 30
Dec,2025
30
Dec,2025
Hyponatremia Risk Assessment Tool
Medication Risk Assessment
Based on the latest medical guidelines, this tool estimates your risk of severe hyponatremia (sodium below 120 mmol/L) from prescribed medications.
Low sodium isn’t just a lab number. When it drops too fast because of a medication, your brain starts to panic. Confusion. Headaches. Seizures. In some cases, death. This isn’t rare. It’s happening in hospitals, nursing homes, and even in people taking pills at home because their doctor never warned them.
What Exactly Is Severe Hyponatremia?
Sodium is the salt in your blood that keeps your cells balanced. Normal levels are between 135 and 145 mmol/L. When it falls below 135, you have hyponatremia. Below 120? That’s severe. At this point, water floods into your brain cells. They swell. And that’s when things go wrong fast.
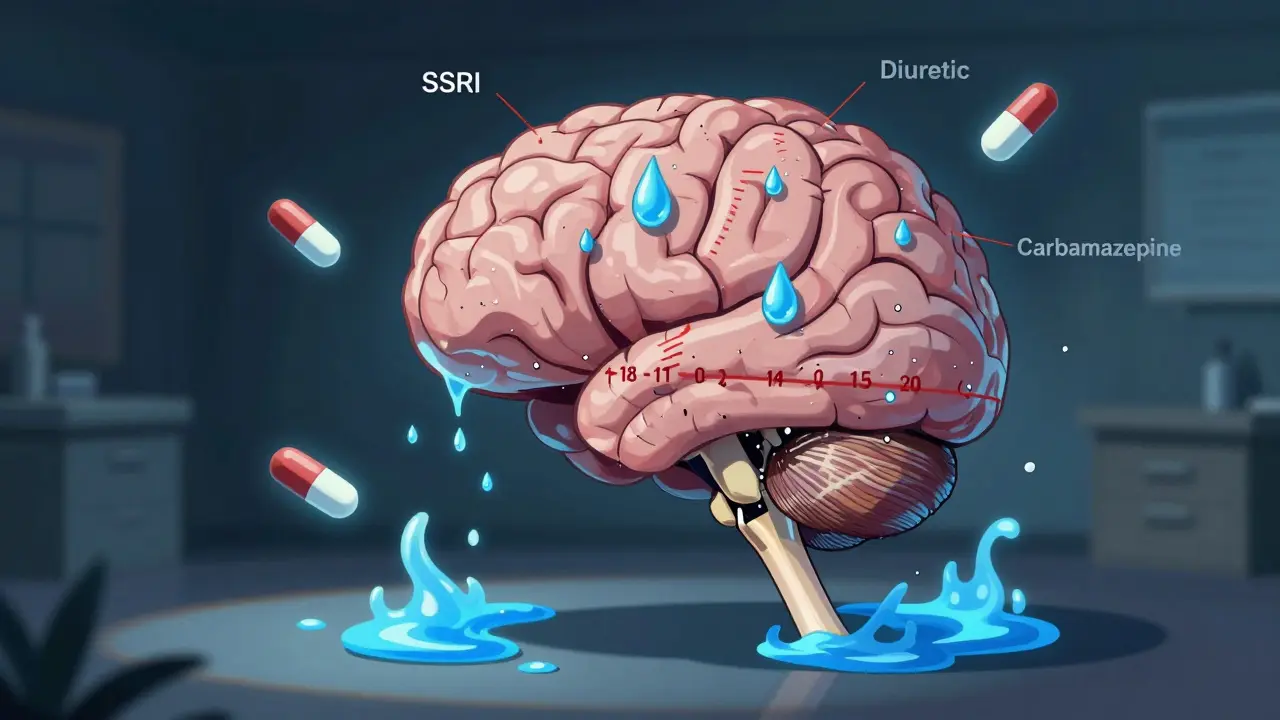
Medications cause about 1 in 5 cases of severe hyponatremia in hospitals. The most common culprits? Diuretics (water pills), SSRIs like sertraline and citalopram, and antiseizure drugs like carbamazepine. Even common painkillers like ibuprofen can trigger it in vulnerable people. It doesn’t take months. Often, sodium starts dropping within days of starting the drug - sometimes as early as day 3.
