 6
Jan,2026
6
Jan,2026
When your medicine costs too much, you skip doses - and it’s more common than you think
Imagine you’re told to take a pill every day to keep your blood pressure under control. But when you go to pick it up, the copay is $75. You’ve already paid rent, bought groceries, and fixed your car. So you skip a few days. Then a week. Then you stop filling the prescription altogether. This isn’t rare. It’s happening to millions of people in the U.S. every year.
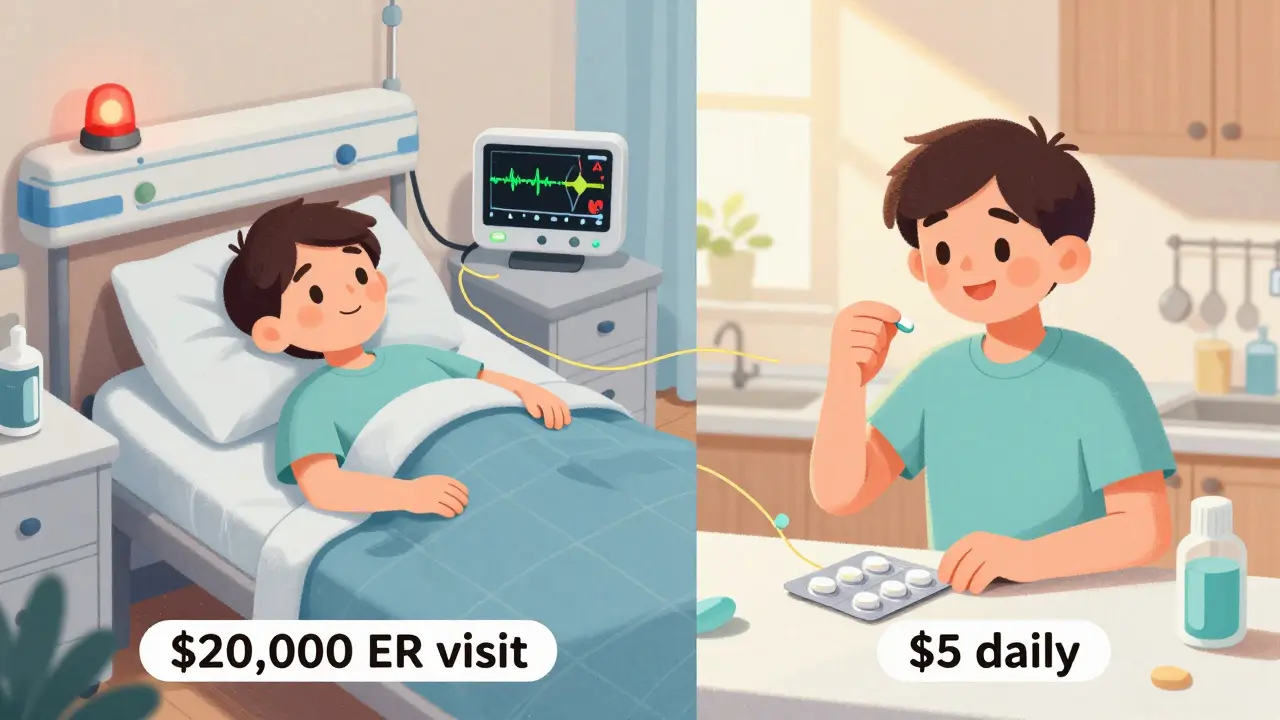
Research shows that when patients face high out-of-pocket costs, they cut corners. They split pills. They delay refills. They stop taking meds entirely. And when that happens, hospitals fill up with preventable emergencies. Heart attacks. Strokes. Diabetic comas. All of it tied back to one simple thing: price.
Generic drugs work just as well - and cost 80% less
Here’s the truth most people don’t know: generic drugs aren’t cheaper because they’re weaker. They’re cheaper because they don’t need to pay for marketing, fancy packaging, or patent lawsuits. The FDA requires generics to have the exact same active ingredient, strength, and dosage form as the brand-name version. They must also prove they’re absorbed into the body at the same rate - within 80% to 125% of the brand drug’s performance. That’s not close. That’s clinically identical.
