 25
Dec,2025
25
Dec,2025
Most people think of hepatitis as a long-term liver problem-something that sticks around for years. But hepatitis A is different. It doesn’t hang around. It hits hard, makes you feel awful for weeks, and then, almost always, it’s gone for good. No lifelong treatment. No chronic liver damage. Just a tough, sometimes scary, but usually temporary illness.
How Hepatitis A Spreads
You don’t need to share needles or have unprotected sex to catch hepatitis A. The virus spreads through something you might not even think about: poop. Not the kind you see, but the kind you don’t. Tiny particles from an infected person’s stool get onto hands, food, water, or surfaces-and then into your mouth.
This happens in real life more than you’d expect. A food worker with hepatitis A doesn’t wash their hands after using the bathroom, then handles a salad. You eat it. You get sick. Or you travel to a place with poor sanitation, drink bottled water that wasn’t properly treated, and end up with a stomach bug that won’t go away. In fact, the CDC found 17 foodborne outbreaks in 2022 linked to contaminated produce handled by infected workers.
The virus is tough. It can survive on surfaces for up to 30 days. It doesn’t care if the water looks clean. It doesn’t care if the restaurant has a good rating. It just needs one person who’s shedding the virus-and one person who touches something contaminated and then eats without washing their hands.
What Happens When You Get Infected
After you swallow the virus, it takes time to show up. On average, 28 days. But it could be as short as 15 days or as long as 50. During this time, you feel fine. You’re not contagious yet.
Then, suddenly, you don’t. You feel tired-like you’ve run a marathon for a week. You lose your appetite. Your stomach feels off. Maybe you get a low fever, or you start throwing up. Your pee turns dark, like cola. Your stools turn pale, almost clay-colored. Then, the yellowing starts. Your skin, your eyes-everything turns yellow. That’s jaundice. It’s the liver screaming that it’s overwhelmed.
Here’s the thing: kids under six often don’t show any of this. They might have a stomach bug and bounce back. Adults? 70-80% get jaundice. The older you are, the worse it gets. People over 50 are at higher risk for serious complications, including rare but dangerous liver failure.
How Long Does It Last?
Most people think, “I had jaundice, so I’m done.” Not quite.
Jaundice usually peaks within a week and fades over the next few weeks. But fatigue? That sticks around. A survey from the Hepatitis Foundation International found that 82% of adults reported extreme tiredness lasting an average of 6.2 weeks. Some people feel okay after a month. Others are dragging for three or four months.
And here’s the surprise: 10-15% of adults, especially those over 50, have relapses. You think you’re getting better. You go back to work. You start cooking again. Then, out of nowhere, you’re tired again. Your stomach feels off. Your eyes look yellow again. This isn’t the virus coming back-it’s your liver still healing. Each relapse lasts about a week to two weeks.
Lab tests tell the real story. Liver enzymes (ALT and AST) spike during infection. For 80% of people, they return to normal within 12 weeks. For 95%, it’s six months. That’s when your liver is truly back to normal.

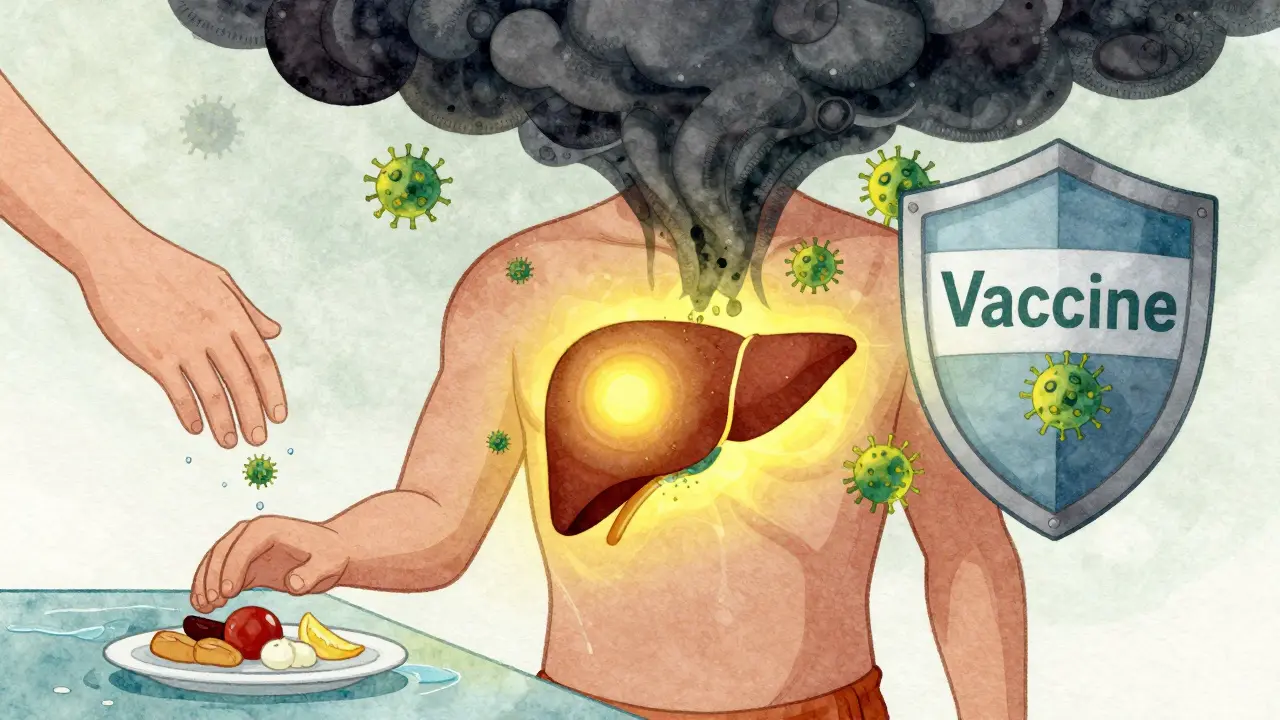
How to Prevent It
There’s one simple, powerful way to avoid hepatitis A: the vaccine.
