 19
Oct,2025
19
Oct,2025
When you’re dealing with angina or other forms of ischemic heart disease, the sheer number of pills on the shelf can feel overwhelming. One name that often pops up in specialist clinics is Vastarel. But how does it really stack up against the more familiar beta‑blockers, nitrates, or newer agents like ranolazine? This guide walks you through the science, the side‑effect profiles, and the practical considerations so you can decide whether Trimetazidine Dihydrochloride-or one of its alternatives-fits your treatment plan.
Key Takeaways
- Vastarel (Trimetazidine) works by improving cellular energy use, not by lowering heart rate or blood pressure.
- Its main advantage is fewer systemic cardiovascular effects, making it useful for patients who can’t tolerate beta‑blockers.
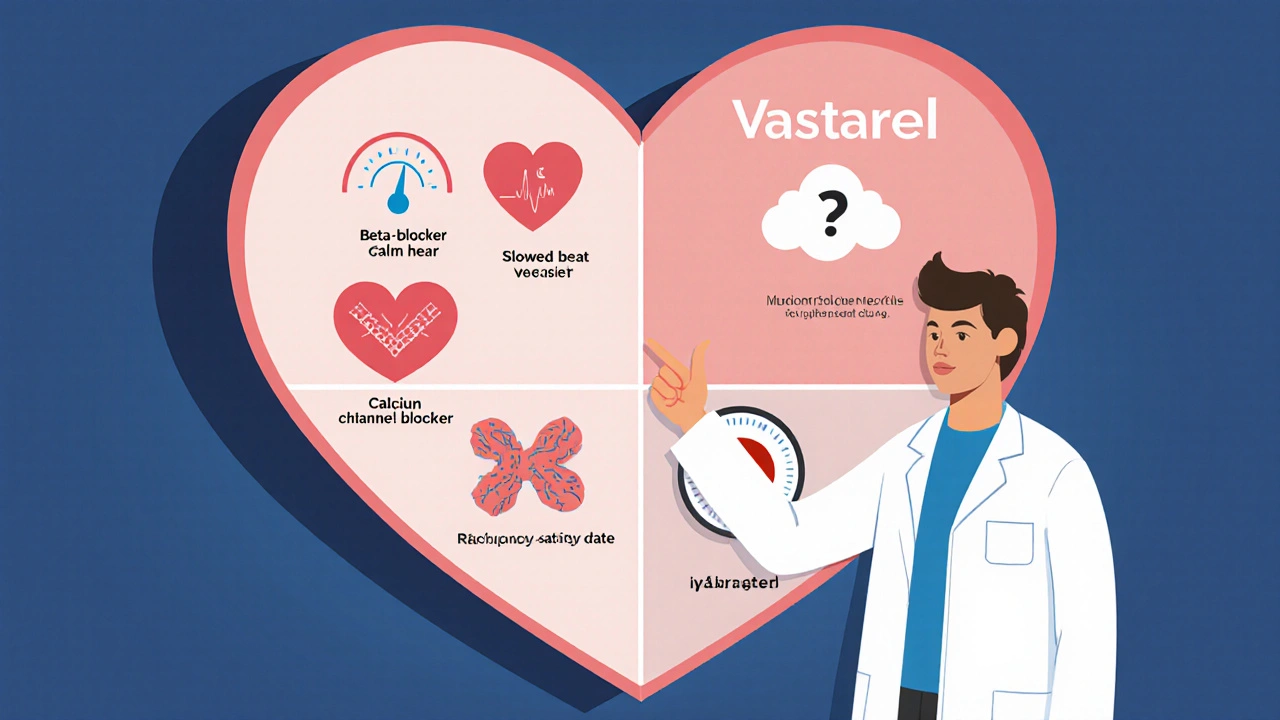
- Alternatives such as beta‑blockers, calcium channel blockers, and ranolazine each have distinct mechanisms and side‑effect trade‑offs.
