 11
Jan,2026
11
Jan,2026
When your kidneys stop working, your body can’t clean your blood. Waste builds up. Fluid swells your legs and lungs. Your bones weaken. Your heart struggles. This isn’t just aging-it’s end-stage renal disease (ESRD), the point where kidneys have lost 90% of their function. At this stage, you can’t survive without treatment. The choices are dialysis, transplant, or death. But beyond survival, there’s another question: which option lets you live the best life?
What Exactly Is End-Stage Renal Disease?
ESRD isn’t a sudden event. It’s the final step in a slow decline. Most people don’t feel sick until their kidneys are nearly gone. By the time doctors diagnose it, the damage is permanent. The official sign? A glomerular filtration rate (GFR) below 15. That means your kidneys are filtering less than 15 milliliters of blood per minute. Healthy kidneys do 90-120.The top two causes? Diabetes and high blood pressure. Together, they cause more than 70% of ESRD cases. Other causes include polycystic kidney disease, autoimmune disorders like lupus, and long-term drug or toxin exposure. In the U.S., about 786,000 people live with ESRD. Nearly 560,000 are on dialysis. Around 226,000 have a working kidney transplant.
Dialysis: Keeping You Alive, But at What Cost?
Dialysis does the job your kidneys can’t. It pulls out waste and extra fluid from your blood. There are two main types: hemodialysis and peritoneal dialysis.Hemodialysis happens in a clinic, usually three times a week. Each session lasts 3 to 4 hours. You’re hooked to a machine that pulls your blood out, cleans it, and puts it back. Blood flows at 300-500 mL per minute. The dialysate fluid moves at 500-800 mL per minute. You need a fistula-a connection between an artery and vein in your arm-created 6 to 12 months before starting. This gives it time to strengthen.
Peritoneal dialysis happens at home. A fluid is pumped into your belly through a catheter. Your peritoneal membrane acts like a filter. After a few hours, the fluid is drained out. This can be done manually 4 times a day (CAPD) or overnight with a machine (APD). Weekly Kt/V (a measure of dialysis effectiveness) should be at least 1.7.
