 29
Apr,2023
29
Apr,2023
Understanding the Connection Between Shingles and Your Liver
As a blogger who is passionate about health and wellness, today, I want to talk about an important topic that affects many people – shingles and its potential impact on your liver. Shingles is a painful skin rash caused by the varicella-zoster virus, the same virus that causes chickenpox. When the virus becomes reactivated later in life, it can result in shingles. While most people are aware of the painful rash and other symptoms associated with shingles, not everyone is aware that it can also affect your liver. In this article, we will discuss the connection between shingles and liver health, and what you need to know to protect yourself and your loved ones.
How Shingles Can Affect Your Liver
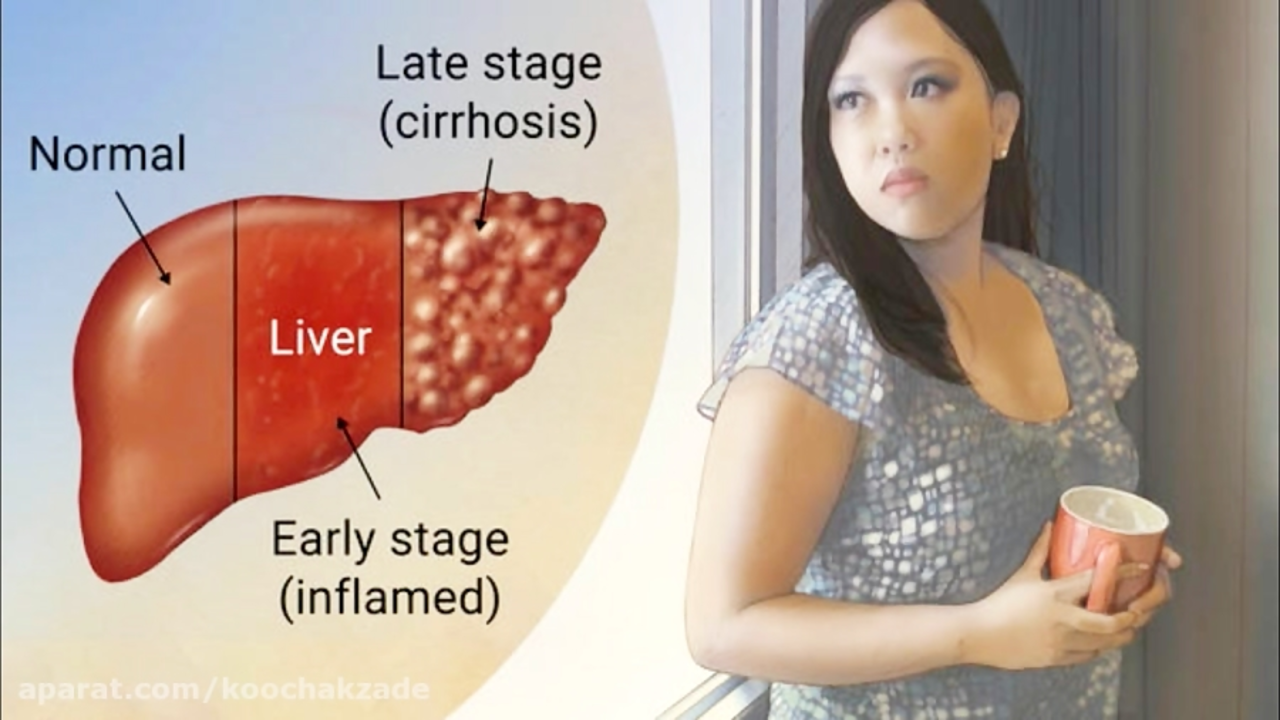
First, let's examine how shingles can affect your liver. Although it's not common, the varicella-zoster virus can cause inflammation in various internal organs, including the liver. This condition is known as visceral disseminated varicella-zoster virus infection. When the liver is affected, it can result in hepatitis, which is an inflammation of the liver. Hepatitis can cause damage to liver cells, and in severe cases, lead to liver failure. Although this is rare, it's essential to be aware of the potential risks and take steps to protect your liver if you have shingles.