- Cost and regulatory status vary by region; in the EU Trimetazidine is prescription‑only, while it’s banned for performance‑enhancing use in sport.
- Choosing the right drug depends on symptom pattern, comorbidities, and personal tolerance.
What Is Vastarel (Trimetazidine Dihydrochloride)?
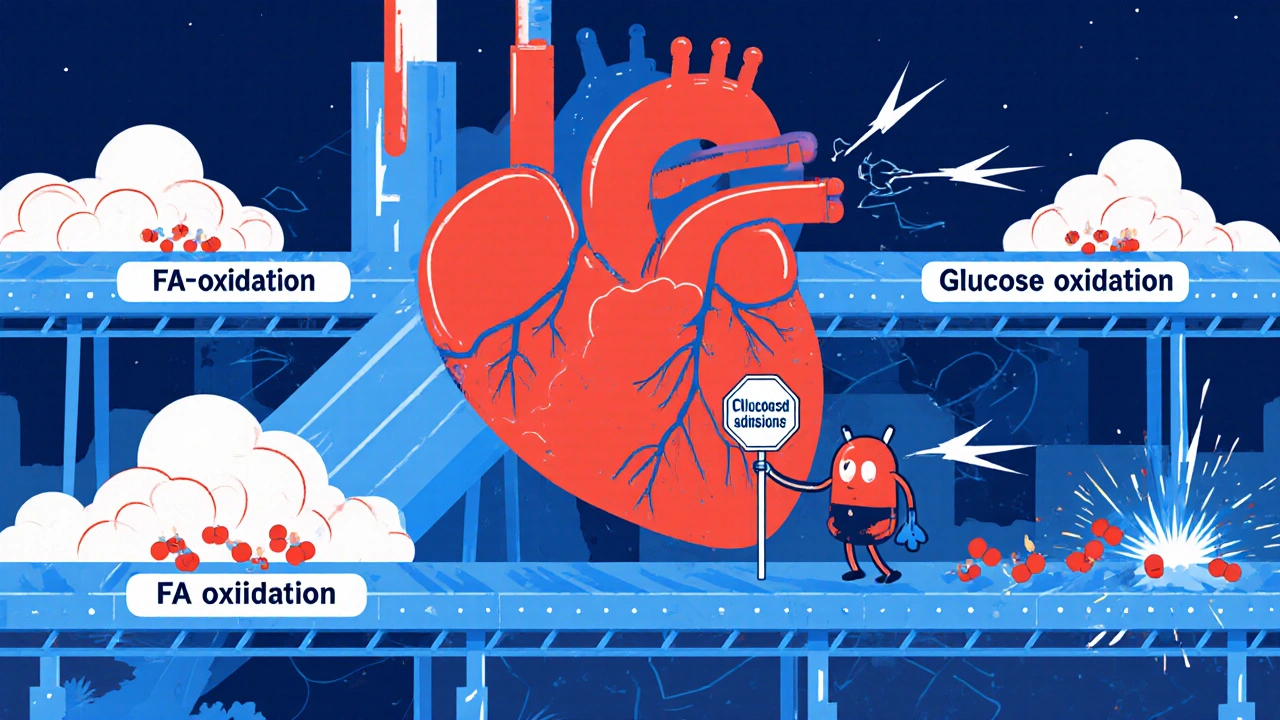
Vastarel (Trimetazidine Dihydrochloride) is a metabolic agent approved in many countries for the treatment of stable angina pectoris and, in some regions, for peripheral arterial disease. The active molecule, trimetazidine, belongs to the class of cell‑protective agents that shift heart‑muscle metabolism from fatty‑acid oxidation toward glucose oxidation, a more oxygen‑efficient pathway.
