 14
Jan,2026
14
Jan,2026
Steroid Cataract Risk Calculator
Assess Your Cataract Risk
Enter your steroid treatment details to estimate your risk of developing steroid-induced cataracts. Based on research, certain factors increase risk significantly.
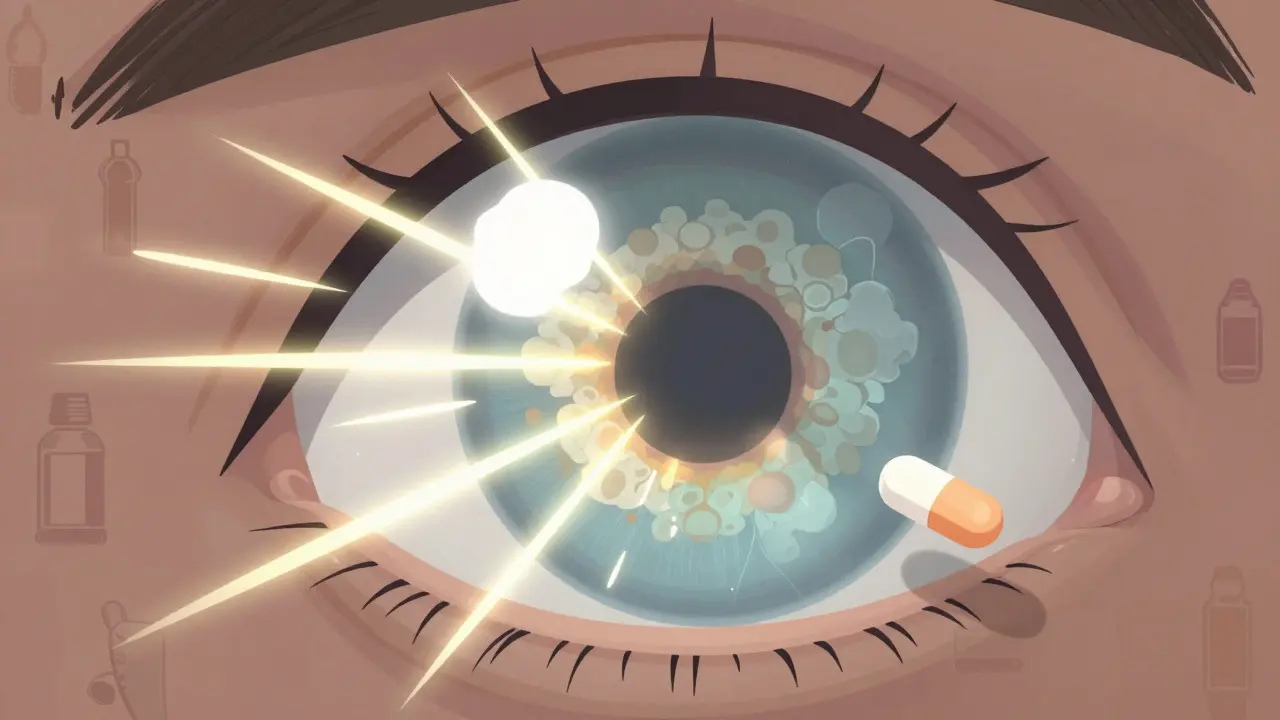
When you’re on steroids for asthma, rheumatoid arthritis, or skin inflammation, you’re focused on feeling better. But there’s a silent side effect many don’t talk about: steroid-induced cataracts. These aren’t the slow, age-related clouding you hear about in older adults. These can show up in just a few months - blurring your vision, making lights glare like halos, and turning colors dull. And if you’re using eye drops, inhalers, or oral steroids long-term, you’re at risk.
What Makes Steroid Cataracts Different?