And the savings? Massive. A statin like brand-name Crestor might cost $75 a month. The generic version, rosuvastatin? $5. Same pill. Same effect. Same doctor’s prescription. Just a fraction of the price. And when patients switch, they stick with it. A 2012 study tracking Medicare patients found that when brand-name statins were moved from a high-cost tier to a low-cost tier, adherence jumped by 5.9%. That’s not a small bump. That’s thousands of people finally taking their meds every day.
Every $10 increase in cost = 2-4% drop in adherence
The link between price and adherence isn’t vague. It’s measurable. Systematic reviews of 160 studies show a clear pattern: the more you pay, the less likely you are to take your medicine. For every $10 rise in out-of-pocket cost, adherence drops by 2% to 4%. In diabetes care, a 2023 study found that each $10 increase in cost led to a 3.7% drop in adherence - and a 5.2% spike in ER visits.
Think about that. A $10 copay difference doesn’t just mean someone’s wallet is lighter. It means someone’s heart is at risk. It means a person with high blood pressure might end up in the hospital - costing the system $15,000 to $25,000 - instead of taking a $5 pill every day.
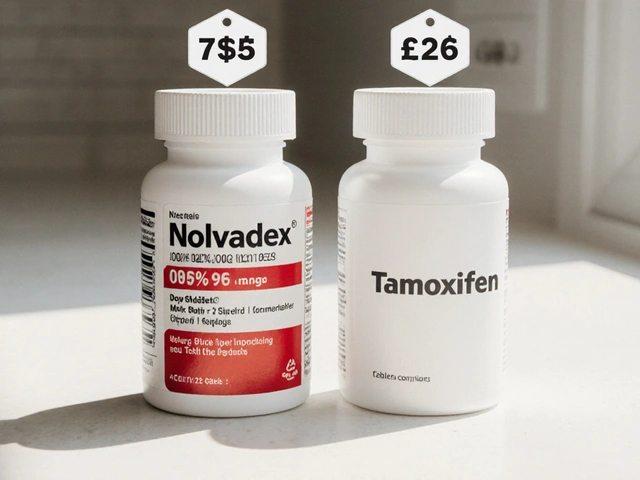
And it’s not just heart meds. For women with early-stage breast cancer on aromatase inhibitors, brand-name users were 22.3% more likely to quit treatment than those on generics. Adherence rates? 68.4% for brand, 73.1% for generic. That 5% gap? It’s the difference between surviving and relapsing.
Real people, real stories
Reddit user u/HeartHealthJourney shared their story in March 2024: “After my cardiologist switched me from brand-name Crestor ($75 copay) to generic rosuvastatin ($5 copay), I went from missing 3-4 doses weekly to perfect adherence for 11 months straight.”
That’s not an outlier. A 2023 JAMA survey of over 2,100 adults found that 32.7% admitted to skipping, cutting, or delaying meds because of cost. Of those, 78% said if they’d known the real price upfront - not just what their insurance said - they wouldn’t have started the drug at all. And 54% said they’d be “moderately or extremely upset” if their doctor didn’t talk about price when prescribing.
People aren’t being lazy. They’re being rational. If you’re choosing between medicine and groceries, you pick groceries. That’s not a moral failure. It’s economics.
Why do brand-name drugs cost so much in the U.S.?
Americans pay 256% more for brand-name drugs than people in Australia, Germany, Canada, or Japan. In 2022-2023, over 4,200 drug prices rose faster than inflation - averaging a $590 increase per product. Meanwhile, generic drugs make up 90% of all prescriptions filled in the U.S., but only 23% of total spending. That’s $643 billion saved between 2009 and 2019 - just from generics.
So why aren’t more doctors pushing generics? Sometimes, it’s habit. Sometimes, it’s lack of time. Sometimes, patients assume “brand = better.” That’s where education matters. The FDA’s “It’s Okay to Use Generics” campaign isn’t just a slogan - it’s a life-saving message.