The hepatitis A vaccine is two shots, given 6 to 18 months apart. After the first shot, you’re 95% protected within four weeks. After the second? Nearly 100%. Since it became routine in the U.S. in 1995, cases have dropped by 95%. That’s not a guess. That’s CDC data.
The CDC recommends the vaccine for all children at age 1. But it’s not just for kids. If you’re traveling overseas, work in healthcare, use drugs, are homeless, or have chronic liver disease-you need it. Even if you’re just planning a trip to Mexico or Thailand, get vaccinated at least four weeks before you leave.
What if you were exposed? Say you ate at a restaurant where someone got sick, or you had close contact with someone who tested positive? You still have a window. If you get the vaccine or a shot of immune globulin within two weeks of exposure, you’re 85-90% protected from getting sick.
Handwashing helps too. Soap and water, scrubbed for 20 seconds-especially after using the bathroom or before eating-can cut transmission by 30-50%. Bleach solutions (5-10 tablespoons per gallon of water) kill the virus on surfaces in two minutes. Don’t use alcohol wipes. They won’t work.
What to Do If You’re Infected
There’s no cure. No antiviral pills. No special diet that speeds recovery. Treatment is about support.
Rest. Drink water. Eat small, low-fat meals. Avoid alcohol completely until your liver enzymes return to normal-that could take months. Don’t take acetaminophen (Tylenol) over 2,000 mg a day. Your liver is already stressed. Don’t add to it.
Most people don’t need hospitalization. Only 10-20% do, usually because they’re dehydrated from vomiting. Outpatient care is enough for 75% of cases.
When can you go back to work or school? The rule is: wait one week after jaundice appears, or until your symptoms are gone and your doctor confirms you’re no longer contagious. Don’t rush it. You’re still shedding the virus in your stool for up to a week after jaundice starts.

Why It’s Not Like Hepatitis B or C
Hepatitis A doesn’t become chronic. You don’t carry it forever. You don’t pass it to your kids through breastfeeding. You don’t need lifelong monitoring. Once your body clears it, you’re immune for life. That’s why the vaccine works so well-it mimics the natural immunity you’d get from infection, without the sickness.
That’s also why it’s so frustrating when people confuse it with hepatitis B or C. Those can lead to cirrhosis, liver cancer, and require drugs for years. Hepatitis A? It’s a storm. It comes, it breaks, and then it’s over.
Who’s at Risk Today?
It’s not just travelers anymore. From 2016 to 2019, cases in the U.S. jumped 350% because of outbreaks among people experiencing homelessness and those who use injection drugs. These groups had low vaccination rates, and crowded living conditions made transmission easy.
But since 2020, targeted vaccination programs in these communities have cut cases by 40%. That’s proof that public health works. Vaccines, outreach, clean handwashing stations-these things save lives.
Still, outbreaks happen. Contaminated food. Poor hygiene in restaurants. Travelers bringing it back. The virus doesn’t take a break. That’s why prevention isn’t optional.
Recovery Is Possible
One man in Melbourne, 58, got hepatitis A after eating raw oysters on vacation. He was hospitalized for dehydration. He lost 15 pounds. He couldn’t work for two months. His wife had to take over cooking, cleaning, everything.
He didn’t die. He didn’t need a transplant. He didn’t become a carrier. He just got sick, rested, drank fluids, and waited. Six months later, his liver enzymes were normal. He’s back to hiking, cooking, and traveling.
That’s the story for most people. Hepatitis A is scary. It’s exhausting. It messes with your life. But it doesn’t define you. It doesn’t ruin your liver. It doesn’t last forever.
And the best part? You can stop it before it starts.
Can you get hepatitis A more than once?
No. Once you recover from hepatitis A, your body develops lifelong immunity. You can’t get infected again. That’s why the vaccine works so well-it trains your immune system to recognize the virus without you ever getting sick.
Is the hepatitis A vaccine safe?
Yes. A CDC study of 45,000 vaccinated children found 99.8% had no serious side effects. The most common reaction is mild soreness at the injection site, lasting less than two days. Serious allergic reactions are extremely rare.
