 7
Nov,2025
7
Nov,2025
When you pick up a prescription, you might not think about what happens after it hits the shelf. But drugs don’t stay the same forever. New risks can show up months or even years later-side effects that weren’t obvious during clinical trials, dangerous interactions with other meds, or dosing mistakes that led to harm. That’s where the FDA Safety Communications come in. These aren’t ads or press releases. They’re official, science-backed updates from the U.S. Food and Drug Administration telling you and your doctor about real, current dangers tied to your medication.
What Are FDA Safety Communications, Really?
The FDA doesn’t just approve drugs and walk away. Once a medicine is out in the real world, used by millions, new patterns emerge. Maybe 10 people reported a rare heart rhythm issue. Maybe a study found a higher chance of liver damage in older adults. When enough evidence builds up, the FDA issues a Drug Safety Communication. These aren’t rare. Between 2020 and 2023, the FDA released 50 to 70 of these each year. They’re not all the same. Some are urgent alerts-like a recall or a boxed warning. Others are updates to the prescribing info, changes to how a drug should be used. The FDA sorts them into types: Drug Safety Communications (the full version), Drug Alerts (shorter, urgent), labeling changes, recalls, and compounding risk notices. You’ll see these on the FDA’s website under Drug Safety and Availability.How to Find the Right Communication
You don’t have to scroll through hundreds of posts. The FDA lets you sign up for email alerts. Go to the FDA’s Drug Safety page and look for the subscription option. You can pick your meds by name or by class-like all opioids, all diabetes drugs, or all antidepressants. That way, you only get alerts about what matters to you. No noise. Just the updates that affect your treatment. If you’re not signed up, search for the drug name + “FDA Safety Communication” on the FDA site. Make sure you’re on the official .gov domain. Fake sites or pharmacy blogs might misrepresent what’s really happening.Breaking Down the Document: What to Look For
Every FDA Safety Communication follows a clear structure. You don’t need a medical degree to read it-you just need to know where to look. First: “What Safety Concern Is FDA Announcing?” This is the headline. It tells you the problem in plain language. For example: “FDA warns of increased risk of serious infections with a certain diabetes drug.” That’s it. No jargon. No fluff. Then: “For Patients” Section This is your part. It tells you what to do. It might say:- “Do not stop taking this medicine without talking to your doctor.”
- “Call your doctor right away if you notice swelling in your legs or sudden weight gain.”
- “Read the Medication Guide every time you refill your prescription.”
Understanding Labeling Changes
Sometimes, the FDA doesn’t issue a new warning. It just updates the drug’s official label-the legal document that tells doctors how to use the medicine. These changes can be tiny but critical. For example, in a 2025 opioid safety update, the FDA changed the wording from “Do not abruptly discontinue” to “Do not rapidly reduce or abruptly discontinue.” Why? Because research showed that even a fast taper-not just stopping cold-could trigger dangerous withdrawal or rebound pain. The change was small, but the meaning was huge. The FDA shows you exactly what changed: old text in strikethrough, new text in bold. They even list the section numbers (like “2.x, 5.x”) so doctors can find it in the full prescribing document. You won’t need these numbers-but if your doctor says, “The label changed,” you can ask: “Which part?” and they’ll know you’re paying attention.
What’s Not in the Communication
Here’s what the FDA doesn’t tell you:- It doesn’t say if you should stop the drug.
- It doesn’t compare drugs.
- It doesn’t tell you about cheaper alternatives.
When to Act Immediately
Not every alert needs you to drop everything. But some do. Here’s how to tell:- STOP using the drug immediately → This means stop taking it now. Call your doctor or go to urgent care. This is rare, but it happens-for example, if a drug is linked to sudden, fatal liver damage.
- Do not stop without talking to your doctor → This means the risk is real, but stopping suddenly could be worse. Think: antidepressants, seizure meds, or steroids. Abruptly quitting can cause seizures, rebound anxiety, or adrenal crisis.
- Monitor for symptoms → This means keep taking the drug but watch for signs like unusual bruising, chest pain, or confusion. Report them right away.
