 29
Dec,2025
29
Dec,2025
If you’re paying hundreds of dollars a month for a prescription, you’re not alone. Many people with chronic conditions - like asthma, diabetes, or rheumatoid arthritis - face sticker shock at the pharmacy counter, even with insurance. That’s where prescription assistance programs come in. These are direct help programs run by drug manufacturers themselves, not government agencies or nonprofits. They’re designed to lower your out-of-pocket costs for brand-name medications, especially when generics aren’t an option.
Two Types of Help: Copay Cards and Free Medications
There are two main kinds of manufacturer assistance programs. One is for people with insurance. The other is for those without it.Copay assistance programs are the most common. These come as cards or coupons you show at the pharmacy. The drug company pays part (or all) of your copay. For example, if your copay is $150 for a specialty asthma inhaler, the card might cover $140, leaving you to pay just $10. These are often available for expensive brand-name drugs - especially specialty medications used for conditions like multiple sclerosis, cancer, or rare autoimmune diseases. About 85% of specialty drugs now offer some kind of copay card, according to PhRMA’s 2023 report.
But these cards have limits. Around 45% cap the total help you can get in a year - anywhere from $1,000 to $25,000. Some limit you to $200 per month. And not all insurance plans let you use them. Many insurers now use “copay accumulator” programs, which means the manufacturer’s payment doesn’t count toward your deductible or out-of-pocket maximum. That can leave you stuck in the coverage gap longer.
The second type is Patient Assistance Programs (PAPs). These are for people who don’t have insurance, or who have insurance but still can’t afford their meds. PAPs often give you the medication for free or at a very low cost. To qualify, you usually need to prove your income is below 200-400% of the Federal Poverty Level. For a family of four in 2023, that meant earning less than $60,000 a year. Programs like Teva’s Cares or Pfizer’s Patient Assistance Program have helped millions get life-saving drugs they otherwise couldn’t afford.
Who Can’t Use These Programs?
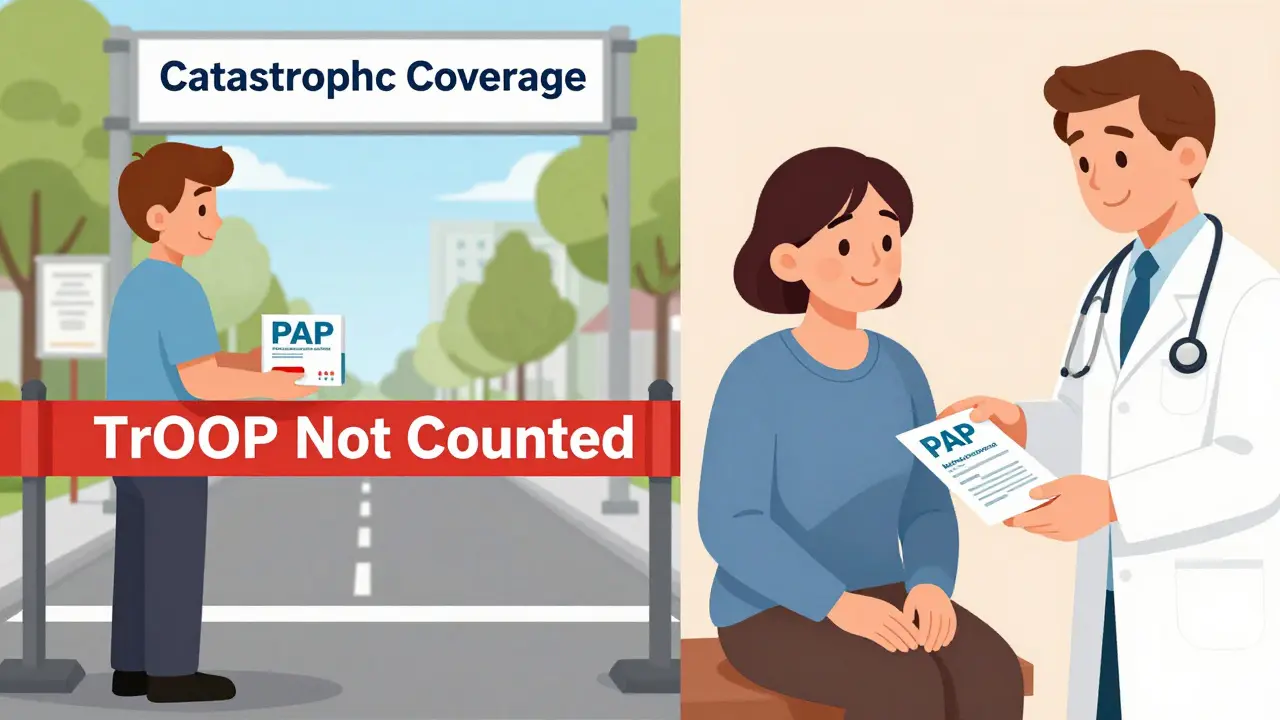
Here’s the catch: not everyone qualifies. If you’re on Medicaid or Medicare, many PAPs won’t help you at all. That’s because federal rules say PAP assistance can’t count toward your Medicare Part D “true out-of-pocket” costs (TrOOP). That means even if you get free drugs through a PAP, you’re still stuck in the Medicare coverage gap longer. You won’t reach catastrophic coverage any faster.And in 78% of state Medicaid programs, using manufacturer copay cards is outright banned. Why? Because states worry these programs push patients toward more expensive brand-name drugs instead of cheaper generics - driving up overall healthcare spending. In fact, a 2022 study in JAMA Internal Medicine estimated copay assistance added $1.4 billion to total drug spending each year by discouraging generic use.
