 31
Aug,2025
31
Aug,2025
If you keep getting urinary tract infections, you want something that actually stops the cycle-not a quick fix that lasts a week. So, is nitrofurantoin effective for recurrent UTIs? Yes, for many people it cuts infections right down while you’re on it, and resistance stays low. But it’s not for everyone, it’s not good for kidney or prostate infections, and long-term use needs a safety plan. I live in Melbourne, and in clinic here the decision usually comes down to: Does it fit your pattern of UTIs, your kidney function, your goals (antibiotics vs non-antibiotics), and your risk tolerance?
TL;DR
- Effectiveness: Daily or post-sex nitrofurantoin prophylaxis reduces UTIs by about 70-90% while you take it; infections often return after stopping (Cochrane reviews; AUA 2019).
- Best fit: Women with culture-confirmed recurrent cystitis (2 in 6 months or 3 in 12), good kidney function (eGFR ≥30), no signs of kidney/prostate infection.
- Safety: Mostly mild side effects; rare lung, liver, or nerve toxicity with long-term use. Plan baseline checks and 3-6 monthly monitoring.
- Alternatives: Methenamine hippurate is a solid non-antibiotic option (BMJ ALTAR trial 2022 showed non-inferiority to daily antibiotics). Vaginal estrogen helps after menopause.
- Australia 2025: E. coli resistance to nitrofurantoin is still low in the community, which keeps it useful (AURA 2023).
What you likely want to do (jobs to be done)
- Decide if nitrofurantoin is a good match for your type of UTIs.
- Learn the best ways to use it (daily, post-sex, or self-start), with the right dose and duration.
- Set up a simple safety and monitoring plan.
- Compare it with credible alternatives like methenamine hippurate or vaginal estrogen.
- Know when to switch, escalate, or investigate further.
How effective is nitrofurantoin for recurrent UTIs?
First, a quick definition. Recurrent UTI means two proven infections in six months or three in a year. If that’s you, and your episodes are simple bladder infections (stinging pee, urgency, frequency) without fever or flank pain, nitrofurantoin is a credible prevention option.
How well does it work? Across multiple randomized trials and meta-analyses, low-dose antibiotic prophylaxis (including nitrofurantoin) cut recurrences by roughly 70-90% while taken. Many people go from 4-6 UTIs a year down to zero or one. That benefit drops after you stop, so we usually reassess at six months. This pattern shows up in classic Cochrane reviews and is also reflected in the American Urological Association (AUA) 2019 guideline for recurrent UTIs in women.
Resistance matters. Nitrofurantoin works because it concentrates in urine and hits bacterial enzymes in several ways, which makes resistance harder to develop. In Australian primary care data (AURA 2023), community E. coli resistance to nitrofurantoin remains low compared with many other oral antibiotics. That’s a big reason it still sits near the top for uncomplicated cystitis here.
Who benefits most?
- Women with culture-proven recurrent cystitis (no fevers, no flank pain).
- Postmenopausal women, especially if combined with vaginal estrogen (reduces recurrences by restoring the vaginal microbiome; AUA 2019).
- Those whose UTIs are sex-associated, who can use a postcoital dose.
- People with good kidney function: eGFR ≥30 mL/min/1.73 m². Below that, drug levels in urine drop and side effects increase.
Who is it not great for?
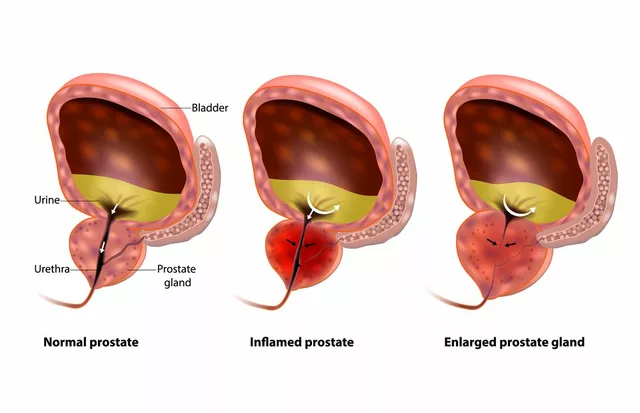
- Suspected kidney infection (fever, back/flank pain, vomiting). Nitrofurantoin doesn’t reach kidney tissue well.
