 27
Jan,2026
27
Jan,2026
Imagine trying to follow a conversation in a busy café, but every time someone speaks from your left side, their voice disappears. You turn your head, lean in, and still miss half the words. This isn’t just background noise-it’s single-sided deafness (SSD). About 1 in 1,000 people live with complete or near-total hearing loss in one ear, while the other ear works normally. It’s not just inconvenient-it’s exhausting. The brain struggles to filter out noise, locate where sounds come from, or understand speech when there’s a person on the deaf side. And yet, many people don’t realize there are real, effective solutions.
What Is Single-Sided Deafness?
Single-sided deafness means you have little to no hearing in one ear, but your other ear hears normally or close to it. It can happen suddenly-after an infection, head injury, or viral illness-or develop slowly over time. Some people are born with it. Others lose hearing after surgery, like removal of a vestibular schwannoma (acoustic neuroma), or from loud noise exposure at work or concerts. The problem isn’t just volume. It’s the head shadow effect. High-frequency sounds like ‘s,’ ‘t,’ and ‘f’ get blocked by your skull before they reach your good ear. In a noisy room, your brain gets overwhelmed trying to sort out what’s important.
CROS Hearing Aids: No Surgery, But Limitations
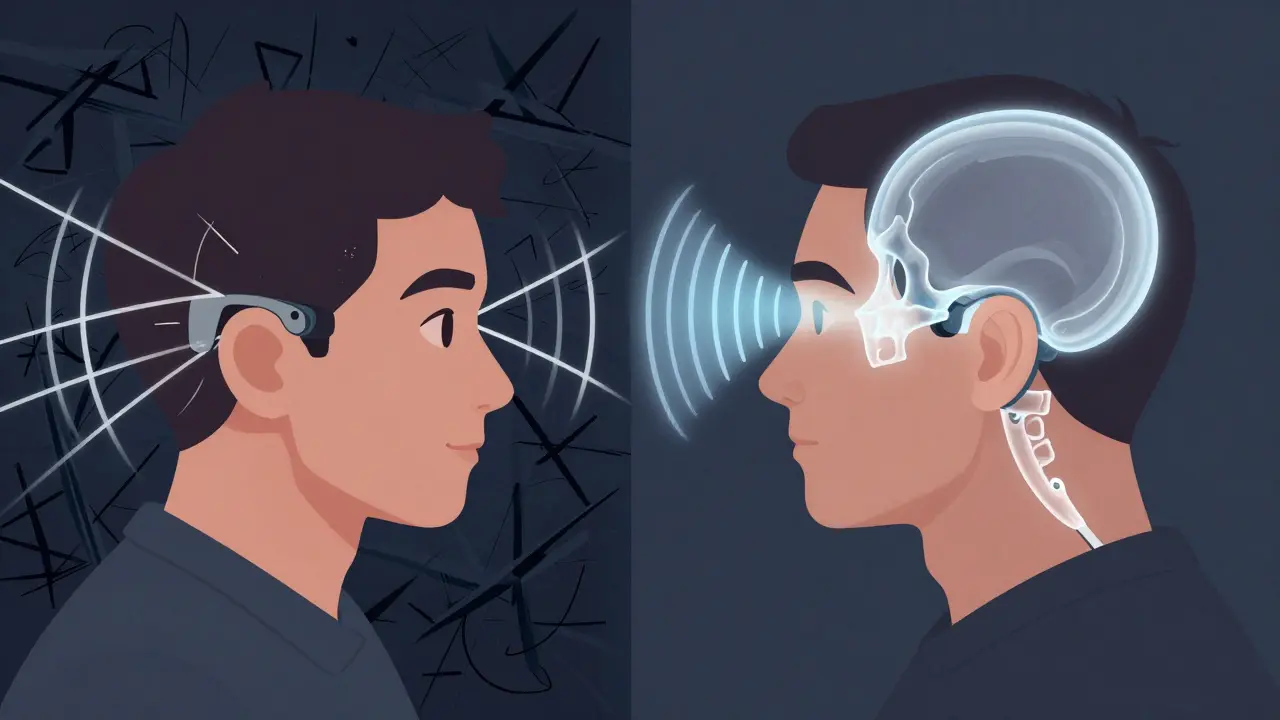
CROS (Contralateral Routing of Signals) hearing aids are the most common first step. They’re non-invasive. A tiny microphone on your deaf side picks up sound and sends it wirelessly-via Bluetooth or magnetic signals-to a hearing aid on your good ear. Think of it like a radio relay: your deaf ear becomes a listener, and your good ear becomes the speaker.