Can you spread hepatitis A without symptoms?
Yes. People are most contagious two weeks before symptoms appear-often before they even know they’re sick. Children under six often show no symptoms at all but can still spread the virus. That’s why handwashing and vaccination are so important, even if no one around you seems sick.
How long should you avoid alcohol after hepatitis A?
Until your liver enzymes return to normal, which takes about 3 to 6 months for most people. Alcohol puts extra stress on your liver while it’s healing. Even small amounts can delay recovery. Doctors recommend complete avoidance during this time.
Does hepatitis A cause permanent liver damage?
No, not in healthy people. Hepatitis A causes acute inflammation, but the liver repairs itself completely. In rare cases-mostly in adults over 50 or those with existing liver disease-acute liver failure can occur, but this is uncommon. Most people recover fully without any lasting effects.
Should I get tested if I think I was exposed?
If you’ve been exposed within the last two weeks and haven’t been vaccinated, get the vaccine or immune globulin right away. Testing isn’t usually needed unless you’re developing symptoms. Blood tests can confirm infection, but treatment is supportive either way. Prevention is faster and more effective than waiting for symptoms.
Can hepatitis A be spread through kissing or casual contact?
It’s very unlikely. The virus spreads through fecal-oral contact, not saliva. You can’t catch it from a kiss, hug, or sharing a drink. But if someone has poor hand hygiene after using the bathroom and then touches your food or your face, that’s how it spreads. Handwashing is the key defense.
Is hepatitis A common in Australia?
No, it’s rare. Australia has high sanitation standards and strong vaccination coverage. Most cases are linked to international travel or outbreaks among vulnerable populations. But the risk isn’t zero-especially if you’re traveling to areas with poor sanitation. Vaccination is still recommended for travelers.






I got hepatitis A in Goa last year after eating street chaat. Thought it was just food poisoning until my eyes turned yellow. Took me 10 weeks to feel normal again. No meds, just rest, coconut water, and my grandma’s turmeric tea. The fatigue? Real. But I’m fine now. Vaccinated my whole family after.
OMG THIS IS A LIE!! I GOT HEP A AND IT CHANGED MY LIFE FOREVER!! I’M STILL YELLOW!! MY LIVER IS A DEAD FISH!! WHY IS EVERYONE LYING ABOUT THIS?? I’M ON YOUTUBE NOW AND THEY SAY YOU CAN’T RECOVER!! MY HUSBAND LEFT ME BECAUSE I ‘SMELLED LIKE JUICE’!!
For context: hepatitis A incidence in the U.S. dropped from 3.4 cases per 100,000 in 1995 to 0.3 in 2022. That’s not just vaccination-it’s sanitation infrastructure, public health education, and targeted outreach. The outbreaks among unhoused populations were a failure of systemic support, not individual behavior. The vaccine works. The system needs to catch up.
There’s something quietly beautiful about how the body heals itself when given space. No magic pill, no grand intervention-just rest, hydration, and time. The liver doesn’t need to be fixed. It needs to be trusted. And yet, our culture screams for quick fixes, for pills, for ‘hacks.’ Hepatitis A doesn’t care about hustle culture. It asks only for stillness. Maybe that’s the real lesson here-not how to prevent disease, but how to surrender to healing.
For anyone recovering: you’re not lazy. You’re not broken. You’re rebuilding. One quiet day at a time.
Vaccine works. Wash hands. Don’t be an idiot. Done.
Let me tell you about my cousin’s friend’s neighbor who got hepatitis A after a sushi date in Portland. He was fine until day 23 when he woke up and his urine looked like motor oil. He thought he was dying. He called 911. The ER doc said, ‘You’re not dying, you’re just livering.’ He spent six weeks in bed. His dog started sleeping on his chest because he smelled like a damp towel. He didn’t work for three months. His plants died. His Netflix queue grew to 147 items. He says the worst part wasn’t the jaundice-it was the silence. No one understood why he couldn’t just ‘snap out of it.’ But here’s the thing-he didn’t snap out of it. He healed. Slowly. Like moss on a rock. And now he’s back, making vegan curry and telling everyone to get the vaccine. It’s not dramatic. It’s just… life.
I really appreciate how clearly this post breaks down the timeline-especially the part about relapses being part of healing, not reinfection. So many people think if symptoms come back, they’ve been reinfected or the vaccine failed. That’s not true. The liver is still recovering. Also, the point about bleach being the only surface disinfectant that works? Crucial. Alcohol wipes are useless against this virus-I learned that the hard way after disinfecting my kitchen with hand sanitizer and still getting sick.
And thank you for mentioning the 10-15% relapse rate. That’s the detail no one talks about. If you’re feeling better but still tired, it’s okay. You’re not failing. You’re just healing.
Of course the CDC says the vaccine is 95% effective after one dose. They also said the 2020 pandemic was ‘not a big deal’ and we’d all be back to brunch by June. But hey, at least the vaccine works. Unlike my last Uber driver who said he ‘got the shot but didn’t need it’ and then gave me hepatitis A via a handshake after using the bathroom. Just saying.