- Most UTIs in men, especially with prostate involvement. It doesn’t penetrate prostate tissue.
- Late pregnancy (around term) and people with G6PD deficiency due to risk of hemolysis; avoid if known G6PD deficiency.
- Anyone with a history of nitrofurantoin-related lung, liver, or nerve issues.
How it stacks up against other strategies? The ALTAR randomized trial (BMJ, 2022) compared daily antibiotic prophylaxis with methenamine hippurate for 12 months and found methenamine was non-inferior in preventing UTIs, with fewer antibiotic resistance issues. That gives people a valid non-antibiotic option. For acute episodes, nitrofurantoin remains a first-line treatment in many guidelines (IDSA; Australian Therapeutic Guidelines) because it works and preserves other antibiotic classes.
| Strategy | Typical Use | Effect on Recurrence | Common Dose | Pros | Watch-outs |
|---|---|---|---|---|---|
| Nitrofurantoin daily prophylaxis | Frequent non-febrile UTIs | ~70-90% reduction while on therapy | 50-100 mg at night for 6-12 months | Low resistance rates; simple dosing | Rare lung/liver toxicity; needs eGFR ≥30 |
| Nitrofurantoin postcoital | Sex-associated UTIs | Similar reduction when sex-triggered | 50-100 mg within 2 hours after sex | Fewer total doses; targeted | Less helpful if UTIs aren’t sex-related |
| Self-start antibiotic (patient-initiated) | Early symptom control; fewer clinic visits | Shortens episodes; reduces complications | Nitrofurantoin 100 mg twice daily for 5 days | Fast relief; culture-directed when possible | Needs a clear plan; rule out red flags |
| Methenamine hippurate | Non-antibiotic prophylaxis | Non-inferior to daily antibiotics in 2022 ALTAR | 1 g twice daily | No classic antibiotic resistance pressure | Works best with acidic urine; avoid with catheters |
| Vaginal estrogen (postmenopausal) | Hormonal atrophy linked UTIs | Reduces recurrences in RCTs | Local cream, tablet, or ring per product | Restores protective flora; very low systemic dose | Not for those with specific estrogen-sensitive cancers unless cleared |
| Cranberry extracts | Adjunct prevention | Modest reduction (Cochrane 2023) | Standardized PAC doses vary | Low risk | Product quality varies; benefits modest |
Key data sources behind these numbers include the AUA 2019 guideline for recurrent UTI, Cochrane reviews on prophylaxis, the 2022 ALTAR trial on methenamine vs antibiotics, the IDSA guidance for acute cystitis dosing, and the 2023 Australian AURA report on resistance.

How to use it safely and smartly (dosing, steps, monitoring)
If you and your clinician decide to try nitrofurantoin, match the regimen to your pattern of infections. Here’s a simple pathway I use with patients.
Step-by-step
- Confirm the pattern. Keep a brief diary: dates, symptoms, any fever/flank pain, and culture results. Recurrent UTI is 2 in 6 months or 3 in 12 months, culture-confirmed.
- Rule out red flags. Go to urgent care if you have fever, back/flank pain, vomiting, pregnancy with fever, or severe illness. That’s not a bladder-only infection.
- Check kidney function. You need eGFR ≥30 mL/min/1.73 m². If there’s chronic kidney disease, adjust the plan.
- Pick the approach:
- Daily prophylaxis: 50-100 mg at night for 6 months, then reassess.
- Postcoital prophylaxis: 50-100 mg within 2 hours of sex if that’s the main trigger.
- Self-start treatment: Keep a 5-day course on hand (100 mg twice daily). Start at first bladder symptoms after submitting a urine sample if possible.