How Do You Know It’s Happening?
The symptoms are easy to miss. They look like the flu. Or stress. Or aging.
- Confusion - not just being forgetful, but not knowing where you are or who people are
- Nausea and vomiting - often the first sign, but dismissed as a side effect
- Headaches - persistent, unlike typical tension headaches
- Muscle weakness or cramps
- Seizures - especially in people with sodium below 115 mmol/L
- Coma - if untreated, this is the final stage
A 72-year-old woman in Melbourne started sertraline for depression. By day 9, she was confused, stumbling, and vomiting. Her GP said it was ‘just adjusting to the medication.’ Two days later, she had a grand mal seizure. Her sodium was 118. She spent five days in ICU. Her doctor never checked her sodium after prescribing it.
This isn’t an outlier. On patient forums, 68% of people with medication-induced hyponatremia say their symptoms were ignored at first. Nurses on Reddit report cases where confusion was labeled as ‘early dementia.’ Vomiting? ‘Gastro bug.’ Headache? ‘Stress.’ By the time someone connects the dots, it’s often too late.
Why Do Some Drugs Cause This?
It’s mostly about SIADH - Syndrome of Inappropriate Antidiuretic Hormone. Normally, your body releases ADH to hold water when you’re dehydrated. But certain drugs trick your brain into making too much ADH, even when you’re not dehydrated. That means your kidneys keep absorbing water, diluting your sodium.
SSRIs are the biggest offenders. They interfere with how serotonin affects ADH release. Carbamazepine does the same. Diuretics like hydrochlorothiazide flush out sodium, but also make you drink more water - a dangerous combo. Even MDMA (ecstasy) can cause this - and it’s not just a party drug. People taking it for chronic pain or anxiety are at risk too.
Some drugs are far more dangerous than others. Carbamazepine has a relative risk of 5.3 compared to non-users. That means you’re over five times more likely to get severe hyponatremia on it than someone not taking it.

Who’s Most at Risk?
This isn’t random. Certain people are sitting ducks.
- People over 65 - 61% of severe cases
- Women - 57% of cases, possibly due to body composition and hormone differences
- People on multiple medications - especially diuretics + SSRIs
- Those with kidney, heart, or liver disease
- People who drink a lot of water - especially if they’re on a drug that makes them retain it
One study found that people over 65 are 2.7 times more likely to develop hyponatremia from medications than younger adults. And it’s not just about age - it’s about how little monitoring happens. Only 63% of doctors follow the FDA’s own guidelines to check sodium within 30 days of starting high-risk drugs.
What Happens If It’s Not Treated?
Severe hyponatremia kills. If sodium stays below 115 mmol/L for more than 48 hours without correction, the mortality rate hits 37%. Even if you survive, you might not recover fully.
One major risk is osmotic demyelination syndrome. That’s when sodium is corrected too fast. Your brain cells, swollen from too much water, get damaged when the water suddenly leaves. This can cause locked-in syndrome - you’re awake, but can’t move or speak. It happens in about 9% of cases where correction is rushed.
Doctors now know: slow and steady wins the race. Correct sodium by no more than 6-8 mmol/L in the first 24 hours. Too fast? Brain damage. Too slow? Seizures and coma. It’s a tightrope walk - and it requires hospital care.
How Is It Diagnosed and Treated?
If you’re on a high-risk drug and feel off, get a blood test. That’s it. No MRI. No CT scan. Just a simple sodium level.
Once confirmed, treatment depends on how fast the drop happened and how low the sodium is.
- For mild cases (130-134 mmol/L): stop the drug, limit fluids, monitor
- For moderate cases (120-129 mmol/L): IV fluids with careful sodium adjustment
- For severe cases (below 120 mmol/L): hospitalization, IV hypertonic saline, close monitoring
New drugs like tolvaptan (Samsca) are now approved for medication-induced cases. It blocks ADH, helping your body get rid of excess water without losing sodium. In trials, it corrected sodium 34% faster than standard care.