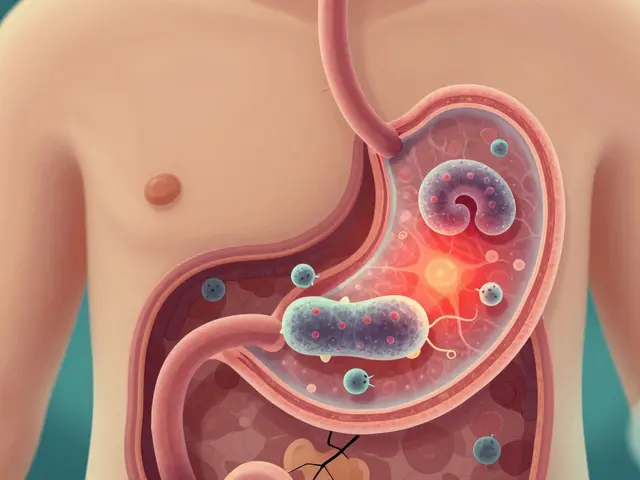
Not all cataracts are the same. Age-related ones form slowly over years, usually in the center of the lens. Steroid-induced cataracts? They grow at the back of the lens - called posterior subcapsular cataracts (PSC). That’s the part of the lens that light passes through first. Even a tiny cloudy spot here can wreck your vision.Why does this happen? Steroids interfere with the proteins inside your lens. Normally, these proteins stay clear and organized. But steroids cause them to clump together like scrambled egg whites. This clumping scatters light instead of letting it focus cleanly on your retina. The result? Blurry vision, ghost images, and trouble reading or driving at night.
What’s worse, steroids also weaken your lens’s natural defenses. Your eye has antioxidants that fight off damage from everyday light and oxygen. Steroids lower those defenses. That means more free radicals build up, and the lens gets damaged faster. Once those proteins are clumped, they don’t unclump. The lens can’t repair itself - it’s like a camera lens that’s permanently fogged.
How Do You Know If You Have One?
The symptoms don’t sneak up. They hit hard and fast:- Blurry vision - especially when reading or doing close work (reported in 92% of cases)
- Glare and halos around lights - streetlights, headlights, or even bright lamps feel blinding
- Colors look washed out - reds seem faded, whites look yellowish
- Double vision in one eye - not because of misaligned eyes, but because the clouded lens splits the light
- Difficulty seeing at night - headlights and streetlights become unbearable
- Reduced peripheral vision - objects at the edge of your sight become harder to spot
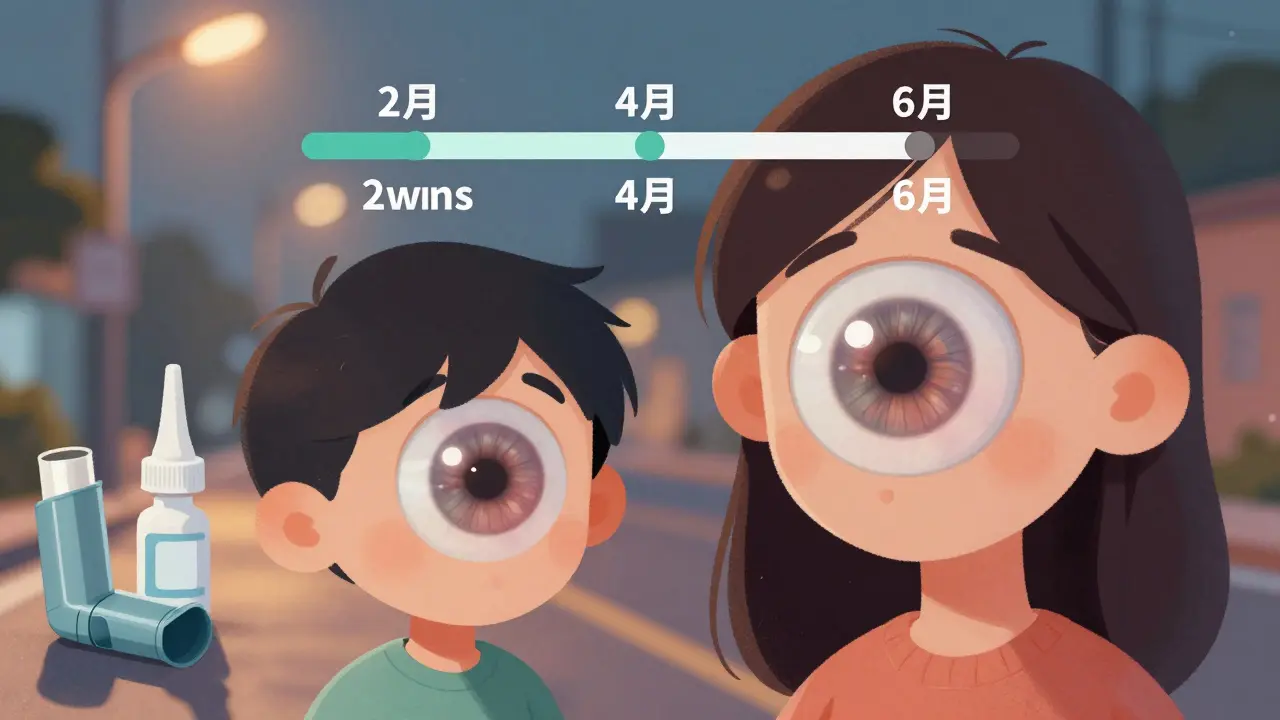
These symptoms often appear within 4 to 6 months of starting steroid therapy. Some people notice changes as early as 2-3 weeks, especially if they’re using high-dose eye drops. If you’ve been on steroids for more than 3 months and suddenly can’t read your phone screen or feel like your glasses are dirty even when they’re clean - get your eyes checked.
Who’s Most at Risk?
It’s not just about how long you’re on steroids. It’s about how much, how you take them, and your body’s sensitivity.- Topical steroids - eye drops, creams, or nasal sprays - carry the highest risk. A 2024 study found they’re 3.2 times more likely to cause cataracts than oral or inhaled forms.
- Dose matters. People using over 2,000mg of beclomethasone (a common inhaled steroid) have a much higher chance of developing cataracts.