- Combine smart adjuncts. After menopause, add vaginal estrogen unless contraindicated. Consider methenamine hippurate if you prefer to avoid daily antibiotics. Avoid spermicides and diaphragms if they trigger UTIs.
- Plan monitoring. Baseline kidney and liver tests, plus a simple check-in every 3-6 months for symptoms (cough, breathlessness, jaundice, numbness).
- Set stop rules. Stop and call your clinician if you develop new cough or breathing issues, unexplained fatigue, dark urine/yellow eyes, numbness/tingling, or persistent rash.
Dosing cheat sheet
- Acute cystitis treatment: 100 mg twice daily for 5 days (monohydrate/macrocrystals) or 50 mg four times daily for 5 days (immediate release).
- Daily prophylaxis: 50-100 mg once nightly for 6 months (sometimes 12 months if clearly beneficial and safe).
- Postcoital prophylaxis: 50-100 mg within 2 hours after intercourse.
Who should not use it or should be cautious
- eGFR <30 mL/min/1.73 m² (reduced urinary levels, higher risk of toxicity).
- Late pregnancy (around week 38 to delivery) and infants under 1 month if breastfeeding, especially with G6PD deficiency.
- History of nitrofurantoin-related lung, liver, or nerve problems.
- Suspected kidney or prostate infection.
- G6PD deficiency (risk of hemolysis).
Common side effects
- Nausea, headache, mild tummy upset (take with food).
- Dark or brown urine (harmless).
Rare but serious
- Lung problems: cough, breathlessness (can be acute hypersensitivity or chronic interstitial changes with prolonged use).
- Liver injury: fatigue, dark urine, jaundice.
- Peripheral neuropathy: tingling or numbness in hands/feet (more likely with diabetes, B12 deficiency, or renal impairment).
Interactions and practical tips
- Probenecid (and sulfinpyrazone) can raise nitrofurantoin blood levels and lower urinary levels-avoid together.
- Magnesium-containing antacids can reduce absorption-separate by 2-4 hours.
- Alcohol: no specific interaction, but avoid if you’re unwell or dehydrated.
- Birth control: nitrofurantoin doesn’t reduce pill efficacy; vomiting or severe diarrhea can-use backup if that happens.
- Diabetes: monitor for neuropathy symptoms; keep an eye on blood sugars during infections.
Monitoring checklist (simple)
- Before starting: Full symptom history, urine culture, eGFR, liver tests.
- At 3 months: Ask about cough, breathlessness, jaundice, numbness; consider repeat eGFR/LFTs if prolonged therapy.
- At 6 months: Reassess benefit. If UTIs are down and you’re well, consider stopping to test the waters. If they return quickly, discuss another 3-6 months or switch to methenamine.
Pregnancy, breastfeeding, and menopause notes: Most guidelines allow nitrofurantoin in early and mid-pregnancy if needed, but avoid close to delivery. During breastfeeding, it’s usually okay for healthy infants older than a month who are not G6PD deficient. For postmenopausal women, adding vaginal estrogen often cuts UTIs and may let you avoid long-term antibiotics.

Alternatives, trade-offs, and when to switch
If you prefer to avoid long-term antibiotics, or if nitrofurantoin isn’t working or causes side effects, you’re not out of options.
Methenamine hippurate
The 2022 ALTAR trial found methenamine hippurate (1 g twice daily) was non-inferior to daily antibiotics for preventing UTIs over 12 months, with fewer antibiotic-resistant organisms. It works by turning into formaldehyde in acidic urine, which suppresses bacteria. Good fits: people with normal kidneys, acidic urine (vitamin C may help), and no long-term catheters. Less ideal: frequent upper UTIs, alkaline urine that’s hard to acidify, or complicated urinary tracts.
Vaginal estrogen (postmenopausal)
Strong recommendation in AUA 2019: low-dose local estrogen reduces UTI recurrence. Rings, tablets, or creams are all options. It doesn’t act like systemic HRT; systemic absorption is low.