How Trimetazidine Works: The Metabolic Angle
The heart normally burns about 70% of its energy from fatty acids and the rest from glucose. Under ischemic conditions-when oxygen supply is limited-fatty‑acid oxidation becomes wasteful because it consumes more oxygen per ATP molecule produced. Trimetazidine inhibits the enzyme 3‑ketoacyl‑CoA thiolase, a key step in fatty‑acid breakdown. By throttling this pathway, cells rely more on glucose, which yields more ATP per oxygen molecule. The result is better contractile performance without changing heart rate or blood pressure.
This mechanism makes Trimetazidine attractive for patients who cannot tolerate drugs that blunt the sympathetic nervous system (beta‑blockers) or cause vasodilation (nitrates).
Who Typically Uses Vastarel?
Doctors prescribe Trimetazidine for patients with chronic stable angina who continue to have chest pain despite optimal dose of first‑line agents. It’s also used off‑label in some European clinics for:
- Peripheral arterial disease (PAD) where muscle oxygenation is compromised.
- Heart failure with preserved ejection fraction, although evidence is still emerging.
Because it does not affect heart rate, it’s a safe add‑on for athletes (where allowed) and for elderly patients prone to bradycardia.
Common Alternatives to Trimetazidine
Below are the main drug families you’ll hear about when discussing angina management.
Beta‑Blockers
Examples: metoprolol, atenolol, propranolol. These blunt the heart’s response to adrenaline, lowering heart rate and contractility, which reduces oxygen demand.
Calcium Channel Blockers (CCBs)
Examples: amlodipine, diltiazem, verapamil. They dilate coronary vessels and decrease afterload, easing the work the heart has to do.
Nitrates
Examples: glyceryl trinitrate (GTN), isosorbide dinitrate. These release nitric oxide, causing rapid vasodilation of both veins and arteries, which reduces preload and improves coronary blood flow.
Ranolazine
Ranolazine (brand name Ranexa) inhibits the late sodium current in cardiac cells, reducing intracellular calcium overload and improving myocardial relaxation.
Ivabradine
Ivabradine (brand Corlanor) selectively slows the pacemaker current (If) in the sinus node, lowering heart rate without affecting contractility.
Head‑to‑Head Comparison Table
| Drug | Mechanism | Primary Indication | Typical Dose | Common Side Effects | Cost (USD/month) |
|---|---|---|---|---|---|
| Vastarel (Trimetazidine) | Shifts metabolism from fatty‑acid to glucose oxidation | Stable angina, peripheral arterial disease | 35 mg twice daily | Gastro‑intestinal upset, headache, rare movement disorders | $30-$45 |
| Metoprolol (Beta‑blocker) | Blocks β‑adrenergic receptors → lowers HR & contractility | Stable angina, hypertension, post‑MI | 50-100 mg daily | Bradycardia, fatigue, depression | $10-$20 |
| Amlodipine (CCB) | L-type calcium channel antagonism → vasodilation | Angina, hypertension | 5-10 mg daily | Peripheral edema, flushing, gingival hyperplasia | $8-$15 |
| GTN (Nitrate) | NO donor → venous & arterial dilation | Acute angina relief | 0.4 mg sublingual PRN | Headache, hypotension, tolerance | $5-$12 |
| Ranolazine | Inhibits late Na⁺ current → improves relaxation | Chronic angina (add‑on) | 500 mg twice daily | Dizziness, constipation, QT prolongation | $120-$150 |
| Ivabradine | Selective If current inhibition → HR reduction | Angina, heart failure with HR > 70 bpm | 5-7.5 mg twice daily | Bradycardia, luminous phenomena | $80-$100 |
Pros and Cons of Vastarel Compared to Alternatives
Advantages of Trimetazidine
- Does not lower blood pressure or heart rate, preserving exercise tolerance.
- Works synergistically with beta‑blockers or nitrates-often added as a third‑line drug.
- Low incidence of severe cardiovascular side effects.
Limitations
- Gastro‑intestinal discomfort is the most common complaint.
- Rare reports of movement disorders (parkinsonian symptoms) led to restricted use in the EU for athletes.
