 24
Sep,2025
24
Sep,2025
Cefaclor vs Alternatives Quiz
A 30‑year‑old pregnant woman presents with acute sinusitis. Which antibiotic is the most appropriate alternative to Cefaclor?
Cefaclor is a second‑generation oral beta‑lactam antibiotic sold under the brand name Ceclor CD. It fights susceptible bacteria by blocking cell‑wall synthesis, leading to bacterial death. Health professionals prescribe it for ear, sinus, throat and urinary‑tract infections, especially when a broad‑spectrum beta‑lactam is needed but penicillins are unsuitable.
How Cefaclor Works and When It’s Used
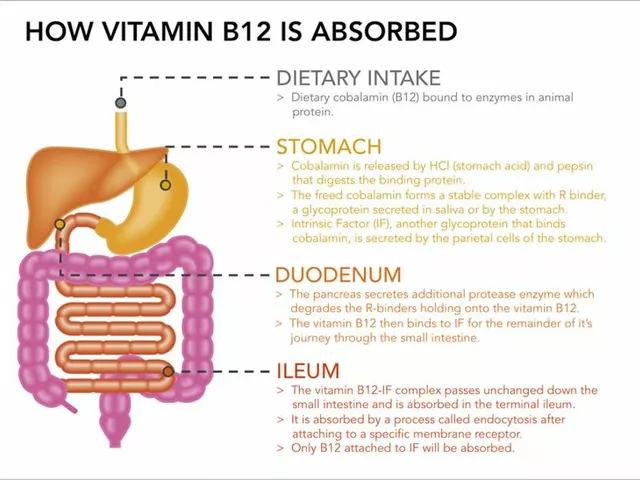
Like other beta‑lactams, Cefaclor targets the penicillin‑binding proteins (PBPs) that assemble the bacterial cell wall. By inhibiting these enzymes, the drug causes the wall to rupture, killing the organism. It is absorbed well orally (about 55‑70% bioavailability) and reaches peak plasma levels within 1-2hours. Because it isn’t metabolized by the liver, renal excretion accounts for most clearance, making dose adjustments important for patients with impaired kidney function.
Typical indications include acute otitis media, streptococcal pharyngitis, bacterial sinusitis, uncomplicated urinary‑tract infections (UTIs), and skin‑soft‑tissue infections caused by susceptible Gram‑positive and some Gram‑negative organisms.
Key Alternatives to Cefaclor
When clinicians consider a substitute, they look at spectrum, dosing convenience, safety in pregnancy, and resistance patterns. Below are the most common alternatives, each introduced with concise microdata.
Amoxicillin is a penicillin‑type broad‑spectrum antibiotic often first‑line for respiratory and ear infections. It works by the same cell‑wall inhibition mechanism but covers a slightly different bacterial range, especially Haemophilus influenzae.
Azithromycin is a macrolide antibiotic that blocks protein synthesis. Its long half‑life allows once‑daily dosing for 3‑5days, making it popular for patients who struggle with multiple daily pills.
Cefuroxime is a second‑generation cephalosporin similar to Cefaclor but with better activity against certain Gram‑negative bacteria and a higher oral bioavailability (≈85%).
Cefdinir is a third‑generation oral cephalosporin offering even broader Gram‑negative coverage, often chosen for community‑acquired pneumonia.
Penicillin V is a narrow‑spectrum penicillin primarily effective against streptococci and some pneumococci, but not useful against beta‑lactamase‑producing strains.
Clarithromycin is a macrolide with strong activity against atypical pathogens such as Mycoplasma and Chlamydia, often used when a patient has a penicillin allergy.
Doxycycline is a tetracycline antibiotic that inhibits protein synthesis. It’s especially useful for acne, Lyme disease, and certain resistant UTIs.
These alternatives collectively cover a spectrum that overlaps with, but also expands beyond, Cefaclor’s typical activity.