But dialysis isn’t free. It takes 12-16 hours a week of your time-just for treatment. Add travel, recovery, and side effects like cramps, low blood pressure, and exhaustion. You’re on a strict diet: low sodium, low potassium, low phosphorus. Fluid intake is limited. You can’t drink like you used to. Many patients feel like they’re living in a cage.
Kidney Transplant: The Best Chance at a Real Life
A kidney transplant isn’t a cure, but it’s the closest thing. It gives you back your body’s natural filtering system. And the data doesn’t lie: transplant recipients live longer, feel better, and spend less time in the hospital.Compared to dialysis, transplant reduces your risk of death by 68%. Five-year survival? 83% for transplant patients versus 35% for those on dialysis. Hospital visits drop by half. You can eat more foods. Drink more water. Travel without planning around sessions. Many return to work, sports, and family life.
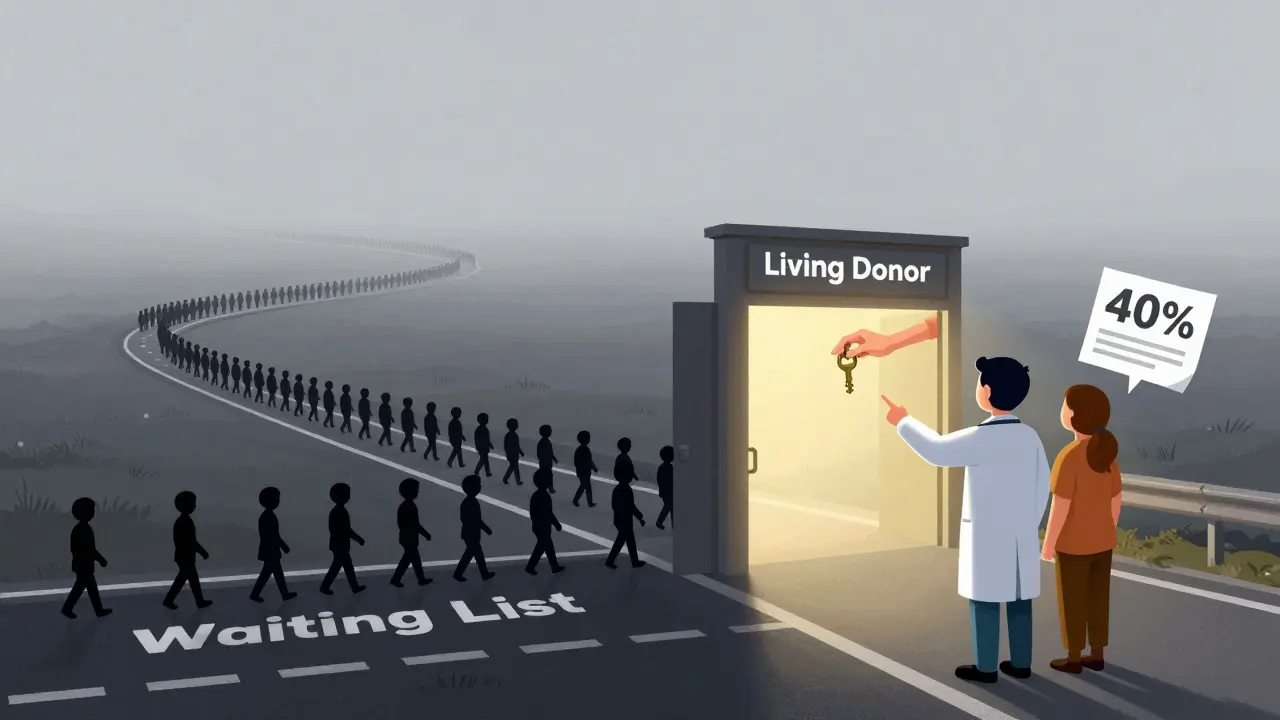
There are two sources for donor kidneys: living and deceased. Living donor transplants have better outcomes. One-year graft survival? 95.5%. Five-year? 86%. Deceased donor kidneys are still good-93.7% survive one year, 78.5% survive five. But you’ll wait. In 2023, over 90,000 people were on the waiting list. Only 27,000 transplants happened that year. The average wait? Four years.
Preemptive transplants-getting a kidney before starting dialysis-give the best results. Only 5% of people who start dialysis are referred early enough. Doctors recommend seeing a transplant center when your GFR drops below 30. That gives you time to get tested, find a donor, and get on the list.

Quality of Life: Numbers Don’t Tell the Whole Story
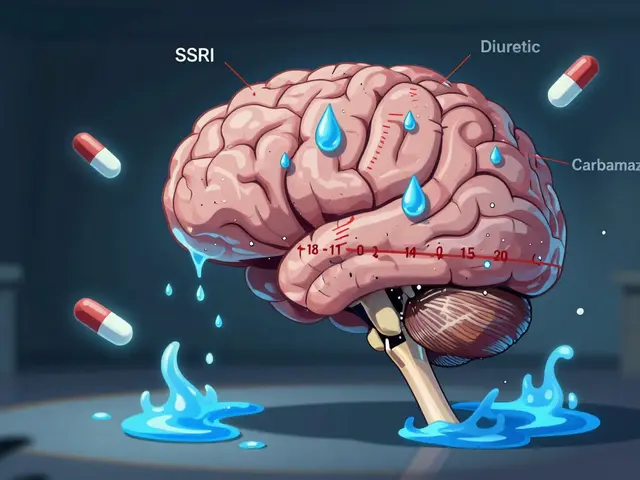
A 2021 study in the Clinical Journal of the American Society of Nephrology used the KDQOL-36 survey to measure quality of life. Dialysis patients scored 53.7 out of 100. Peritoneal dialysis patients scored 67.2. Transplant patients? 82.4. That’s a 28.7-point jump. That’s not just a number. That’s being able to sleep through the night. That’s taking your kid to school without feeling dizzy. That’s eating a banana without checking your potassium levels.Transplant recipients don’t need to be tied to a machine. They don’t need to plan vacations around dialysis centers. They can eat out. Travel. Work full-time. They still take daily pills-immunosuppressants like tacrolimus, mycophenolate, and steroids-but those are a small price compared to the freedom.
