 10
Jan,2026
10
Jan,2026
Ever wonder why a pill you swallow can calm your headache, lower your blood pressure, or fight an infection? It’s not magic. It’s chemistry. Every medicine you take - whether it’s aspirin, antibiotics, or antidepressants - works by interacting with your body at a molecular level. But knowing how medicines work isn’t just for doctors. It’s the key to using them safely.
How Medicines Actually Work
Medicines don’t float around your body randomly looking for trouble. They’re designed to fit into specific spots, like keys into locks. These spots are called receptors, enzymes, or transporters - tiny structures on or inside your cells. When a medicine binds to one of these, it changes how the cell behaves. Take aspirin. It blocks an enzyme called COX-1, which makes chemicals that cause pain and swelling. No enzyme, no pain signal. Simple. SSRIs like fluoxetine (Prozac) work differently. They stop nerve cells from reabsorbing serotonin - the brain chemical linked to mood. By keeping more serotonin active, they help lift depression. It’s not just about adding something new; it’s about changing how your body already works. Some medicines work locally. Laxatives act right in your gut. Antacids sit in your stomach. Others travel through your bloodstream to reach faraway targets. That’s why a pill for arthritis doesn’t just affect your knee - it circulates everywhere. But not every part of your body is equally accessible. The blood-brain barrier, for example, protects your brain from toxins. Only certain drugs, like the Parkinson’s treatment Sinemet®, are built to slip through it.Why Protein Binding Matters
Once in your blood, most medicines stick to proteins - often 95% or more. That’s not a bad thing. It keeps them from being flushed out too fast. But here’s the catch: only the 5% or less that’s floating free can actually do its job. If you take another drug that also binds to those same proteins, it can push your medicine off. Suddenly, more of it is active. That’s how warfarin, a blood thinner, can become dangerously strong if you start taking a common antibiotic like sulfonamide. Your free warfarin level can jump by 20-30%, raising your risk of bleeding. This isn’t rare. It’s a known interaction - and one you can avoid if you understand how it works.First-Pass Effect and Why Doses Vary
Not every pill you swallow makes it into your bloodstream. When you take medicine orally, it goes through your liver before entering circulation. The liver breaks down some of it. This is called the first-pass effect. Morphine loses about 30% this way. Propranolol? Up to 90%. That’s why some drugs need much higher doses than others. If your liver processes a drug fast, you might need to take it more often. If it’s slow, even a small dose could build up and cause side effects. That’s why your doctor doesn’t just give everyone the same amount.
When Medications Are Safe to Use
Safety isn’t just about following the label. It’s about matching the drug to your body - and knowing what can go wrong. Take lithium, used for bipolar disorder. It’s effective - but the line between helpful and toxic is thin. Blood levels must stay between 0.6 and 1.2 mmol/L. Too low? It won’t work. Too high? You could end up in the hospital with tremors, confusion, or kidney damage. Why? Because lithium doesn’t have one clear target. It affects multiple systems. That’s why doctors check your blood regularly. You can’t guess this. You need testing. Or consider warfarin. It’s been around for decades. But because it blocks vitamin K - a nutrient in spinach, kale, and broccoli - your diet matters. Eat a big salad one day, then none for a week? Your INR (a blood test that measures clotting) can swing wildly. Patients who understand this don’t just avoid greens - they eat them consistently. That’s the difference between safety and danger.Why Knowing the Mechanism Reduces Risk