Modern CROS devices like the Phonak CROS Marvel, Oticon CROS Free, and Signia CROS Pure 312 are sleek, rechargeable, and even include tinnitus masking. They’re easy to put on, adjust, and remove. No cuts. No implants. No recovery time. You can try one for two weeks before buying. Most people adapt within days.
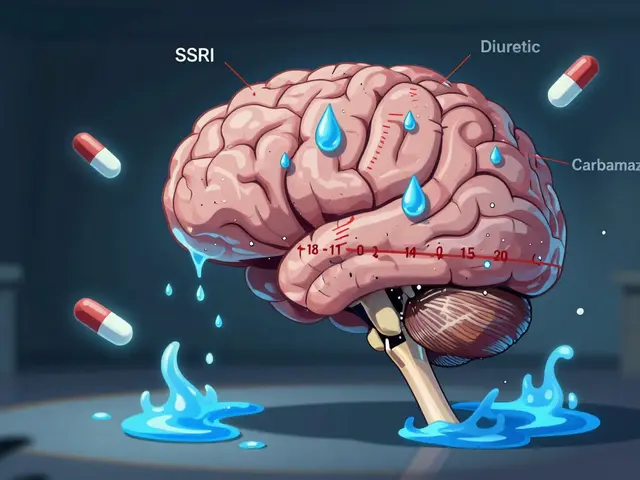
But here’s the catch: CROS doesn’t restore balance. It just moves sound. And in noisy places, it can make things worse. If someone talks to your deaf side while background noise is on your good side, the CROS system brings all that noise into your good ear too. Studies show users often report less speech understanding in restaurants or crowded offices than when they weren’t wearing anything at all. One Reddit user wrote: ‘I love not having surgery, but voices from my deaf side sound like they’re inside my head. And I’m changing batteries every two days.’
Another issue? Battery life. Most CROS devices use size 13 or 312 batteries that last only 2-3 days. That’s not a problem for some-but if you’re traveling, working long shifts, or hate fiddling with small batteries, it adds stress. And while CROS helps with awareness of sounds from the deaf side, it doesn’t help you locate where they come from. Your brain still hears everything as coming from your good ear.
Bone-Anchored Hearing Devices: Surgery, But Better Sound
Bone-anchored hearing systems (BAHS), like the Cochlear Baha 6 Max, Oticon Medical Ponto 5 SuperPower, and MED-EL Bonebridge, work differently. Instead of sending sound through air, they send vibrations directly through your skull bone to your inner ear. The sound bypasses your outer and middle ear entirely. This is called bone conduction.
There are two types: percutaneous and transcutaneous. Percutaneous systems, like the original Baha, have a small titanium implant screwed into your skull. After 3-6 months of healing, the sound processor clips onto a post sticking out of your skin. Transcutaneous systems, like the Ponto 5, use magnets to hold the processor against your scalp without a post. The MED-EL Bonebridge is fully implanted under the skin-no external post at all.
These devices don’t just move sound-they restore spatial hearing. Studies show BAHS reduces the head shadow effect by 8-10 dB, similar to CROS. But unlike CROS, they don’t amplify noise from the bad side. The sound travels straight through bone, so background noise on your good ear stays mostly untouched. In tests, BAHS users understood speech better than CROS users when noise was on their good side.
Users often describe the sound as ‘more natural.’ One user on HearingTracker said: ‘The surgery healed well, but I get skin irritation twice a month. Still, the sound quality is worth it.’
Cost, Surgery, and Long-Term Trade-Offs
CROS systems cost between $2,500 and $4,000. BAHS systems cost $4,000 to $8,000 for the device alone-plus $3,000 to $7,000 for surgery. Insurance often covers BAHS if you meet criteria, but CROS is rarely covered unless you have other hearing loss.
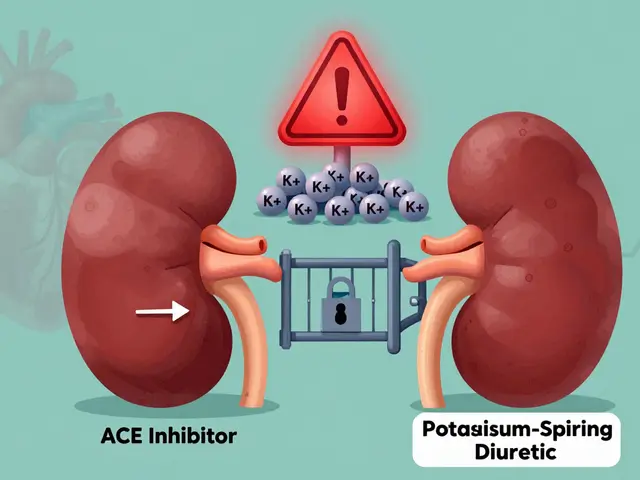
Surgery isn’t minor. It requires a CT scan, a 45-minute procedure under local or general anesthesia, and 3-6 months of healing before the processor is even turned on. Complications happen. About 15-63% of percutaneous users develop skin reactions around the implant-redness, swelling, or infection. Some need antibiotic creams or even revision surgery. Transcutaneous systems reduce this risk, but they’re less powerful and may not work well if you have thick scalp tissue.