Recognizing the Symptoms of Shingles-Related Liver Problems
Now that we know shingles can potentially affect your liver, it's crucial to recognize the symptoms of shingles-related liver problems. These can include:
- Jaundice (yellowing of the skin and eyes)
- Dark urine
- Light-colored stools
- Abdominal pain
- Nausea and vomiting
- Fatigue
- Loss of appetite
- Itching
If you have shingles and start to experience any of these symptoms, it's essential to contact your healthcare provider immediately. Early diagnosis and treatment can help prevent severe liver damage and other complications.
Preventing Shingles and Protecting Your Liver
Fortunately, there are steps you can take to prevent shingles and protect your liver. One of the most effective ways to prevent shingles is by receiving the shingles vaccine. The vaccine can significantly reduce your risk of developing shingles and its complications, including liver problems. It's generally recommended for adults aged 50 and older, as the risk of shingles increases with age. If you're unsure whether you should get the vaccine, talk to your healthcare provider.
In addition to getting vaccinated, it's crucial to maintain a healthy lifestyle to keep your liver in good shape. This includes:
- Eating a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats
- Exercising regularly
- Maintaining a healthy weight
- Limiting alcohol intake
- Avoiding risky behaviors that can expose you to hepatitis viruses, such as sharing needles or having unprotected sex
By taking steps to prevent shingles and protect your liver, you can reduce your risk of developing liver problems and maintain overall good health.
Managing Shingles and Liver Health If You're Already Affected
If you've already been diagnosed with shingles and are concerned about your liver health, it's essential to work closely with your healthcare provider to manage your condition. They can recommend appropriate antiviral medications to treat the shingles, as well as monitor your liver function through blood tests. If liver problems are detected, your healthcare provider may recommend additional treatment, such as medications to reduce inflammation or manage specific symptoms.
It's also crucial to maintain a healthy lifestyle, as mentioned earlier, to support your liver health. In addition, managing stress and getting plenty of rest can help your immune system fight off the virus and reduce the risk of complications.
In conclusion, while shingles can potentially affect your liver, there are steps you can take to prevent the virus and protect your liver health. By being aware of the risks and taking action to maintain your overall well-being, you can reduce the likelihood of experiencing shingles-related liver problems.





Hey folks, let’s dive into this shiny connection between shingles and liver health with a burst of energy! 🌟 The varicella‑zoster virus can occasionally wander beyond the skin and stir up inflammation in the liver – a rare but real scenario. Staying ahead means getting the shingles vaccine, especially after the big five‑oh, because prevention is the most vibrant shield you can wield. Pair that with a diet rich in leafy greens, berries, and lean proteins, and your liver will thank you with a steady rhythm. Keep active, manage stress, and remember: a healthy liver is the backstage crew keeping your body’s show running smoothly.
Super proud of you for taking the vaccine step! 🙌 Your liver will love the extra love you’re giving it.
It’s fascinating how a virus primarily known for a painful rash can, in exceptional cases, tip its hat toward hepatic involvement. While the incidence of shingles‑related hepatitis remains low, the clinical signs-jaundice, dark urine, and fatigue-should never be dismissed lightly. Prompt antiviral therapy, coupled with routine liver function monitoring, forms a solid safety net. Moreover, embracing a balanced diet rich in antioxidants can bolster hepatic resilience against inflammatory insults. Staying informed and proactive turns a potential scare into a manageable health journey.
Skipping the vaccine is simply irresponsible when it endangers both skin and liver.
Looks like most people don’t realize the liver risk until symptoms appear. It’s a good reminder to keep up with check‑ups and vaccines. Stay healthy.
One might contemplate the delicate equilibrium of the human organism, wherein an external pathogen such as varicella‑zoster can perturb the hepatic milieu. This perturbation, albeit infrequent, underscores the interdependence of cutaneous and visceral health. It is prudent, therefore, to adopt preventative measures that reinforce systemic homeostasis, exemplified by immunization and judicious lifestyle choices. In this manner, the preservation of hepatic integrity becomes not merely a medical concern but a philosophical commitment to bodily harmony.
Our nation will not be held back by foreign viruses; we must demand universal shingles vaccination and protect our liver health with the same vigor we defend our borders.