Other antibiotic options
- TMP-SMX or trimethoprim: effective where resistance is low and no allergies, but resistance can be high in some regions.
- Cephalexin: some use 125-250 mg nightly for prophylaxis; watch resistance and gut effects.
- Fosfomycin: great for acute episodes; not usually for long-term prophylaxis.
- Pivmecillinam: useful for acute cystitis in many countries (including Australia); less commonly used for prophylaxis.
Non-antibiotic add-ons
- Cranberry: A 2023 Cochrane review supports a modest reduction in UTIs with standardized cranberry products rich in proanthocyanidins.
- D‑mannose: a large high-quality trial (JAMA, 2024) found no meaningful benefit vs placebo for preventing recurrent UTIs.
- Probiotics: evidence is mixed and mostly weak for UTI prevention.
- Behavioral tweaks: stay hydrated, don’t hold urine too long, urinate after sex, avoid spermicides if they trigger episodes.
When to switch strategies
- Breakthrough infections: If you’re getting 2 or more UTIs during a 6‑month prophylaxis window, review cultures. Switch if the bug is resistant or if the pattern suggests a different trigger.
- Side effects or lab changes: Stop and reassess if you develop lung/liver signals or neuropathy.
- No clear benefit by 3-6 months: Consider methenamine hippurate or add vaginal estrogen.
- Pregnancy planning: Swap to pregnancy‑compatible plans and avoid nitrofurantoin near term.
Mini‑FAQ
- Can I take it long term? Some people use it for 6-12 months safely with monitoring. Longer than that calls for careful risk-benefit review because rare lung or liver toxicity becomes more relevant.
- Will it mess up my gut microbiome? Compared with broad‑spectrum antibiotics, nitrofurantoin is gentler on the gut because it concentrates in urine. Still, any antibiotic can shift flora. Methenamine avoids this issue.
- Does it work for men? Not great for prostate infections. Recurrent UTIs in men often need a deeper workup (prostate, obstruction) and a different antibiotic strategy.
- Alcohol, coffee, spicy food-do they matter? No direct interaction with alcohol, but dehydration and bladder irritation can worsen symptoms. Hydration helps.
- Does it affect birth control? No known effect on the pill. Vomiting/diarrhea from illness can lower pill absorption-use backup if that happens.
- What if cultures are negative but I have symptoms? Consider urethral syndrome, pelvic floor issues, or interstitial cystitis. Repeating antibiotics may not help; ask for a broader evaluation.
Next steps and troubleshooting
- If your UTIs are clearly sex‑associated: Try postcoital nitrofurantoin 50-100 mg plus hydration and urinating after sex. If still frequent, step up to daily prophylaxis or methenamine hippurate.
- If you’re postmenopausal: Add vaginal estrogen early. It can reduce the need for antibiotics and often improves comfort.
- If you have diabetes or neuropathy risks: Keep courses shorter, monitor for tingling or numbness, and check B12 status if symptoms appear.
- If you get a fever or back pain: Stop self‑treatment and seek urgent care-possible kidney infection needs a different antibiotic and sometimes imaging.
- If you travel often: Discuss a standby self‑start plan (e.g., a 5‑day nitrofurantoin course) and a small urine collection kit for culture if feasible.
- If cultures show resistant bugs: Switch antibiotics based on sensitivity. Consider methenamine hippurate to reduce resistance pressure.
- If you’re pregnant or trying: Talk through timing. Early pregnancy may allow nitrofurantoin if needed, but avoid near delivery. Options change trimester by trimester.
Why this guidance is credible
The approach here lines up with: AUA 2019 guideline on recurrent UTIs in women; IDSA and national guidance for acute cystitis dosing; Cochrane reviews showing strong prophylaxis effects while on therapy; the ALTAR trial (BMJ, 2022) on methenamine non‑inferiority; the Australian AURA 2023 report showing low community resistance to nitrofurantoin; and a 2024 JAMA trial showing D‑mannose isn’t effective for prevention. These are the sources clinicians lean on in 2025.