In 2023, the FDA reported that 32% of adverse drug events came from patients who didn’t understand how their medicine worked. Think about MAO inhibitors, used for depression. If you eat aged cheese, cured meats, or red wine while on them, you can trigger a sudden, deadly spike in blood pressure. Why? Because these foods contain tyramine - and MAO inhibitors stop your body from breaking it down. One ounce of blue cheese has 1-5 mg of tyramine. Enough to cause a crisis. But if you know why, you avoid it. Simple. On the flip side, patients on trastuzumab (Herceptin) for breast cancer are tested for HER2 protein before treatment. If the tumor has it, the drug works. If not, it won’t. That’s precision medicine. And patients who understand this feel more in control. A 2023 survey found that 78% of those who knew how Herceptin worked felt confident about safety - and 63% could spot heart problems early, a known side effect. That’s not luck. That’s knowledge.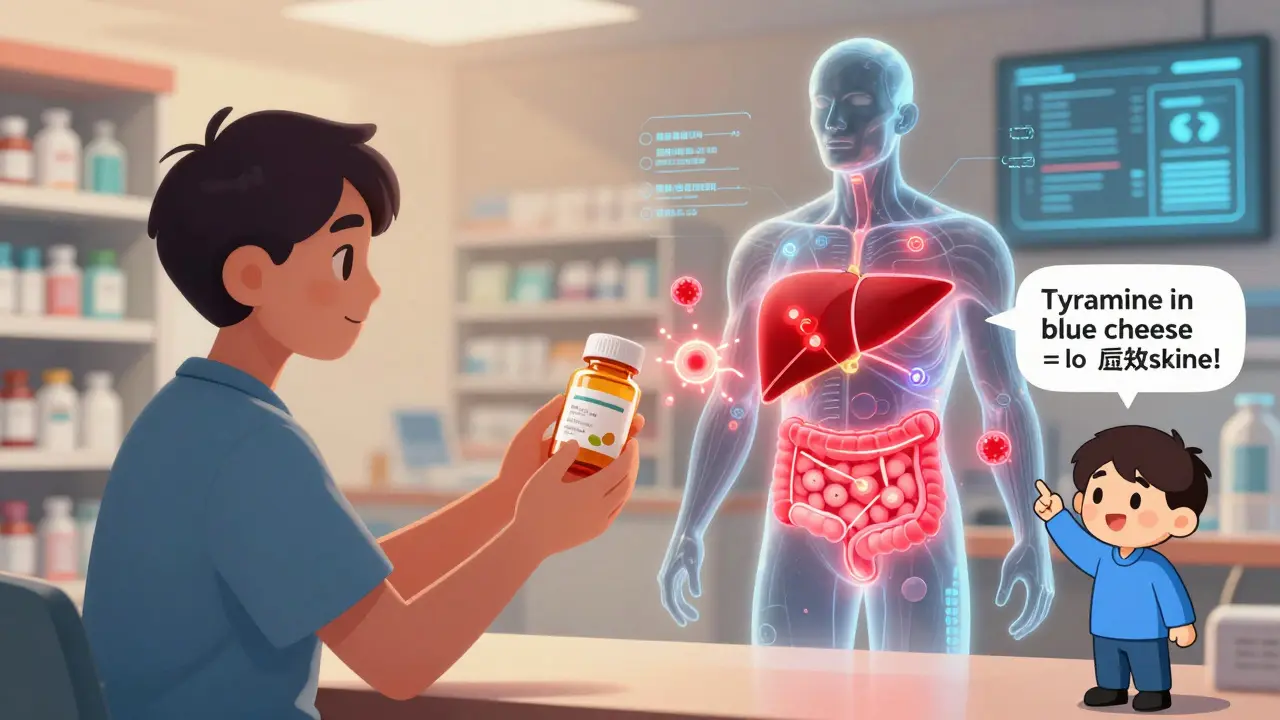
What Happens When We Don’t Understand the Mechanism
Some drugs work - but no one fully knows why. Dimebon, a Russian antihistamine, looked promising for Alzheimer’s in small early trials. But when tested in larger studies, it failed. Why? Because its mechanism was unclear. You can’t predict side effects or optimize doses if you don’t know how the drug interacts with your body. That’s why the FDA now requires detailed mechanism-of-action data for nearly all new drugs. In 2015, only 62% of applications included this. By 2023, it was 87%. The thalidomide tragedy in the 1960s is a chilling example. One form of the molecule helped with morning sickness. The other caused severe birth defects. At the time, scientists didn’t realize the body could turn one into the other. Today, we test for these differences. We know enantiomers matter.What You Can Do to Stay Safe
You don’t need a medical degree to use medicine safely. But you do need to ask the right questions:- What is this medicine supposed to do? Is it blocking a receptor? Stopping an enzyme? Increasing a chemical?
- What should I avoid? Foods? Other meds? Alcohol? (Ask about protein binding, vitamin K, tyramine, or liver metabolism.)
- What side effects mean something’s wrong? Muscle pain on statins? That’s not normal fatigue - it could be rhabdomyolysis. Dizziness on blood pressure meds? Maybe your dose is too high.
- Do I need blood tests? Lithium, warfarin, some antiseizure drugs - they all need monitoring.
The Future: Personalized Safety
By 2028, we may have “digital twins” - computer models of your body that simulate how a drug will affect you. They’ll use your genetics, liver enzymes, and even gut bacteria to predict reactions. Right now, the NIH’s All of Us program is studying 1 million people to find out why 28% of bad reactions are tied to genetic differences. One day, your doctor might say, “Your genes mean you process this drug slowly. We’ll start with half the dose.” Until then, the best tool you have is understanding. Not just knowing what to take - but why.Can I stop taking my medicine if I feel better?
It depends on the drug. Antibiotics must be finished even if you feel fine - stopping early lets resistant bacteria survive. Blood pressure or cholesterol meds work continuously; stopping them causes levels to rebound. Antidepressants like SSRIs can cause withdrawal if stopped suddenly because your brain has adjusted to higher serotonin levels. Always talk to your doctor before stopping - never guess.
Why do some medicines cause side effects I didn’t expect?
Because most drugs don’t act on just one target. Aspirin reduces pain by blocking COX-1, but COX-1 also protects your stomach lining - so stomach upset is a common side effect. Statins lower cholesterol by blocking HMG-CoA reductase, but that same enzyme is involved in muscle cell function - which is why muscle pain can happen. Side effects aren’t mistakes; they’re unintended consequences of how the drug works.