Long-term, BAHS users stick with it. In one study, 93% of BAHS users came back for follow-ups. Only 46% of CROS users did. Why? Because CROS often disappoints. People expect it to fix everything. It doesn’t. It’s a band-aid. BAHS, while more invasive, delivers real, measurable improvement in hearing quality.
Who Gets What?
Not everyone is a candidate for both. CROS only works if your good ear has normal hearing (pure-tone average of 25 dB HL or better). If your good ear also has mild hearing loss, CROS won’t help-it might even make things worse. BAHS can work even if your good ear has mild-to-moderate hearing loss (up to 45-55 dB HL), because it delivers sound directly to the inner ear.
Age matters too. Most users are between 45 and 64. But younger people with SSD from trauma or illness are increasingly seeking solutions. If you’re active-running, swimming, working in construction-BAHS is more stable. CROS devices can fall out during exercise. BAHS stays put.
Occupation plays a role. People in loud jobs-firefighters, musicians, factory workers-are more likely to choose BAHS because they need reliability. Office workers who mostly talk face-to-face might do fine with CROS.
The Future: Cochlear Implants and AI
There’s a new player: cochlear implants (CIs) for SSD. Until recently, CIs were only for people with hearing loss in both ears. But new research, including the 2015 CINGLE trial, showed CI users had far better sound localization than those with CROS or BAHS. In 2024, the FDA expanded CI approval for SSD.
Now, experts recommend a step-by-step approach: Try CROS first for at least 4 weeks. If you’re still struggling-especially in noise or with spatial awareness-move to BAHS. If you’re still not satisfied after 6 months, consider a cochlear implant. The latest BAHS models, like Cochlear’s Baha 7 Smart, now use AI to reduce wind noise and enhance speech. CROS systems are getting smarter too, with better noise filters and Bluetooth streaming to phones.
What Should You Do?
Don’t accept SSD as permanent silence. There are options. But choosing the right one isn’t about what’s newer or pricier-it’s about your life.
If you:
- Want to avoid surgery
- Have normal hearing in your good ear
- Work in quiet environments
- Don’t mind changing batteries often
Then CROS is a good starting point.
If you:
- Have mild hearing loss in your good ear
- Need reliable sound in noisy places
- Exercise, swim, or work in loud environments
- Want long-term stability and better sound quality
Then BAHS is worth the surgery.
And if you’ve tried both and still feel like you’re missing out on conversations, ask about cochlear implants. The technology has changed. What was once a last resort is now a first option for many.
There’s no one-size-fits-all. But there is a right choice-for you. Talk to an audiologist who specializes in SSD. Get tested. Try devices. Don’t settle for silence when sound is within reach.
Can CROS hearing aids restore normal hearing in one ear?
No. CROS systems don’t restore hearing in the deaf ear. They route sound from the deaf side to the good ear. Your brain still receives all sound through one ear, so true binaural hearing-like natural sound localization and noise filtering-isn’t possible. CROS helps you hear sounds from your deaf side, but it doesn’t fix how your brain processes them.
Is bone-anchored hearing surgery risky?
Like any surgery, there are risks. The most common is skin irritation around the implant (15-63% of users). Infection, delayed healing, or implant loosening can happen. But serious complications are rare. Most patients heal well, especially with transcutaneous systems like Oticon’s Ponto 5 or MED-EL’s Bonebridge, which avoid skin penetration. The procedure is outpatient, takes less than an hour, and most people return to normal activities within a week.
How long do CROS and bone-anchored devices last?
CROS hearing aids typically last 4-6 years before needing replacement, depending on usage and battery wear. Bone-anchored sound processors last 5-7 years. The titanium implant (in percutaneous systems) is designed to last a lifetime. If your processor fails, you can usually just swap it out without another surgery. Transcutaneous systems like Bonebridge have internal components that also last decades.
Can children use CROS or bone-anchored hearing devices?
Yes. Children as young as 5 can use bone-anchored systems with softbands before they’re old enough for surgery. CROS devices are also used in kids with SSD, especially if they’re not candidates for surgery. Early intervention helps with speech development and school performance. Many schools now support hearing devices as part of educational accommodations.
Does insurance cover CROS or bone-anchored hearing devices?