- Cost is higher than generic beta‑blockers or CCBs in many markets.
In contrast, beta‑blockers excel at reducing mortality after myocardial infarction but can cause fatigue and are unsuitable for asthmatics. Nitrates relieve acute pain quickly but develop tolerance within weeks. Ranolazine is potent for refractory angina but its price and QT‑prolongation risk keep it as a specialty add‑on.
How to Choose the Right Agent for You
When deciding between Vastarel and its peers, ask yourself these practical questions:
- What’s my main symptom pattern? If you need rapid relief during an attack, short‑acting nitrates are unbeatable. For chronic symptom reduction, consider metabolic agents like Trimetazidine or ranolazine.
- Do I have comorbid conditions? Asthma, COPD, or severe bradycardia push you away from beta‑blockers. Kidney disease may affect dosing of certain CCBs.
- How tolerant am I of side effects? If headaches from nitrates or edema from amlodipine bother you, Trimetazidine’s milder profile might be preferable.
- What does my insurance cover? Generic beta‑blockers and CCBs often have the lowest out‑of‑pocket cost. Trimetazidine may need prior authorization.
- Am I an athlete? In many sports federations, Trimetazidine is on the prohibited list, so discuss alternatives with your physician.
Most clinicians adopt a stepwise approach: start with a beta‑blocker or CCB, add a nitrate for acute relief, and consider Trimetazidine or ranolazine when symptoms persist.
Frequently Asked Questions
Is Trimetazidine safe for long‑term use?
Clinical trials up to five years have not shown an increase in mortality. The main safety concerns are mild gastrointestinal upset and very rare movement‑disorder reports. Regular follow‑up every 6-12 months is advisable.
Can I take Trimetazidine together with beta‑blockers?
Yes. Because Trimetazidine works on cellular metabolism rather than heart rate, it complements beta‑blockers without causing additive bradycardia or hypotension. Many cardiologists prescribe them together for refractory angina.
Why is Trimetazidine banned in professional sports?
The World Anti‑Doping Agency (WADA) lists Trimetazidine as a prohibited substance because it can enhance cardiac efficiency during intense exercise, giving an unfair endurance advantage.
How quickly does Trimetazidine start working?
Therapeutic effects usually appear after 1-2 weeks of consistent dosing, as the heart’s metabolic shift gradually improves oxygen utilization.
Is there a generic version of Vastarel?
In many European and Asian markets, trimetazidine is sold under various generic names, often at a lower price than the branded Vastarel tablets.
Bottom line: Trimetazidine isn’t a first‑line therapy for every angina patient, but it fills a valuable niche when conventional drugs fall short or cause intolerable side effects. Talk to your cardiologist about where it fits into your personalized treatment plan.



Honestly, the whole hype around Vastarel feels like a marketing gimmick. It promises a metabolic miracle, yet the clinical data barely outshine cheap beta‑blockers. If you’re flipping through the side‑effect list, you’ll see mild GI upset, but you also get a price tag that most insurance plans balk at. For a drug that doesn’t even lower heart rate or blood pressure, the justification for putting it on a pill‑board seems thin. In practice, I’ve seen patients who could have been steadied on metoprolol without the extra paperwork. So unless you have a very specific intolerance to first‑line agents, Vastarel is more fluff than substance.
Hey, I get where you’re coming from, but there are folks who actually feel better on Trimetazidine. When beta‑blockers cause fatigue or bronchospasm, this metabolic shift can be a lifesaver. It’s not a silver bullet, but having another tool in the toolbox isn’t a bad thing.