Esteemed readers, consider the ancient wisdom that health is the sum of harmonious functions; when the varicella‑zoster virus insinuates itself within hepatic tissue, it disrupts this harmony. It is incumbent upon us, as custodians of our bodies and cultural heritage, to employ prophylactic strategies-chief among them vaccination-to preserve this delicate balance. Moreover, the integration of dietary principles rooted in our diverse cultures can further fortify hepatic resilience. Let us, therefore, approach this challenge with both scientific rigor and the reverence afforded to the traditions that have sustained us.
Oh sure, because who doesn’t love a rash that moonlights as a liver saboteur? In all seriousness, the shingles shot is your ticket to keeping both skin and liver out of the drama department. Toss in some veggies, a decent night’s sleep, and you’ve got a recipe for a body that won’t be starring in any unwanted sequels.
Yeah, because ignoring a vaccine is the fastest way to turn your liver into a drama queen. Let’s keep the drama on Netflix, not in our bodies.
People keep saying shingles only hits the skin but they forget how the virus can sneak into the liver and cause trouble 😑 the pharma doesn’t want you to know about the hidden risks they’re pushing the vaccine like it’s a miracle cure while hiding side effects you never hear about 😤 keep reading the fine print folks
Honestly, the discourse around shingles and hepatic implications is often plagued by layman simplifications. One must definately consider the virological nuance before jumping to conclusions. Vaccination, while beneficial, should be evaluated in the context of individual immunological profiles. Receiving the shot without proper counsel is a faux pas in modern preventative medicine.
Look, I’m not here to chant patriotic slogans but it’s absurd how some people dismiss the shingles vaccine as a government ploy. The truth is, protecting your liver isn’t a political statement-it’s basic self‑care. If you’re tired of the same old scare tactics, just do what makes sense for your health.
Hey, I noticed you haven’t mentioned your diet yet-what are you actually eating? 🍽️ If you’re loading up on processed junk, your liver is begging for help, especially when shingles shows up. Drop the soda, add some greens, and let’s get that organ humming again! 🔥
First and foremost, let’s acknowledge that shingles, while commonly relegated to a dermatological nuisance, possesses a latent capacity to affect visceral organs, the liver being a prime example; this fact, though not headline news, deserves our undivided attention. The pathophysiology hinges on the reactivation of varicella‑zoster virus, which, in rare instances, disseminates systemically, prompting hepatic inflammation that mirrors viral hepatitis both clinically and biochemically. Consequently, clinicians should maintain a high index of suspicion when a patient presents with the classic dermatomal rash accompanied by unexplained jaundice, dark urine, or malaise. Laboratory evaluation, including liver function tests and viral PCR, becomes indispensable in delineating the extent of involvement. Early initiation of antiviral therapy, such as acyclovir or valacyclovir, can mitigate hepatic injury, yet it is not a panacea; supportive care, adequate hydration, and nutritional optimization remain cornerstones of management. Speaking of nutrition, a diet replete with antioxidant‑rich fruits, cruciferous vegetables, and lean proteins serves to bolster hepatic resilience, while excessive alcohol consumption unequivocally exacerbates the risk of decompensation. Moreover, lifestyle modifications-regular exercise, stress reduction techniques, and sufficient sleep-collectively contribute to a robust immune response capable of subduing viral resurgence. It is also paramount to recognize that vaccination stands as the most effective prophylactic measure, dramatically curbing the incidence of shingles and, by extension, its hepatic sequelae; the recombinant zoster vaccine, with its superior efficacy, is especially recommended for adults over fifty. In populations with pre‑existing liver disease, the stakes are even higher, necessitating vigilant monitoring and perhaps an adjusted therapeutic regimen. Furthermore, interdisciplinary collaboration among dermatologists, hepatologists, and primary care providers ensures a comprehensive approach, fostering early detection and coordinated treatment. Public health initiatives should therefore emphasize educational campaigns that highlight the less obvious complications of shingles, thus dispelling the myth that it is merely a skin issue. Lastly, patients must be empowered to report any atypical symptoms promptly, as timely intervention can be the difference between transient discomfort and permanent hepatic compromise. In summary, while shingles‑related liver involvement remains uncommon, its potential severity mandates a proactive stance encompassing vaccination, early diagnosis, and holistic care. By intertwining medical vigilance with lifestyle stewardship, we can safeguard both the skin and the liver from this stealthy adversary.