- Duration. Four months of continuous use is the tipping point. But some patients show early signs in just 6 weeks.
- Children on long-term steroids for conditions like nephrotic syndrome or asthma are especially vulnerable. Their lenses are still developing and more sensitive to chemical changes.
- Existing eye conditions - if you already have diabetes, uveitis, or an artificial lens (IOL), your risk jumps.
Here’s the twist: 73% of people who knew about steroid cataracts were still using steroids. Knowledge doesn’t stop the risk - because often, the steroids are necessary to keep a life-threatening condition under control.
Can You Reverse It Without Surgery?
Unfortunately, no. Once the protein clumps form, they don’t dissolve. Stopping steroids might slow further damage - but it won’t clear what’s already there. And in many cases, you can’t just quit. Stopping steroids suddenly can trigger a flare-up of your original disease - asthma attacks, autoimmune flares, or even adrenal crisis.The goal isn’t always to stop steroids. It’s to manage the balance. Your doctor might:
- Switch to a lower-potency steroid
- Reduce the dose to the minimum effective level
- Change the delivery method (e.g., switch from eye drops to oral if possible)
- Use steroid-sparing drugs like immunomodulators
There’s no proven supplement or eye drop that reverses steroid cataracts. Some studies are looking at antioxidants like vitamin C or N-acetylcysteine to protect the lens, but nothing’s been confirmed yet. Prevention is the only real tool right now.
How Is It Diagnosed?
Your regular eye exam won’t catch it early. You need a specialist - an ophthalmologist - with a slit-lamp microscope. This tool shines a thin beam of light into your eye and lets the doctor see the exact location and density of the clouding.Early steroid cataracts look like a tiny, pearl-like opacity at the back of the lens. It’s easy to miss if you’re not looking for it. That’s why routine screenings are critical. The Mayo Clinic recommends:
- A baseline eye exam before starting long-term steroid therapy
- Follow-up exams every 3-6 months if you’re on high-dose or long-term steroids
- Immediate exam if you report any vision changes
Many patients don’t realize their blurry vision is from cataracts. They think it’s just aging, tired eyes, or needing new glasses. But if you’re on steroids and your glasses aren’t helping - it’s time for a real eye check.

What’s the Treatment?