Bottom line: nitrofurantoin is still one of the most reliable options to prevent recurrent bladder infections when used thoughtfully and safely. Pair it with a plan, monitor a few simple things, and be ready to pivot to methenamine or vaginal estrogen if your goals or risks shift. That’s how you break the UTI loop without trading it for a new problem.




Ah, the timeless dance between microbes and medicine! In the quiet corridors of a Melbourne clinic, the decision to wield nitrofurantoin feels like choosing a sword for a specific foe. It cuts down recurrent cystitis with a precision that is almost poetic, yet it demands respect for the kidney’s quiet whispers. One must weigh the rhythm of infections against the subtle hum of side‑effects, lest we trade one torment for another. So, dear reader, let the thought of balance guide you before you press that prescription pad.
What a wonderful deep‑dive into the nitrofurantoin universe! I love how the author has unpacked everything from the nitro‑magic in your bladder to the subtle art of monitoring labs. First, let’s celebrate the fact that a low‑dose antibiotic can slash UTIs by up to ninety percent – that’s a game‑changer for anyone tired of the endless cycle of doctor visits. Second, the safety checklist is like a mini‑roadmap, reminding us that a simple blood test every few months can keep the rare but serious lung or liver troubles at bay. Third, the comparison with methenamine hippurate gives hope to those who crave a non‑antibiotic route, especially post‑menopausal women who can also add vaginal estrogen for a triple‑boost. Fourth, the post‑coital dosing strategy feels like a clever, targeted strike, sparing the body from daily exposure while still pre‑empting the usual suspects after intimacy. Fifth, the crystal‑clear advice on eGFR thresholds ensures that we don’t overstep the boundaries of renal safety – a reminder that the kidneys are the unsung heroes of drug clearance. Sixth, I appreciate the nod to lifestyle tweaks – staying hydrated, urinating after sex, and avoiding spermicides – because sometimes the simplest habits are the most effective. Seventh, the inclusion of a monitoring checklist, complete with symptom flags like cough or numbness, equips patients with a proactive plan rather than passive waiting. Eighth, the mention of pregnancy nuances reminds us that medicine is never one‑size‑fits‑all; timing matters, especially near term. Ninth, the thoughtful integration of behavioral advice, such as adjusting catheter use and maintaining acidic urine for methenamine, showcases a holistic view. Tenth, the author’s grounding in reputable guidelines – AUA, IDSA, Cochrane – gives the whole discussion a sturdy foundation. Eleventh, the style is clear, concise, and yet incredibly thorough – a rare combo in today’s fast‑paced online health content. Twelfth, the emphasis on patient‑specific decision making respects individual values and risk tolerance. Thirteenth, the call to reassess after six months encourages a dynamic, not static, treatment plan. Fourteenth, the clear dosing cheat sheet demystifies the regimens for anyone feeling overwhelmed. Fifteenth, the final takeaway – nitrofurantoin remains a reliable ally when used wisely – feels like a reassuring hand on the shoulder. All in all, this guide is a beacon for anyone navigating the frustrating world of recurrent UTIs, offering both science and compassion in equal measure.
Marvelous exposition! The intertwining of clinical data with patient‑centered nuance reads like a symphonic movement, each instrument – be it nitrofurantoin, methenamine, or estrogen – playing its part in the grand opus of urinary health. One cannot help but admire the precision of the tables, the clarity of the dosing algorithms, and the lyrical flourish that animates even the most mundane laboratory reminder. In particular, the post‑coital dosing strategy resonates like a well‑timed crescendo, striking at the exact moment the pathogen attempts its encore. Moreover, the cautionary notes on eGFR thresholds are a reminder that, even in drama, the foundation must be solid lest the edifice crumble. Finally, the call to reassess every six months invites the reader into an ongoing dialogue with their own body, a dance of vigilance and compassion.