What’s being done - and what’s working
Change is happening. The Inflation Reduction Act of 2022 capped insulin at $35 a month. Starting in 2025, Medicare Part D will cap out-of-pocket drug spending at $2,000 a year. That’s huge. It could improve adherence for 1.4 million seniors.
Real-time benefit tools (RTBTs) are another game-changer. These are systems built into electronic health records that show a doctor, right at the moment of prescribing, what a drug will cost the patient. Pilots using these tools saw 12-15% improvements in adherence. One program, Magellan’s inforMED, reported a 2:1 return on investment - meaning for every dollar spent on the tool, $2 was saved in avoided hospitalizations.
Pharmacies are helping too. Apps like GoodRx let patients compare prices across local pharmacies - sometimes finding a $10 difference between two stores just five miles apart. That’s not magic. That’s transparency.

The hidden cost of non-adherence
Skipping meds doesn’t just hurt the patient. It hurts everyone. Medication non-adherence causes up to 50% of treatment failures. It contributes to over 100,000 preventable deaths every year in the U.S. And it costs the system between $100 billion and $300 billion annually in avoidable hospital visits, emergency care, and complications.
Meanwhile, patients who stick to their meds have 15-20% fewer hospitalizations. That’s not just better health. That’s fewer ambulance rides, shorter stays, less strain on nurses and doctors.
It’s not about being “responsible.” It’s about removing barriers. If you make a medicine affordable, people will take it. If you don’t, they won’t - no matter how important it is.
What you can do - whether you’re a patient or a caregiver
- Ask your doctor: “Is there a generic version?” Even if you’ve been on a brand drug for years, a switch might be possible.
- Use GoodRx or SingleCare to check prices before you fill your prescription. Sometimes the cash price is lower than your insurance copay.
- Ask about copay assistance programs. Many drugmakers offer discounts for low-income patients.
- If your pharmacy says a drug is “not covered,” ask if there’s an alternative on your plan’s preferred list.
- Talk to your pharmacist. They know which generics work best and which ones are most affordable.
And if you’re a caregiver for someone with chronic illness - don’t just remind them to take their pills. Ask: “Can we afford this?” That question might save a life.
Future trends: Paying for value, not just volume
The next frontier isn’t just lowering prices - it’s aligning costs with outcomes. “Value-based insurance design” means lowering copays for drugs that truly change lives - like blood pressure meds, diabetes drugs, or mental health treatments - even if they’re expensive. Early pilots showed 18.3% higher adherence for these high-value medications.
The FDA is also speeding up generic approvals. Under GDUFA III, $1.1 billion is being invested to bring 1,500+ new generics to market by 2027. That means more options. Lower prices. Fewer excuses.
What’s clear now? Lower generic prices don’t just save money. They save lives. And the data doesn’t lie - when patients can afford their meds, they take them. And when they take them, they stay healthy.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate - within 80% to 125% of the brand drug’s performance. Thousands of studies confirm they work just as well. The only differences are in inactive ingredients like color or filler - which don’t affect how the medicine works.
Why do some people still prefer brand-name drugs?
Some believe brand-name drugs are stronger or more reliable, often because of marketing. Others have had bad experiences with generics - but those are usually due to switching between different generic manufacturers, not because generics are inferior. In rare cases, a patient might react slightly differently to a filler ingredient, but this is uncommon. For most people, switching to generic is safe and effective.
Can I ask my doctor to switch me to a generic?
Absolutely. Doctors are trained to prescribe based on safety, effectiveness, and cost. If you’re struggling to afford your medication, say so. Many doctors will switch you to a generic - or even a different brand-name drug on a lower cost tier - without any loss in effectiveness. Don’t be shy. Your health is worth the conversation.
Why are generic drugs so much cheaper if they’re the same?
Brand-name companies spend billions on research, clinical trials, and marketing to get their drug approved. Once the patent expires, other companies can make the same drug without those upfront costs. They don’t need to advertise. They don’t need to pay for fancy packaging. So they can sell it for 80-85% less. The medicine is identical - the price tag isn’t.