When vision drops below 20/40 or interferes with daily life - surgery is the only option. Cataract surgery removes the clouded lens and replaces it with a clear artificial one (IOL). It’s one of the safest and most common surgeries in the world.For steroid-induced cataracts, outcomes are excellent. About 92% of patients regain sharp vision after surgery. But there’s a catch: if you keep using steroids afterward, the new lens can still be at risk. The same protein-damaging process can affect the capsule that holds the new lens, causing a condition called posterior capsular opacification (PCO) - sometimes called a “secondary cataract.”
That’s why post-surgery care matters:
- Continue steroid monitoring - your ophthalmologist will watch for PCO
- Use anti-inflammatory eye drops as prescribed - to reduce swelling and clouding risk
- Report any sudden vision changes - even after surgery
Most people return to normal activities within a week. But if you’re still on high-dose steroids, your recovery might take longer. Your surgeon will coordinate with your prescribing doctor to make sure your systemic condition stays stable during healing.
How to Protect Yourself
You can’t always avoid steroids. But you can reduce your risk:- Ask your doctor: “Is there a lower-dose or non-steroid alternative?”
- If using eye drops, don’t overuse them. Use only as prescribed - even if symptoms improve.
- Use a spacer with inhalers. This cuts down the amount that gets swallowed and absorbed into your system.
- Get regular eye exams - every 6 months if you’re on long-term steroids.
- Keep a log: note the type, dose, and duration of every steroid you’ve taken. Share this with your eye doctor.
Coordination between your rheumatologist, pulmonologist, or dermatologist and your ophthalmologist cuts vision loss risk by 37%, according to 2022 clinical data. Don’t let your eye care be an afterthought.
The Bigger Picture
Steroid-induced cataracts are rising. With more people using steroids for autoimmune diseases, asthma, and even skin conditions, we’re seeing more cases. In the U.S. alone, an estimated 380,000 to 570,000 cataract cases each year are linked to steroid use. Globally, the steroid market is worth over $12 billion - and nearly 1 in 5 of those products are eye drops or nasal sprays.Yet awareness is low. Only 38.6% of people know inhaled steroids can cause cataracts. That’s dangerous. You don’t need to fear steroids. But you do need to respect them. They’re powerful tools - but like any powerful tool, they come with risks you can’t ignore.
If you’re on steroids and your vision is changing - don’t wait. Don’t assume it’s just aging. Get your eyes checked. Early detection means better outcomes. And if surgery is needed - it’s not a failure. It’s a reset. A chance to see clearly again, while still managing the condition that brought you here.
Can steroid-induced cataracts go away on their own?
No. Once the lens proteins clump due to steroid exposure, the damage is permanent. Stopping steroids may prevent further damage, but it won’t reverse the clouding. Surgery is the only way to restore clear vision.
Are steroid eye drops more dangerous than oral steroids for cataracts?
Yes. Topical steroids - especially eye drops - carry a 3.2 times higher risk of causing cataracts compared to oral or inhaled forms. Even small amounts absorbed into the eye can trigger protein changes in the lens. That’s why doctors warn against long-term use of steroid eye drops without regular monitoring.
How long after starting steroids do cataracts usually appear?
Cataracts can develop as early as 2-4 weeks in high-risk cases, but most appear within 4-6 months of continuous use. The longer you’re on steroids - and the higher the dose - the faster they form. This is much faster than age-related cataracts, which take years.
Can children get steroid-induced cataracts?
Yes. Children on long-term steroid therapy - for conditions like nephrotic syndrome, severe asthma, or autoimmune disorders - are at high risk. Their lenses are still developing and more sensitive to steroid-induced protein changes. Regular eye exams are essential for any child on steroids for more than 3 months.
Is cataract surgery safe if I still need to take steroids?
Yes. Cataract surgery is safe even if you continue steroid therapy. However, ongoing steroid use increases the risk of posterior capsular opacification (PCO) after surgery. Your eye doctor will monitor you closely and may prescribe anti-inflammatory drops to reduce this risk. Communication between your surgeon and prescribing doctor is key to managing both your vision and your underlying condition.