Why This Matters for You
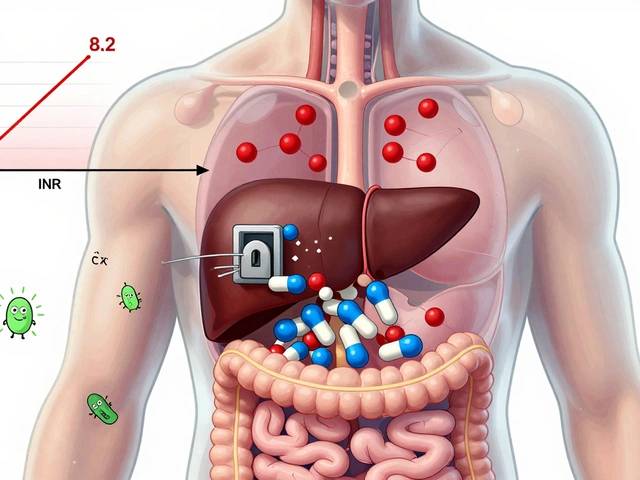
Imagine you’ve been on a blood thinner for five years. You feel fine. Then, in 2024, the FDA issues a communication: “New data shows increased bleeding risk in patients over 75.” You’re 78. You didn’t know. You didn’t get a letter. But now you know. You talk to your doctor. They check your blood levels. They adjust your dose. You avoid a hospital visit. That’s the power of these communications. They’re not fear-mongering. They’re risk management. And they’re your right to know.
What Patients Say
On patient forums, people often confuse FDA Drug Alerts with full Safety Communications. One Reddit user thought a minor alert about a stomach upset was a recall. Another patient stopped her insulin because she misread a warning. That’s dangerous. The FDA’s own surveys show only 54% of patients fully understand what these alerts mean. That’s why they’re rolling out plain-language summaries in English and Spanish-and testing visual icons (like a red stop sign for urgent actions) to make it clearer.What You Can Do Today
1. Sign up for email alerts on the FDA’s Drug Safety page. Pick your meds. 2. Keep every Medication Guide you get. File them. Re-read them each refill. 3. Ask your pharmacist if there’s been a recent FDA update on your drug. Pharmacists get these alerts too. 4. Ask your doctor: “Has there been any new safety info on this drug?” Don’t wait for them to bring it up. 5. Don’t stop or change your dose based on an alert alone. Always talk to your provider first.What’s Changing Soon
The FDA is moving faster. Under the 2022 Food and Drug Omnibus Reform Act, they now have to issue safety updates within 30 days of a major finding-down from 60. They’re also testing personalized alerts through patient portals. By 2025, you might get a notification in your MyChart account if your drug gets a new warning. The goal? Get the right info to the right person, at the right time. No more delays. No more confusion.Reading an FDA Safety Communication isn’t about becoming a scientist. It’s about becoming an informed patient. You don’t need to understand every technical detail. You just need to know where to look, what to ask, and when to act.
Are FDA Safety Communications the same as drug recalls?
No. A drug recall means the product is pulled from shelves because it’s contaminated, mislabeled, or unsafe to use. FDA Safety Communications are warnings about new risks that may require changes to how the drug is used-like updating dosing instructions or adding a new warning. You usually don’t need to return your pills unless the FDA specifically says to.
Can I trust FDA Safety Communications?
Yes. The FDA bases these on real-world data from doctors, patients, clinical studies, and national databases. They don’t issue them lightly. Each one goes through rigorous review by scientists, clinicians, and regulatory experts. While no system is perfect, the FDA is one of the most trusted drug safety agencies in the world.
Why do some drugs get safety alerts years after they’re approved?
Clinical trials involve thousands of people, but real-world use involves millions. Rare side effects, interactions with other meds, or risks in older or sicker patients often only show up after years of use. The FDA monitors this through systems like the Sentinel Initiative, which tracks health records from over 200 million people. It takes time to spot patterns-but once they’re clear, the FDA acts.
Do these alerts apply to generics too?