But the real win? Prevention.

How to Prevent It
You can’t always avoid the medication. But you can avoid the disaster.
- Ask your doctor: ‘Is this drug linked to low sodium?’ before you start it
- Request a sodium blood test 7-10 days after starting high-risk drugs - especially if you’re over 65
- Don’t drink excessive water. No more than 1.5-2 liters a day unless told otherwise
- Know the symptoms. If you feel confused, nauseous, or have a headache after starting a new pill, don’t wait. Get tested
- Ask your pharmacist. They see drug interactions every day. One patient’s pharmacist caught an SSRI + diuretic combo before the script was filled. Her sister had seizures from the same mix.
Doctors need to do better. A 2023 study found it takes an average of 3.2 cases before a clinician starts recognizing the pattern. That’s three people nearly dying before someone learns.
What’s Changing in 2025?
Things are slowly improving. In March 2024, the European Medicines Agency required pharmacists to give sodium monitoring advice when dispensing high-risk drugs. The FDA now mandates stronger warnings on 27 medications.
But real progress is coming from tech. Mayo Clinic is testing an AI tool that scans electronic health records and predicts hyponatremia risk 72 hours before symptoms show. It’s 87% accurate. Imagine if your doctor got an alert: ‘Patient on sertraline - sodium likely to drop below 125 in 48 hours.’ That’s not sci-fi. It’s happening now.
Still, the biggest barrier isn’t technology. It’s awareness. Patients aren’t warned. Doctors don’t test. And the system keeps moving.
What You Can Do Right Now
If you’re taking any of these drugs:
- SSRIs (sertraline, fluoxetine, citalopram, escitalopram)
- Diuretics (hydrochlorothiazide, furosemide)
- Antiseizure meds (carbamazepine, oxcarbazepine)
- NSAIDs (ibuprofen, naproxen - especially long-term)
- MAOIs or MDMA
Ask for a sodium blood test. Don’t wait for symptoms. Don’t assume it’s ‘normal.’ If your doctor says no, ask why. If they still refuse, go to a pharmacist or urgent care. Get it done.
And if you’ve already had confusion or a seizure on a new medication - tell every doctor you see. Write it down. Make it part of your medical history. Because this isn’t a one-time event. It can happen again.
Low sodium doesn’t announce itself with a siren. It whispers. And if you’re not listening, it screams.
Can antidepressants cause low sodium?
Yes. SSRIs like sertraline, citalopram, and fluoxetine are among the most common causes of medication-induced hyponatremia. About 22% of all drug-related cases are tied to these antidepressants. The risk is highest in the first 2-4 weeks after starting the drug. Symptoms like nausea, confusion, or headaches shouldn’t be brushed off as ‘side effects.’ Get a blood test if you’re on one of these and feel off.
How long does it take for hyponatremia to develop from medications?
It can happen as quickly as 3-7 days after starting a high-risk drug. Most cases occur within the first 30 days. A 2023 study found 73% of severe cases developed within that window. That’s why guidelines now recommend checking sodium levels within 7-10 days of starting drugs like SSRIs or diuretics - especially in people over 65.
Is hyponatremia from drugs reversible?
Yes - if caught early. When treated within 24 hours, recovery rates are 92%. But if treatment is delayed beyond 48 hours, the chance of full recovery drops to 67%. Some people recover completely after stopping the drug and correcting sodium slowly. Others suffer permanent brain damage, especially if sodium was corrected too quickly or if seizures occurred. Timing and careful correction make all the difference.
Can I check my sodium at home?
No. Sodium levels can only be measured through a blood test. There are no reliable home devices or finger-prick tests for sodium. If you suspect low sodium, go to a clinic, pharmacy, or urgent care for a simple blood draw. It takes minutes and costs less than $50 in most places. Don’t wait for symptoms to get worse.
What should I do if I have a seizure from low sodium?
Call emergency services immediately. Do not try to treat it yourself. Seizures from hyponatremia mean your sodium is dangerously low - likely below 115 mmol/L. This is a medical emergency. You need IV fluids and careful correction in a hospital. Even if the seizure stops, you still need urgent care. Delaying treatment increases the risk of permanent brain damage or death.
