should I get my potassium checked?
If you’re on this combo and have risk factors (diabetes, kidney disease, heart failure), get tested within 1-2 weeks of starting, then at 4 weeks, and every 3-6 months if stable. If your eGFR is below 60, check monthly for the first 3 months. If your potassium was ever high, your doctor should test you more often-every 1-2 months-until it’s stable.
Can I eat bananas or potatoes if I’m on this combo?
You can eat them in small amounts, but you need to be careful. One banana has over 400 mg of potassium. A medium potato has about 900 mg. If you’re on this combo, aim to keep your daily potassium intake under 2,900-3,500 mg. Avoid daily consumption of high-potassium foods. Talk to a dietitian about alternatives-like apples, berries, cabbage, and rice-that are lower in potassium but still nutritious.
What if my potassium is high but I feel fine?
Feeling fine doesn’t mean you’re safe. High potassium often causes no symptoms until it’s dangerously high. By the time you feel weakness, irregular heartbeat, or nausea, it may already be life-threatening. That’s why regular blood tests are non-negotiable. Even if you feel perfect, get your levels checked as your doctor recommends. Silent hyperkalemia is what kills people.




Man, this post is like a Netflix doc about your heart slowly screaming in silence 😅
ACE inhibitors + spironolactone = the medical equivalent of stacking two Jenga blocks from opposite sides and hoping the tower doesn’t fall.
I’ve seen patients go from ‘feeling great’ to code blue in 72 hours because no one checked K+ after the script was filled.
Doctors are so focused on ‘protecting the heart’ they forget the heart needs stable electrolytes to even *have* a chance.
It’s not that the combo is bad-it’s that we treat it like a coffee order, not a live wire.
And don’t even get me started on patients buying potassium-rich ‘health’ smoothies after their script.
Bro, your kale smoothie isn’t a virtue signal-it’s a cardiac grenade.
Why do we still let people walk out with this combo and zero education?
It’s not negligence-it’s systemic laziness.
And yeah, Lokelma’s a game-changer, but it’s $800/month. Good luck explaining that to Medicare.
Real talk: we’re playing Russian roulette with a loaded gun and calling it ‘evidence-based care.’
THEY KNOW. THEY KNOW WHAT THEY’RE DOING. 🤡
Big Pharma doesn’t want you to know potassium can KILL you-they want you addicted to the combo so you keep buying the binders.
Look at the timeline-Lokelma came out RIGHT when hyperkalemia deaths spiked.
It’s not medicine-it’s a cash grab wrapped in a stethoscope.
They’ll give you a $300/month pill to fix what they created with a $0.10 pill.
And don’t tell me ‘monitoring’ is safe-when was the last time your doctor called you after a lab result?
It’s all a scam. They profit off your fear.
Stop trusting the system. Your heart is a hostage.
They’re not saving lives-they’re monetizing collapse.
And yes, I’ve seen 3 people die from this. I’m not exaggerating.
THEY WANT YOU WEAK. THEY WANT YOU DEPENDENT.
🚨
Okay but can we just appreciate how *dramatic* this post is?? 😭
Like, yes, hyperkalemia is scary-but so is forgetting to check your tire pressure.
It’s not a horror movie, it’s a chronic condition with a checklist.
My dad’s been on this combo for 5 years, K+ stable, no drama.
He checks his levels, avoids bananas like they’re radioactive, and drinks water like it’s his job.
It’s not magic, it’s just… paying attention.
Also, Lokelma? My cousin takes it. Costs less than her monthly yoga class.
Stop panic-scrolling. Your doctor isn’t trying to kill you. They’re trying to help you live longer.
And yes, bananas are delicious-but maybe eat one a week, not daily.
It’s not rocket science. It’s just… responsibility.
❤️🩺
Listen, I served in the Army. We didn’t have fancy binders or ECG machines.
We had a lab, a needle, and a rule: if your K+ is over 5.5, you get a loop diuretic and a stern look.
Now we’ve got people in the U.S. acting like this is some new, mysterious plague.
It’s not. It’s basic physiology.
Europeans do this better. They test at 7 days, not 14.
And don’t get me started on ‘dietary potassium’-you think eating a banana is ‘natural’?
Back in my day, we ate rice, beans, and chicken. No kale smoothies.
Stop overcomplicating it.
Test. Adjust. Don’t panic.
And for God’s sake, stop blaming Big Pharma.
It’s not a conspiracy-it’s medicine.
And if you can’t follow a simple blood test schedule, maybe you shouldn’t be on this combo.
Simple.
Wow. This is the most comprehensive breakdown I’ve seen since I read that 2021 NEJM meta-analysis on RAAS blockade and electrolyte dynamics.
But let’s be real-most clinicians still treat this like a ‘maybe check it sometime’ thing.
Meanwhile, in the UK, NICE guidelines mandate potassium testing at 7, 14, and 30 days post-initiation.
Here? We wait until the patient shows up with a weird ECG and says ‘I felt weird.’
And yes, I’ve seen patients on Lokelma for 3 years now-$800/month, yes-but they’re alive.
Meanwhile, the guy who refused it? Died at 68 from asystole.
It’s not elitist to value data-it’s just… not American.
Also, SGLT2 inhibitors are the real MVP here.
They don’t just lower K+-they lower mortality.
Why aren’t we prescribing them first?
Because we’re still stuck in the ACE-inhibitor-is-the-gold-standard mindset.
Time to evolve.
And yes, I’ve published on this. Twice.
🧠
Y’all are overthinking this. 😊
My grandma’s on this combo and she’s 82 and hiking every weekend.
She checks her K+ every 4 months, skips the oranges, and drinks her tea.
That’s it.
Don’t let fear turn a life-saving combo into a death sentence.
You got this.
And if you’re scared? Talk to your doctor. They’re not monsters.
❤️ You’re not alone. We’re all just trying to keep our hearts beating.
One lab test at a time. 💪
potassium is a silent killer. no one talks about it. but it kills more than opioids. really.
doctors forget. patients forget. labs forget.
we need alarms. like smoke detectors for blood.
simple.
why not?
its 2025.
we have watches that track heart rate.
why not potassium?
someone should make this.
imagine if your apple watch buzzed: ‘k+ high. call doc.’
game changer.
just sayin.
not a doctor. just a person who lost someone.
😭
Thanks for posting this. I’ve been on this combo for 3 years and never knew how risky it was.
I thought my doctor had it under control.
Just got my K+ checked last week-5.3.
They switched me to a low-dose hydrochlorothiazide and gave me a food list.
Turns out I was eating salt substitute like it was salt.
Whoops.
Anyway, I’m feeling better now.
Just wanted to say… this info saved me.
And yeah, I’ll stop putting banana in my oatmeal.
Thanks for the heads up.
❤️