Yes. If the alert is about a drug’s active ingredient, it applies to all versions-brand name and generic. For example, if the FDA issues a warning about “metformin,” it applies to all metformin tablets, regardless of the manufacturer. The FDA lists the active ingredient clearly in each communication.
What if I can’t understand the communication?
Don’t guess. Call your doctor or pharmacist. Ask them to explain it in simple terms. You can also ask for the “Highlights of Prescribing Information” version, which is shorter and easier to read. The FDA now offers plain-language summaries for high-risk drugs in both English and Spanish. If you’re still unsure, ask for a written summary you can take home.



Just signed up for the FDA alerts for my blood pressure med-finally got tired of guessing if my weird dizziness was me or the drug. Best decision this year.
OMG I JUST REALIZED I’VE BEEN THROWING OUT MY MEDICATION GUIDES LIKE GROCERY LIST PAPER??? 😱 I’M READING MINE TONIGHT
Most people can’t even spell ‘pharmacokinetics’ but somehow think they’re qualified to interpret FDA alerts? Look, if you need a 10-step guide to read a .gov page, maybe don’t self-diagnose with WebMD. The FDA isn’t TikTok.
i just want to say that i think this is so important because a lot of people dont realize that just because a drug is on the shelf doesnt mean its safe forever and i used to think that if my doctor prescribed it then its fine forever but that’s not true at all and i learned this the hard way when my friend had that reaction to her antibiotic and no one knew until the FDA posted it and honestly i wish i had known sooner because now i keep all my guides in a folder and i read them every time i get a refill and i even ask my pharmacist if anything changed and it makes me feel way more in control like im not just a passive person taking pills
Small change, huge impact. That opioid wording shift from ‘abruptly discontinue’ to ‘rapidly reduce or abruptly discontinue’? That’s the kind of precision that saves lives. Kudos to the FDA for getting the language right.
why do americans always make everything so complicated? in india we just take what doctor says and dont ask questions. why read all this? you think FDA knows better than your doctor? lol
Thank you for writing this in a way that actually feels human. I’m a single mom of three and I don’t have time to be a medical researcher-but I do have time to open an email and read two sentences. This guide? It’s the kind of thing that makes me feel like I’m not failing my family just because I’m not a doctor.
Generic drugs are included yes but do you know how many people think brand name is the only one with warnings? I had a cousin stop metformin because he thought only Glucophage had the alert. He ended up in ER. This needs more outreach.
Wait so you’re saying I’m supposed to actually read the tiny booklet that comes with my pills? Like, the one I’ve been using as a coaster for my coffee? That’s… a lot. I just want to feel better. Why does everything have to be so much work?
Oh, wonderful. Another 12-page, hyper-formal, bureaucratically overwrought, comma-spliced, semicolon-abusing, passive-voice-laden, FDA-issued monstrosity that only a pharmacologist with a thesaurus and a caffeine IV could parse. And you expect *me*-a person who just wants to take my pill and not die-to read this like it’s Shakespeare? The FDA should be sued for emotional abuse.
My grandma started reading her guides after I showed her how to find the ‘For Patients’ section. She now calls me every time she gets a new refill. We talk about it like a book club. It’s weirdly beautiful.
Ugh. Another ‘FDA says’ article. Next they’ll tell us to brush our teeth with our left hand while standing on one foot. This is just fearmongering dressed up as ‘safety.’ My uncle took this same drug for 20 years and he’s still alive. The FDA just wants to make themselves look important.
It is imperative that patients understand that the issuance of a Drug Safety Communication constitutes a formal regulatory action predicated upon empirical evidence derived from post-marketing surveillance systems. This is not conjecture; it is evidence-based pharmacovigilance at its most rigorous.
I wonder how many people feel like they’re being punished for being sick. Like, you’re already dealing with pain or anxiety or high blood pressure, and now you have to become a detective just to stay alive? It’s not just about reading the alert-it’s about being told you’re not enough unless you’re also a scientist. That’s heavy.
Love that the FDA is testing visual icons-like a red stop sign. Simple, universal. I’m from the UK and even I get confused by all this text. A picture says a thousand words, especially when you’re stressed or tired.