Let me unpack the hidden layers behind the approval of Trimetazidine. The pharmaceutical conglomerates have long been embedding metabolic modulators into the angina market, a niche that the traditional sympatholytics can’t touch without side‑effects. What’s rarely disclosed is the entanglement with regulatory capture: lobbyists have nudged agencies to classify this agent as “essential” despite the modest absolute risk reduction. Moreover, the post‑marketing surveillance data, buried deep in obscure EU registries, hint at a disproportionate incidence of movement disorders, suggesting a neuro‑toxic sub‑population that’s been quietly dismissed as “rare”. The timing of the drug’s introduction coincides with a wave of patent extensions for older beta‑blockers, a classic case of product‑life‑cycle management. Add to that the fact that elite sports bodies banned it only after whistleblowers exposed its subtle performance‑enhancing properties, raising the question: if the drug truly improves cardiac efficiency, why hide that fact from the public? The metabolic shift from fatty‑acid to glucose oxidation sounds scientific, but in reality it’s a clever re‑branding of a modest oxidative stabilizer. The cost escalation-$30 to $45 a month-outpaces generic alternatives, pointing to profit motives rather than pure therapeutic need. In short, while the drug may have a place for certain refractory patients, the broader narrative is one of strategic market positioning, regulatory maneuvering, and selective data disclosure.
The mechanistic rationale you outlined aligns with the pharmacodynamic profile of trimetazidine. Specifically, the inhibition of 3‑ketoacyl‑CoA thiolase redirects myocardial substrate utilization toward glycolysis, thereby enhancing ATP yield per unit of O₂ consumed. Clinical meta‑analyses have reported a modest improvement in exercise tolerance, quantified as a 1.2‑minute increase in treadmill duration (p<0.05). However, the incidence of extrapyramidal symptoms-approximately 0.02% in pooled cohorts-necessitates vigilant monitoring, particularly in patients with pre‑existing movement disorders. From a formulary standpoint, the cost‑effectiveness ratio is borderline, given the incremental quality‑adjusted life year (QALY) gain of 0.03. Thus, the drug’s utility is best confined to a niche of β‑blocker‑intolerant individuals with persistent angina despite optimal conventional therapy.
Trimetazidine feels like a secret weapon for the tired heart.
While brevity has its charm, it’s worth noting that any decision to add a metabolic agent should be made after a thorough assessment of the patient’s comorbid conditions and current medication regimen. In practice, we often schedule a follow‑up visit at six weeks to assess tolerance and efficacy before considering further escalation.
Alright, let’s break this down in plain English for everyone who’s ever stared at a pile of pill bottles and felt like they were reading a chemistry textbook. First off, you’ve got your classic players: beta‑blockers, calcium channel blockers, nitrates – they’re the rock stars of the angina world, keeping the heart rate low, dilating vessels, or just giving you a quick win when you feel that chest squeeze. Then comes Trimetazidine, the underdog that doesn’t try to be a headliner; it quietly tells heart cells, “Hey, let’s burn sugar instead of fat because it’s more efficient when oxygen’s scarce.”
Now, why does that matter? Because sugar burns cleaner, you get more bang for your oxygen buck, and theoretically, you feel less pain during those tight spots. The catch? It’s not a miracle cure – it won’t drop your blood pressure, and it won’t make you run a marathon without feeling winded. It’s more like a sidekick that helps when the main heroes are either out of the picture or causing you too many side‑effects.
Patients who can’t take beta‑blockers because they’re asthmatic or bruise easily from low blood pressure often find Trimetazidine a decent add‑on. The side‑effects are usually mild – a bit of nausea or a headache – but there’s a tiny chance you might develop tremors or, in rare cases, movement issues that look a bit like Parkinson’s. Cost is another story; you’ll pay more than a generic metoprolol, but often less than the pricey ranolazine.
Bottom line: think of Trimetazidine as a backup singer. It doesn’t steal the spotlight, but it can keep the show running smoothly when the lead singers need a break. Talk to your doc about whether that backup role fits your specific health concert.
The analogy of a backup singer is apt. In clinical practice, we usually re‑evaluate symptom frequency after six to eight weeks of add‑on therapy to determine true benefit.
Enough with the buzzwords – the heart doesn’t care about your marketing spin.