It depends. Most private insurance plans cover bone-anchored systems if you meet medical criteria-like normal hearing in the good ear and documented speech understanding issues. CROS systems are rarely covered because they’re considered ‘non-medical’ by some insurers. Medicare typically doesn’t cover hearing aids. Medicaid coverage varies by state. Always check with your provider and ask for a pre-authorization letter.
Can I use CROS and BAHS together?
No. Both devices are designed to work as standalone solutions. Using them together would cause feedback, interference, and confusion for your brain. The goal is to pick one system that best matches your needs. If one doesn’t work, you can switch to the other-many people start with CROS and upgrade to BAHS later.
Why do some people say CROS makes noise worse?
CROS picks up all sound from the deaf side-including background noise-and sends it to your good ear. If the noise is louder than the speech you’re trying to hear, your brain gets flooded. Studies show CROS users often perform worse than unaided in noisy environments where the noise is on the deaf side. It’s not broken-it’s just not designed for complex listening situations. BAHS avoids this because it doesn’t amplify noise from the bad side.
What’s the success rate for bone-anchored hearing devices?
Success rates are high. Around 90% of users report improved speech understanding in noise and better sound localization after 6 months. Satisfaction rates are above 85% in long-term studies. The biggest factor in success is proper patient selection-making sure you have the right type of hearing loss and realistic expectations. Choosing a specialist with experience in SSD is key.




I tried a CROS system for three months and honestly? It felt like my brain was stuck in a tin can. Sounds from my left side came out of my right ear like they were inside my head. I stopped using it after my kid started screaming from behind me and I had no idea where it was coming from. Still better than nothing, I guess.
SSD isn’t just about hearing-it’s about feeling included. I used to avoid parties, dinners, even family gatherings because I’d miss half the jokes. Got the Baha 6 Max last year. Surgery was a breeze, the healing took longer than I expected, but now? I hear my wife whispering from the left side while she’s making coffee. That’s not a device-that’s a lifeline.
Everyone’s acting like BAHS is magic. Let’s be real-15-63% infection rates? That’s not a ‘risk,’ that’s a warranty claim waiting to happen. And you’re telling me people are okay with a metal post sticking out of their skull? Meanwhile, CROS users are just being told to ‘adapt.’ No wonder 54% quit. The real problem? Audiologists push the expensive stuff because they get kickbacks. Don’t believe the hype.
For anyone considering BAHS: find a center that specializes in SSD, not just general audiology. My first audiologist didn’t even mention transcutaneous options. I ended up with a Ponto 5 SuperPower and zero skin issues after 18 months. Also-don’t rush the trial period. Give CROS at least 6 weeks. Some people need time for their brain to rewire.
Oh sweetie, you’re still using CROS? Honey, you’re not ‘adapting,’ you’re just tolerating a glorified Bluetooth speaker taped to your head. If you’re in your 40s and still changing batteries every two days, you’re doing it wrong. Go get the implant. Your brain will thank you. And no, your insurance shouldn’t make you beg for it-this isn’t a luxury, it’s a necessity.
My dad had a BAHS after acoustic neuroma surgery. He’s 72. Wears it every day. Doesn’t complain. He says he finally hears his grandkids laughing from the other room. That’s the whole point, isn’t it? Not the tech. Not the cost. Just being there.
Interesting how the article glosses over the fact that most CROS users are middle-aged professionals who can afford to try things. What about the gig workers, the single moms, the people without insurance? The system is rigged. BAHS is the gold standard, but only if you’ve got the privilege to access it. The real tragedy isn’t the deafness-it’s the healthcare inequality.
Let me tell you about the day I realized BAHS changed my life. I was at the farmers market-rainy, crowded, music blaring from a speaker on my left. Someone asked me if I wanted the organic kale. I turned, heard them clearly, and said yes. No squinting. No leaning. No guessing. That’s not a hearing aid. That’s a portal back to the world. CROS is like listening to a podcast through a pillow. BAHS? It’s like someone finally turned the volume on reality.
Wow. So CROS is a band-aid, BAHS is surgery with side effects, and cochlear implants are the ‘new hotness.’ What’s next? A neural lace? I get it-you want to fix everything. But maybe the real solution is just… learning to lip-read and using subtitles everywhere. Or better yet-stop treating deafness like a glitch to be coded out. Sometimes silence is just… peace.
My cousin tried CROS after a car accident. She hated it. Got the Bonebridge. Now she swims, hikes, even does yoga without worrying about her device falling off. The only thing she misses? The sound of her own footsteps on gravel. Weird, right? Turns out, your brain notices the little things. But she’d take that trade any day.
Y’all in the West act like this is some new miracle. In Nigeria, we’ve been using bone conduction for generations-traditional healers with metal rods on the skull. You pay $8K for tech that’s basically a glorified tribal tool? And you call it innovation? 🤦♀️