But it’s not perfect. You’re at higher risk for infections. Some medications cause tremors, weight gain, or high blood pressure. You need regular blood tests. You can’t skip appointments. But compared to dialysis? It’s a trade-off that most people say is worth it.
Who Can Get a Transplant?
Not everyone qualifies. Age alone doesn’t disqualify you, but if you’re over 75 with heart disease, dementia, or uncontrolled cancer, you’re unlikely to be approved. Active drug or alcohol use? You need to be clean for at least 6 months. Severe heart failure (ejection fraction under 25%)? You’ll need to stabilize first.And here’s the hard truth: access isn’t equal. African American patients are less likely to be referred for transplant evaluation-even when they have the same medical needs. The RaDIANT Community Study found that after education programs for doctors and patients, transplant referrals for Black patients jumped 40%. That’s progress, but the gap still exists.
Medicare covers ESRD treatment, but only after 3 months of dialysis. If you get a transplant, coverage lasts 36 months. After that, you need other insurance. Many patients lose coverage because they can’t afford private plans. That’s why early planning matters.
What’s Changing in 2026?
The system is slowly improving. The Kidney Care Choices Model, launched in 2022, pays providers to refer patients to transplant centers earlier. More centers are pushing for living donor programs. The 21st Century Cures Act helped expand the donor pool by allowing organs from older or higher-risk donors. Living donor transplants have risen 18% since 2018.The NIH has invested $157 million through 2026 for the Kidney Precision Medicine Project. This isn’t about one-size-fits-all treatment anymore. Researchers are studying how genetics, inflammation, and immune responses affect transplant success. The goal? Personalized immunosuppression-fewer side effects, better long-term outcomes.
But the waiting list keeps growing. 3,000 new people join every month. Only 27,000 transplants happen each year. That’s a 10-to-1 gap. Even with all the advances, most people will spend years waiting.
What Should You Do If You Have ESRD?
If you’re newly diagnosed:- See a nephrologist immediately. Don’t wait.
- Ask for a transplant evaluation when your GFR drops below 30. Don’t wait until you’re on dialysis.
- Get your family tested as potential living donors. A living donor kidney lasts longer and works better.
- Learn about home dialysis options. They give more control than in-center treatments.
- Join a patient support group. Talking to others who’ve been there helps more than you think.
If you’re already on dialysis:
- Ask your team: “Am I a candidate for transplant?”
- Don’t assume you’re too old, too sick, or too late. Many people get transplants in their 60s and 70s.
- Keep your blood pressure and sugar under control. These affect transplant success.
- Take your meds. Missed doses of phosphate binders or vitamin D can damage your bones and heart.
Final Thought: It’s Not Just About Living Longer. It’s About Living Better.
Dialysis keeps you alive. A transplant gives you your life back. The numbers prove it: better survival, fewer hospital stays, higher quality of life. But the real win? Waking up without thinking about your next treatment. Eating a meal without counting grams. Hugging your grandchild without feeling weak. That’s not medicine. That’s freedom.The system isn’t perfect. Wait times are long. Costs are high. Disparities still exist. But if you’re willing to fight for it-early referral, asking questions, pushing for evaluation-you can beat the odds. Your kidneys may be failing. But your life doesn’t have to be.
Can you live a normal life after a kidney transplant?
Yes. Most transplant recipients return to work, travel, exercise, and enjoy hobbies within 3 to 6 months. They don’t need dialysis sessions, have fewer dietary restrictions, and report higher energy levels. The trade-off is taking daily immunosuppressant pills and attending regular checkups to prevent rejection and infection.
How long do kidney transplants last?
Living donor kidneys last an average of 15 to 20 years. Deceased donor kidneys last 10 to 15 years. Some last 25+ years with good care. Graft survival rates are 95.5% at 1 year and 86% at 5 years for living donor transplants. Rejection, infection, or side effects from medications can shorten lifespan, but most people live longer with a transplant than on dialysis.
Why are so few people referred for transplants early?
Many doctors still treat ESRD as a dialysis-first problem. Patients aren’t always told about transplant options until they’re already on dialysis. There’s also a lack of awareness among patients and providers about living donor potential. Studies show that when clinics actively educate patients and remove barriers, transplant referrals increase by 40% or more.
Can you get a transplant without being on the waiting list?