What if my insurance doesn’t cover the generic?
That’s rare, but it can happen if the generic isn’t on your plan’s formulary. Ask your pharmacist if there’s another generic version that is covered. Or ask your doctor to request a formulary exception. You can also use tools like GoodRx to find cash prices - sometimes the out-of-pocket cost is lower than your insurance copay. Don’t assume you have no options.
How do real-time benefit tools help patients?
These tools show doctors the exact out-of-pocket cost for a prescription right at the time they write it. That means they can choose a cheaper alternative before the patient even gets to the pharmacy. In pilot programs, this led to 12-15% more people filling their prescriptions. It removes guesswork and prevents the shock of a $100 bill at the counter.



I used to skip my blood pressure meds till I switched to generic. $5 vs $75? No contest. I started taking them daily. My BP dropped. My bank account didn't cry. Simple as that.
They don't want you to know this but the FDA is in bed with Big Pharma. Generics are just placebos with different labels. They're testing us. You think your $5 pill is the same? It's not. The fillers are designed to make you dependent. Wake up.
I love how this post breaks down the numbers. That 5.9% adherence jump with generics? That's not just statistics-that's people getting to see their grandkids graduate. The real tragedy isn't the price tag, it's the silence around it. Doctors don't talk about cost because they're not trained to. But patients? We're forced to be financial surgeons just to stay alive.
You know what's wild? People act like generics are some kind of compromise. Nah. It's like buying a Toyota Camry instead of a BMW with the same engine. The brand just charges you for the logo. I've been on generic lisinopril for six years. My BP is perfect. My wallet is happier. And no, I don't feel 'second-class'-I feel smart.
Real-time benefit tools are the quiet revolution. I work in primary care. We started using one last year. Prescriptions filled jumped 14%. Patients didn't have to choose between meds and rent. The system was broken. Now we're patching it with tech, not guilt. Doctors aren't villains. We just didn't have the right tools till now.
I'm a pharmacist. I've seen people cry at the counter because their insulin is $400. Then I pull up GoodRx and it's $25. They don't know this stuff exists. No one told them. And yeah, some doctors don't bring it up because they're rushed. But it's not laziness-it's systemic failure. We're treating symptoms while ignoring the root cause: pricing insanity.
This isn't about being cheap. It's about being human. If I have to choose between my asthma inhaler and my daughter's school lunch, I'm picking lunch. No shame. No guilt. Just survival. The fact that we even have to make that choice is the real disease.
America pays too much because we're soft. Other countries negotiate. We let corporations run wild. If you can't afford your meds, you're not poor-you're naive. Get a better job. Move to Canada. Stop whining. This isn't a crisis, it's a consequence.
Let's be honest-adherence isn't the real issue. It's the illusion of control. We pretend that if we just make drugs cheaper, people will magically become responsible. But what about the trauma? The distrust? The mental health crisis? The fact that 40% of Americans can't afford a $400 emergency? You can't fix systemic collapse with a GoodRx coupon. You need revolution.
I'm British. We get generics for free on the NHS. I used to think it was just socialism. Then my cousin came over from Texas with type 2 diabetes. She was skipping doses because her copay was $90. I cried. Not because she was irresponsible. Because the system failed her. We don't treat health like a human right here. But we should.
India makes 70% of the world's generics. We export them to America and you call them 'cheap'? We're the backbone of your healthcare and you treat us like a warehouse. You want lower prices? Then stop blaming the poor. Start taxing the CEOs who hike insulin prices 300% in a year.
bro the FDA is just a puppet 🤡 i took a generic and my heart started racing 😭 they put something in it to make you sick so you buy more pills 💸 #pharmacontrol
I used to think generics were sketchy. Then I got prescribed one for my cholesterol. Same pill. Same results. Saved me $70 a month. I told my whole family. Now my mum's on it too. Simple. Smart. Why is this even a debate?
I dont care what the data says i skipped my meds for 3 months and nothing happened so why bother