Are older adults more at risk?
Yes. People over 65 make up 61% of severe medication-induced hyponatremia cases. Their kidneys don’t handle water balance as well, they’re more likely to be on multiple medications, and they often drink more water thinking it’s healthy. The risk is 2.7 times higher than in younger adults. Any older person starting a new medication - especially an SSRI or diuretic - should get a sodium test within 10 days.





OMG I knew a lady who went from ‘just tired’ to ICU in 4 days after starting sertraline. Her doctor said ‘it’s just anxiety’ 🤦♀️ Why do they treat older women like they’re just being dramatic? I’m telling everyone I know to ask for a sodium test before taking any new pill. This isn’t hype - it’s survival.
So let me get this straight - we’ve got a system that can predict stock market crashes in real time but can’t alert a doctor that their 70-year-old patient’s brain is slowly drowning in water because of a depression pill? 🤔 The real tragedy isn’t the hyponatremia. It’s that we’ve normalized medical negligence as ‘standard practice.’
Big Pharma knows. They just don’t care. 💊☠️ SSRIs are basically water retention bombs with a smiley face. And don’t even get me started on how they push these on grandmas like they’re vitamins. #WakeUpSheeple
This is why western medicine is broken you people think a blood test solves everything but in Nigeria we know your body speaks if you listen stop overmedicalizing everything
Okay so I’m 68 and on hydrochlorothiazide and sertraline and I’ve had headaches for 3 weeks and my husband says ‘you’re just stressed’ but I’ve been googling and I think I’m dying?? Can someone tell me if I’m being paranoid or if I should go to the ER right now?? I’m terrified and no one listens and I just want to live please help
Y’all need to stop treating doctors like gods. I had my sodium checked after 5 days on citalopram - it was 129. My doc said ‘eh, it’s fine.’ I walked out, went to urgent care, and they admitted me. That’s the difference between ‘maybe I’m fine’ and ‘I’m not dying on your watch.’
It’s not just about the drugs. It’s about how we treat elderly patients like invisible objects. If a 25-year-old had these symptoms, they’d get scanned, tested, and treated immediately. But a 72-year-old woman? ‘Oh, that’s just aging.’ That’s not medicine. That’s ageism with a stethoscope.
Hey everyone - I’m a nurse in Mumbai and I’ve seen this over and over. One woman came in after 3 days on fluoxetine - confused, vomiting, couldn’t stand. Sodium was 114. We started IV saline immediately. She woke up 2 days later crying because she remembered her granddaughter’s birthday. But here’s the thing - she didn’t know she was in danger. No one told her. So if you’re on any of these meds - especially if you’re over 60 - don’t wait for a seizure. Get tested. Just one blood draw. It’s cheaper than your morning coffee. And it could save your mind. Please. I beg you. Don’t be like the 68% who got ignored. Be the 32% who asked. Your brain will thank you.
Man… I’ve been on carbamazepine for seizures for 12 years. Never knew this was a thing. My doc never mentioned sodium. I’ve had headaches for years and thought it was just stress. Guess I’m getting tested next week. Thanks for the wake-up call. 🙏
While the clinical observations presented are indeed compelling, one must consider the broader epidemiological context. The prevalence of medication-induced hyponatremia remains statistically low relative to the total population exposed to these agents. To suggest systemic negligence without acknowledging the complexity of polypharmacy and comorbidities risks fueling unwarranted public alarmism. Evidence-based guidelines exist - adherence, not suspicion, is the corrective mechanism.
My mom had a seizure on sertraline. They told her it was ‘just a phase.’ She spent 11 days in the hospital. Now she’s fine - but she can’t remember my wedding. I’m not mad at the doctor. I’m mad that no one warned us. This post? It’s the reason I’m telling every single person I know to get tested. Don’t wait for the scream. Listen for the whisper.
Test your sodium 7-10 days after starting SSRIs or diuretics. That’s it. No drama. No panic. Just a simple blood test. If your doc says no, get a second opinion. Your brain is worth it.