Can I prevent steroid-induced cataracts with vitamins or supplements?
No proven supplements exist yet. While some research is exploring antioxidants like vitamin C or N-acetylcysteine to protect the lens, no clinical guidelines support their use for prevention. The only proven strategies are reducing steroid dose, switching delivery methods, and getting regular eye exams.




So let me get this straight-you’re telling me my asthma inhaler is slowly turning my vision into a bad LSD trip? Great. Just great. I’ve been using this thing for five years and now I can’t see the road at night? Thanks, Big Pharma. And don’t even get me started on the $800 eye exam they want me to pay for. I’ll take my chances with blurry vision over bankruptcy.
This is not a medical issue-it’s a corporate conspiracy. Steroids were never meant to be prescribed for asthma. The pharmaceutical industry, in collusion with the American Medical Association and the FDA, has been deliberately promoting steroid use to create a permanent patient base for cataract surgery. Look at the numbers: 380,000 cases a year? That’s not an epidemic-it’s a profit model. And they want you to believe it’s just ‘aging’.
Let’s be real. The whole ‘steroid cataracts’ narrative is overstated. Most people on inhaled steroids never develop them. The real issue is lazy doctors who don’t monitor patients. If you’re on steroids for six months and haven’t seen an ophthalmologist, you’re not a victim-you’re negligent. Also, ‘posterior subcapsular cataracts’? That’s just fancy jargon for ‘your lens got fried’. No need to overcomplicate it.
There’s something profoundly metaphysical about steroid-induced cataracts. The lens-once a vessel of pure, unadulterated light-becomes a prison of scrambled protein, a physical manifestation of the soul’s corrosion under chemical domination. We are not just losing vision; we are losing our ability to perceive truth. The world becomes washed out because the system has washed out our essence. And yet… we keep taking the pills. Isn’t that the tragedy of modern existence?
If you're on steroids and your vision is changing get your eyes checked now not tomorrow not next week now. This isn't optional. This is your sight we're talking about. You don't wait for a heart attack to start exercising. You don't wait for blindness to start protecting your eyes. Do the work. Talk to your doctor. Get the screening. Your future self will thank you
I’m a nurse and I’ve seen this so many times. Patient comes in saying ‘my glasses are dirty’-but their glasses are clean. They’ve been on prednisone for 6 months for lupus. No one told them about the eye risk. I always hand out those pamphlets now. Just a little heads up can save someone’s vision. You don’t need to be scared-just informed.
My mom got steroid cataracts from her eczema cream. She didn’t even know it was possible. She used it for years. Got surgery last year. Now she sees colors like she’s 25 again. It’s wild. The thing is, she didn’t stop the cream-she just switched to a lower dose and got monitored. It’s not about quitting steroids. It’s about managing them smart.
I know someone who went blind after steroid eye drops. They said it was ‘rare’. But then they lost their job because they couldn’t drive. Then their husband left. Then they got depression. Now they’re on disability. And the doctor who prescribed it? Still getting paid. This isn’t medicine. It’s a slow-motion betrayal.
In India, we have a saying: ‘The medicine that saves your breath can steal your sight.’ My cousin’s son has nephrotic syndrome. He’s been on steroids since he was two. His mom takes him for eye checks every three months. She says it’s the only way to keep him safe. We don’t have fancy clinics everywhere, but we know: if you’re giving a child steroids, you owe them eyesight. No excuses.
If you're on long-term steroids and haven't had a dilated eye exam in over six months, you're playing Russian roulette with your vision. It's not fearmongering-it's fact. Schedule the appointment. Bring your steroid log. Ask for a slit-lamp. Be the one who doesn't wait until it's too late. Your eyes are irreplaceable.
The notion that steroid-induced cataracts are ‘common’ is statistically misleading. The actual incidence rate among users is less than 5%. Yet, this article amplifies fear through selective data. Furthermore, the claim that ‘knowledge doesn’t stop the risk’ is both false and dangerous. Informed consent is not a buzzword-it is a medical imperative. The author’s tone suggests incompetence, not awareness.