Even if you’re eligible, applying can be a hassle. The average PAP application takes 45 to 60 minutes. You need tax returns, pay stubs, doctor’s notes, and proof of residency. Some programs require reapplying every year. A 2022 survey by the Patient Advocate Foundation found only 37% of eligible patients even knew these programs existed.
How to Find and Use These Programs
The easiest way to start is with the Medicine Assistance Tool (MAT), run by PhRMA. It’s free, confidential, and lets you search over 900 assistance programs by drug name, condition, or income level. Just enter your medication and zip code - it will show you which manufacturers offer help, what the income limits are, and how to apply.For copay cards: Once you find a program, download the card or get a code. Bring it to the pharmacy when you fill your prescription. The pharmacist will process it like a coupon. No paperwork needed at your end.
For PAPs: You’ll need to fill out a form - usually online or by mail. You’ll need:
- Proof of income (last two pay stubs or tax return)
- Proof of U.S. residency
- Prescription from your doctor
- Doctor’s signature on the application
Some programs mail you the medication directly. Others give you a card to use at the pharmacy. If approved, you might pay as little as $15 per prescription - like with Dulera for asthma, where the maximum savings is $90 per fill.
The Bigger Picture: Are These Programs Helping or Hurting?
Supporters say these programs save lives. PhRMA reports that in 2022, drug companies gave $24.5 billion in assistance to 12.7 million people. Dr. Jane Smith from the Brookings Institution says without copay cards, 2.3 million more Americans would skip doses or stop taking their meds entirely.But critics point out these programs don’t fix the real problem: drug prices. They’re a Band-Aid on a broken system. Manufacturers set high list prices, then offer discounts to make it look like they’re helping. Meanwhile, insurers and pharmacy benefit managers (PBMs) often get the rest of the rebate - not the patient.
And the system is getting more complicated. Twenty-two states have passed laws to regulate or restrict copay assistance. California now requires drugmakers to publicly report how much they spend on these programs. The federal government is also looking at new rules to increase transparency.
Some experts worry these programs reinforce inequality. If you have private insurance, you might get $100 off your drug. If you’re on Medicaid or uninsured, you might get nothing. And if you’re on Medicare, you might get free drugs - but it won’t help you get out of the coverage gap.
What’s Next for Prescription Assistance?
The market for these programs is growing fast. Analysts at Evaluate Pharma predict drug manufacturers will spend $38.2 billion on patient assistance by 2027. That’s up from $24.5 billion in 2022. More programs are being added, and digital tools are making them easier to use. MAT now connects directly with pharmacy systems so discounts are applied automatically.But without real price controls, these programs will keep being a stopgap. They’re essential right now - especially for people who can’t afford their meds. But they’re not a long-term solution. The hope is that as more states and the federal government step in with price transparency laws and caps on out-of-pocket costs, these programs will become less necessary.
For now, if you’re struggling to pay for your prescription, don’t assume you’re out of options. Check MAT. Talk to your pharmacist. Ask your doctor’s office - they often have patient coordinators who help with applications. Even if you think you don’t qualify, it’s worth applying. Many people get approved who never thought they would.
Frequently Asked Questions
Do I qualify for a patient assistance program if I have Medicare?
It depends. Most manufacturer PAPs do not help people with Medicare or Medicaid. This is because federal rules say the assistance can’t count toward your Medicare Part D out-of-pocket costs. However, a few programs have exceptions for low-income Medicare beneficiaries. Always check the specific program’s rules - some may still help if you meet very low income thresholds.
Can I use a copay card with my insurance?
Maybe. Many insurers now use “copay accumulator” programs, which means the manufacturer’s payment doesn’t count toward your deductible or out-of-pocket maximum. This can leave you paying more over time. Always ask your insurance company if they allow copay assistance to count toward your limits. If they don’t, you might still save money on each prescription - but it won’t help you reach catastrophic coverage faster.
Are manufacturer assistance programs only for brand-name drugs?
Yes. Copay cards and PAPs are almost always for brand-name medications. Generic drugs are already low-cost, so manufacturers don’t offer assistance for them. These programs are designed to help with expensive specialty drugs where there’s no generic alternative - like biologics for rheumatoid arthritis or cancer treatments.
How long does it take to get approved for a PAP?