Nice summary 😊
Glad you liked it! A quick heads‑up: when you start nitrofurantoin, make sure to get a baseline eGFR and LFTs. Checking them again at 3‑month intervals catches the rare pulmonary or hepatic signals early, so you can adjust or stop before any serious trouble develops.
We can’t overlook the importance of personalizing therapy. If the infections are clearly sex‑related, a post‑coital dose is often enough – no need for daily pills that may increase risk of adverse events.
Exactly! And remember to stay hydrated – plenty of water helps flush out bacteria. Also, set a reminder on your phone to take the dose within the two‑hour window after intimacy. It’s a small habit but makes a huge difference. 😊
Don’t forget to schedule those blood checks; a quick lab visit is worth the peace of mind.
I appreciate the thoroughness of the guide. The integration of both antibiotic and non‑antibiotic strategies offers a balanced perspective that respects patient autonomy while remaining evidence‑based.
While the exposition is commendably comprehensive, one must remain vigilant against the seductive allure of "low‑resistance" narratives. History teaches us that overreliance on any single antimicrobial inevitably cultivates selective pressure, even for agents such as nitrofurantoin, whose current low resistance may mask an emerging trend. Moreover, the subtle endorsement of methenamine hippurate, though supported by the ALTAR trial, warrants scrutiny regarding its dependence on urinary pH – a variable seldom controlled in routine practice. In short, let us not be lulled into complacency by the veneer of safety; continuous surveillance and judicious stewardship remain paramount.
Great job breaking down the options. For anyone considering estrogen, start with a low‑dose vaginal cream and monitor for any local irritation. Pairing it with a short course of nitrofurantoin can often bridge the gap while the microbiome rebalances.
Sounds like a plan but I think the pharma lobby is pushing these meds to keep us dependent they want us on antibiotics forever
All these “alternatives” are just marketing gimmicks. Stick to proven antibiotics.
Your concern about marketing is understandable; however, the data from the ALTAR trial and subsequent meta‑analyses demonstrate that methenamine hippurate offers a non‑antibiotic pathway with comparable efficacy. It is prudent to discuss both options with patients, allowing informed choice while maintaining antimicrobial stewardship.
Look i dont c how this works but i think u should just take the lad buy cheap and dont over think it
Ah, the simplicity of “just take the cheap pill” – a truly avant‑garde approach to modern medicine. One could argue that such an attitude epitomises the very essence of patient‑centred care: empowering individuals to make uninformed choices with reckless abandon. Yet, perhaps the sarcasm is a veil for genuine concern: the ease of a cheap tablet might lure patients into a false sense of security while ignoring the nuanced balance of renal function, resistance patterns, and the ever‑present spectre of pulmonary toxicity. In any case, let us not reduce complex pharmacotherapy to a one‑liner; the art lies in nuance, not in the blunt instrument of “just take it”.
The guide is well‑structured, yet a few linguistic refinements could enhance clarity. For instance, the phrase “Nitrofurantoin cuts infections right down while you’re on it” would benefit from the adverbial clause “while you are actively taking the medication,” thereby eliminating any potential ambiguity. Additionally, the list of side effects should be presented in parallel grammatical form – e.g., “nausea, headache, and mild gastrointestinal upset” – to maintain syntactic consistency. Such modest edits preserve the document’s scientific rigor while ensuring the prose remains impeccably polished.
Thanks for the edit tips! i think it looks good now but u kno sometimes i crush typos when i r typing fast lol. The content is still on point and i prefer the dramtic tone you used it makes rading more
engaging!.
Everyone’s talking about nitrofurantoin like it’s some harmless wonder‑drug, but have you considered who’s really profiting? The big pharma syndicate has been quietly funding “research” to keep us on antibiotics while they pull the strings behind the scenes. Even the “low resistance” numbers are suspiciously perfect – a classic data‑fabrication play to keep the market saturated. Stay woke, question the source, and don’t let them dictate your health decisions.