Yes-if you have a living donor. A living donor transplant doesn’t require you to be on the national waiting list. You can be evaluated and scheduled as soon as the donor is cleared. This is called a preemptive transplant and is the fastest, most effective way to avoid dialysis entirely.
Is dialysis worse than a transplant?
Medically, yes. Dialysis has a 68% higher risk of death than transplant. Quality of life scores are 28 points lower. But dialysis is still life-saving. For those who can’t get a transplant due to health, age, or lack of access, it’s the best available option. The goal isn’t to make people feel guilty for choosing dialysis-it’s to make sure everyone has the chance to choose transplant.
What are the costs of kidney transplant vs. dialysis?
In the first year, a transplant costs more-around $100,000 for surgery and medications. But after that, annual costs drop to $15,000-$25,000 for immunosuppressants. Dialysis costs $90,000-$100,000 per year, every year. Over five years, transplant saves the system over $300,000 per patient. Medicare spends $35 billion annually on ESRD care, mostly on dialysis.
Can you donate a kidney if you’re over 60?
Yes. Many donors are in their 60s and even 70s. Donor health matters more than age. As long as you’re in good shape, have normal kidney function, and no major chronic diseases, you can be evaluated. Living donor transplants from older donors have excellent success rates and help reduce the waiting list.




Just read this whole thing and I’m crying. Not because it’s sad-because it’s true. I’ve seen my mom go through dialysis for five years. The exhaustion, the diet, the constant fear-it’s a slow erosion of dignity. But when she got her transplant? She started gardening again. Bought a motorcycle. Laughed like she used to. This isn’t just medicine. It’s a second chance at being human.
My uncle got a kidney from his sister last year. He’s 71. Still drives, still plays chess at the community center. People think transplants are for young people-but no. If you’re otherwise healthy, age shouldn’t be a barrier. The system needs to stop assuming older folks ‘don’t deserve it.’ They’ve earned the right to live well.
Let’s be clear: dialysis is a financial and logistical nightmare. The $90K/year cost is obscene when a transplant saves $300K over five years. Yet hospitals still push dialysis-first protocols because it’s profitable. This isn’t medical ethics-it’s capitalism exploiting the vulnerable. We need systemic reform, not just patient education. The KCCM model is a start, but it’s not enough.
Wait. So you’re telling me I could’ve avoided five years of hell if someone had just TOLD me about transplant options? My sister died waiting. She was too scared to ask. Too tired to fight. And now I’m supposed to be grateful for a ‘study’ that says ‘referrals increased 40%’? That’s not progress. That’s a funeral with a ribbon.
My cousin got a kidney from a stranger in India. No blood relation. Just someone who said yes. They did the whole process through a nonprofit. Took 8 months. No waiting list. I didn’t know this was possible. Why don’t more people know this? We need to spread the word. Not just in hospitals. In temples. In villages. In WhatsApp groups.
I work in a dialysis center. I see the same faces three times a week. Some don’t speak. Some cry silently. One woman brings her grandkids in to read to her during treatment. I don’t say much. But I listen. And I think-this isn’t just about kidneys. It’s about who gets to feel like they still belong in the world.
Hey-listen. If you’re reading this and you’re newly diagnosed? DO NOT WAIT. Go to a transplant center TODAY. Even if you think you’re too old, too sick, too anything-you’re not. I was 68. Had diabetes. Thought I was out of luck. Got a transplant in 11 months. Now I hike. I dance with my wife. I eat tacos. I cry sometimes-not from pain, but from joy. You can have this too. Just ask. Just push. Just don’t give up.
There’s a quiet violence in how we treat ESRD. We frame it as a medical problem, when it’s really a social one. Who gets referred? Who gets heard? Who gets to live? The numbers tell part of the story-but the silence around access, the lack of urgency, the way we normalize waiting years to live-that’s the real pathology. A transplant doesn’t just replace a kidney. It restores agency. And agency is the most underrated medicine of all.
My dad got his transplant last year. He’s 70. Still takes his pills. Still gets bloodwork. But now he sleeps through the night. And last weekend? He grilled burgers. No restrictions. No IVs. Just him. And the smoke. And the smell of charcoal. That’s what they don’t tell you. It’s not about surviving. It’s about remembering what it feels like to be alive.