Approval can take anywhere from a few days to six weeks, depending on the program and how quickly you submit all required documents. Some programs offer expedited review for life-threatening conditions. Always follow up if you haven’t heard back after two weeks. Your doctor’s office may be able to help speed up the process.
Is the Medicine Assistance Tool (MAT) really free and confidential?
Yes. MAT is run by PhRMA and is completely free to use. You don’t need to create an account or give personal information unless you decide to apply for a program. Your search history and data are not shared with drug companies or insurers. It’s designed to be a private, secure way to find help.
Can I use more than one assistance program at the same time?
Generally, no. Most programs require you to choose one source of assistance per medication. You can’t stack manufacturer copay cards or combine a PAP with a nonprofit grant for the same drug. But you can use different programs for different medications. For example, one PAP for your diabetes drug and a copay card for your blood pressure medication.
What if I don’t have a doctor or insurance?
You still might qualify. Some PAPs allow you to use a letter from a clinic or community health center instead of a private doctor’s note. If you don’t have insurance, you may still be eligible for a PAP as long as you meet income requirements. Contact the program directly - they often have case managers who can help you navigate the process.
Next Steps
If you’re paying too much for prescriptions, start here:
- Go to medicinesassistancetool.org and search for your medication.
- Check if you qualify for a copay card or PAP.
- Print or save the application and bring it to your doctor.
- Ask your pharmacist if they’ve helped other patients with the same drug.
- If you’re denied, call the program’s helpline - sometimes decisions are overturned with a quick call.
Don’t give up. These programs work - but only if you ask. Millions of people use them every year. You’re not the first, and you won’t be the last. The system is flawed, but help is out there if you know where to look.





I literally cried when I found out my insulin copay card covered $120 of my $140 monthly bill. I’ve been skipping doses to make it last, and then I almost died in the ER last year. This isn’t charity-it’s survival. If you’re reading this and you’re scared to apply? Do it. The paperwork sucks, but so does dying. I got approved in 11 days. You’re not a burden. You’re a human being trying to live.
just found out my insurer blocks copay cards... so even though i get $150 off my biologic, it dont count toward my deducible. so i’m still paying full price until i hit $8k. feels like they’re playing a rigged game. thanks for the heads up on MAT though. gonna check it out now.
ughhh why is this so complicated?! 😭 I just want my meds without crying over my bank app. Why do I have to be a detective just to stay alive?! 🤯 #PharmaIsTheVillain
Oh wow, so drug companies give $24 billion in 'help'... but only after they jack up the list price to $800 a pill? Brilliant business model. You get a $100 coupon? Congrats. You just paid $700 extra so they could give you back $100. And now they're lobbying to ban Medicaid from using those same cards? Classic. They don't care if you live-they care if you're profitable.
From a PBM analyst perspective: these programs are a necessary evil. They reduce non-adherence, which lowers long-term ER costs. But the structural inefficiencies-copay accumulators, Medicaid bans, Medicare TrOOP loopholes-are systemic failures. The real win would be integrating these programs into a unified, automated eligibility engine. MAT is a good start, but we need interoperability with EHRs and pharmacy networks. We’re talking about saving lives, not just optimizing coupons.
People who can't afford meds should just get a job. If you're on Medicaid, you're already getting help. Stop being lazy and stop blaming pharma. I work two jobs and I pay full price. You can too.
Just wanted to say-this post saved me. I’ve been on Dulera for 3 years and thought I was stuck paying $110 a month. Found the PAP through MAT, applied with my clinic’s help, and now I pay $15. My lungs feel like they’re breathing again. Don’t give up. Talk to your pharmacist. They’ve seen it all. And yes, your doctor’s office probably has someone who does this all day. Just ask.
It’s fascinating how this entire system functions as a performative altruism façade. Drug manufacturers, in their infinite wisdom, have engineered a compliance theater where they appear benevolent while maintaining monopolistic pricing structures. The fact that patients are expected to navigate bureaucratic labyrinths to receive what should be a basic human right is not just inefficient-it’s ethically indefensible. One wonders if the boardrooms even acknowledge that these are people, not line items.
Who even needs these programs? If you can't afford your meds, maybe you shouldn't be on them. I work 60 hours a week and I pay full price. If you're on Medicare, you're already getting taxpayer money. Stop sucking the system dry. This is why America's healthcare is broken-because everyone wants a handout.
As a Canadian who has lived under universal coverage for over two decades, I must say this is both heartbreaking and bewildering. That people in a nation with such vast resources must navigate such labyrinthine systems just to breathe, to walk, to live... it is a profound moral failure. I do not say this to judge, but to bear witness. May your courage in seeking help be met with more compassion than bureaucracy. From Toronto, with deep solidarity.
THEY’RE JUST GIVING AWAY DRUGS?!?!?!?!!?!!? This is why we’re BROKE!!! Who’s paying for this?! TAXPAYER MONEY?!?!!?!!? I work at a factory and I pay full price!! I don’t get free stuff!! This is SOCIALISM!! 🚨🚨🚨 #AMERICAFIRST #NOFREESTUFF