Are natural supplements safer than prescription drugs?
Not necessarily. St. John’s Wort, for example, can reduce the effectiveness of birth control pills, blood thinners, and even some antidepressants. It works by activating liver enzymes that break down other drugs - similar to how grapefruit juice affects statins. Just because something is “natural” doesn’t mean it’s safe to mix with prescription meds. Always tell your doctor what supplements you’re taking.
How do I know if my medication dose is right?
For some drugs, like warfarin or lithium, blood tests tell you exactly. For others, like blood pressure or antidepressants, your symptoms and how you feel over time are the best guide. If you’re still having symptoms or having side effects, your dose may need adjusting. Don’t assume the first dose is perfect - many medications require fine-tuning over weeks.
Why do some drugs need to be taken with food and others on an empty stomach?
Food can change how fast or how much of a drug enters your bloodstream. Some drugs, like certain antibiotics, are absorbed better on an empty stomach - food blocks them. Others, like statins or NSAIDs, are easier on your stomach if taken with food. The instructions aren’t arbitrary. They’re based on how the drug behaves chemically with digestion.
Can I drink alcohol while taking medicine?
It’s risky. Alcohol can increase drowsiness with sedatives, raise blood pressure with some antidepressants, and overload your liver when combined with painkillers like acetaminophen. Even a single drink can be dangerous with certain drugs. If you’re unsure, assume it’s unsafe - and ask your pharmacist.





This is actually one of the clearest explainers I’ve read on how meds work. I used to think pills were just little magic bullets, but now I get why my doc keeps asking if I eat spinach. 🙌
So you're telling me that if I don't understand the molecular mechanism of my antidepressant, I'm basically playing Russian roulette with my brain? That's terrifying. And also, why does no one ever explain this to patients before they sign the consent form? It's like handing someone a chainsaw and saying 'be careful.'
Wow. Another feel-good article that ignores the fact that 80% of people can't even spell 'pharmacokinetics' let alone understand it. This is why so many people stop their meds. You think telling them about COX-1 enzymes is going to make them compliant? Please. They just want the headache to go away.
Very good. I like how you explain with simple words. In Nigeria, many people think medicine is from spirit. Now they can see it is science. Thank you.
Let’s be real - we’re all just lab rats in a giant pharmaceutical simulation. The body is a black box, and drugs are just noisy signals we throw into it hoping something sticks. The fact that we’ve survived this long without fully understanding how ibuprofen works is either a miracle or a sign we’re all just incredibly lucky. Or both. Either way, I’m not taking another pill until I know which protein it’s flirting with.
Oh wow. A 2023 FDA report says 32% of adverse events come from patients not understanding their meds? Shocking. Next you’ll tell me people don’t read the ‘do not operate heavy machinery’ warning on their Tylenol. Maybe we should just print the entire pharmacology textbook on the pill bottle. Or better yet - hire a TikTok influencer to explain it with dance moves.
So basically, if I take two pills and one makes me sleepy and the other makes me alert, I’m just playing molecular tug-of-war with my liver? Cool. I’ll just keep doing that.
Actually, this is why I started asking my pharmacist for analogies. ‘SSRIs are like putting a cork in the serotonin recycling tube’ - that made more sense than any medical pamphlet. Also, I now know not to eat blue cheese with my MAO inhibitor. Thanks, Reddit.
Thank you for writing this. I’ve been on lithium for 7 years and no one ever explained why I need monthly blood tests - I thought it was just bureaucracy. Now I get it: it’s not about checking if I’m ‘compliant,’ it’s about staying alive. I’m sharing this with my support group. 💙
Great breakdown. I’m a nurse in Mumbai and I use this kind of explanation every day. Patients remember ‘key in lock’ better than ‘receptor agonism.’ Also, always ask about supplements - St. John’s Wort is everywhere here, and no one realizes it’s a silent drug killer.
The first-pass effect is just the liver’s way of saying ‘not today, buddy.’ Propranolol gets 90% chewed up? That’s not pharmacology, that’s a digestive power move. Also, ‘digital twins’? Sounds like sci-fi marketing. We still don’t know why aspirin works for some and gives others migraines. We’re still flying blind.
In India, we call this ‘dawa ka kaam’ - how the medicine works. My grandma always said, ‘If it’s too strong, it’ll burn you. If it’s too weak, it won’t help.’ She didn’t know about receptors, but she knew the truth. Simple, but true.
Wow. So the future is… computer models of your body? Cool. So instead of trusting doctors, we’ll trust a machine that doesn’t even know what a bad day feels like. And I’m supposed to be okay with that? Meanwhile, my actual doctor just prescribed me 3 new meds because I ‘didn’t respond’ to the first 2. Guess what? I’m just a data point now.
As someone who’s been on 5 different antidepressants, I can confirm: knowing the mechanism doesn’t make side effects go away, but it makes you feel less crazy when you’re crying in the shower because your brain suddenly hates serotonin. Also, yes, I still avoid aged cheese. No regrets.