Side‑Effect Profile Compared
Understanding safety is a major driver for substitution. Below is a quick snapshot of the most frequent adverse events for each drug.
| Antibiotic | GI Disturbance | Allergic Reactions | Special Safety Notes |
|---|---|---|---|
| Cefaclor | Diarrhea (≈10‑15%) | Rash, rare anaphylaxis | Contraindicated in severe penicillin allergy |
| Amoxicillin | Diarrhea (≈12%) | Rash, higher cross‑reactivity with penicillins | Safe in pregnancy (Category B) |
| Azithromycin | Mild nausea (<5%) | Rare rash | Prolonged QT interval risk |
| Cefuroxime | Diarrhea (≈8‑10%) | Rash, possible cross‑reactivity | Higher hepatic metabolism |
| Cefdinir | Loose stools (≈12%) | Rash, rare eosinophilia | Stools may turn red‑orange |
| Penicillin V | Stomach upset (≈10%) | Rash, higher anaphylaxis risk | Not for β‑lactamase producers |
| Clarithromycin | Nausea, taste disturbances | Rash, rare hepatotoxicity | Drug‑drug interactions (CYP3A4) |
| Doxycycline | Esophagitis, photosensitivity | Rare severe skin reaction | Contraindicated in pregnancy (Category D) |
Overall, Cefaclor’s side‑effect burden sits in the mid‑range. Patients with a known penicillin allergy often benefit from a macrolide like Azithromycin, while those needing a broader Gram‑negative cover may prefer Cefuroxime or Cefdinir.

Pharmacokinetics and Dosing Differences
Choosing an alternative often boils down to how easy the regimen is for the patient. Here’s a concise breakdown:
- Cefaclor: 250‑500mg every 6hours (four times daily). Food slows absorption slightly but does not affect efficacy.
- Amoxicillin: 500mg every 8hours or 875mg twice daily. Can be taken with meals.
- Azithromycin: 500mg once daily for 3days (or 500mg on day1 then 250mg days2‑5). No food restrictions.
- Cefuroxime: 250‑500mg every 12hours. Food improves absorption.
- Cefdinir: 300mg every 12hours. Take with a full glass of water.
- Penicillin V: 500mg every 6‑8hours; must be taken on an empty stomach.
- Clarithromycin: 250‑500mg every 12hours; best taken with food to reduce GI upset.
- Doxycycline: 100mg twice daily; avoid taking just before bedtime without food.
Patients who struggle with four times daily dosing often find a once‑daily macrolide or a twice‑daily cephalosporin more adherent.
Choosing the Right Antibiotic - Decision Guide
Below is a practical flow you can use during a primary‑care visit:
- Confirm the suspected pathogen and local resistance patterns.
- Check patient’s allergy history - especially penicillin or macrolide reactions.
- Assess special populations: pregnancy, renal impairment, or known QT‑prolongation.
- Match the infection to the drug’s spectrum (e.g., Cefaclor for mixed‑flora sinusitis, Azithromycin for atypical pneumonia).
- Consider dosing convenience - aim for the fewest daily doses that maintain efficacy.
- Review drug‑drug interaction potential, especially with macrolides and clarithromycin.
- Finalize the prescription and give clear counseling on side‑effects and adherence.
Using this checklist, a clinician might start with Cefaclor for a straightforward ear infection, but switch to Azithromycin if the patient reports a penicillin allergy, or pick Cefuroxime when a stronger Gram‑negative push is needed.
Bottom Line Summary
Ceclor CD (Cefaclor) remains a solid, mid‑range oral cephalosporin for common respiratory and urinary infections. Its Cefaclor alternatives-including Amoxicillin, Azithromycin, Cefuroxime, Cefdinir, and Doxycycline-offer varied spectra, dosing schedules, and safety profiles that can better fit individual patient needs. The key is to match infection type, allergy status, pregnancy considerations, and convenience together. When used wisely, any of these agents can clear the infection while minimizing resistance and side‑effects.
Frequently Asked Questions
Is Cefaclor safe for children?
Yes. Cefaclor is approved for pediatric use down to 6months of age for ear, sinus, throat, and urinary infections. Dosing is weight‑based, usually 10‑20mg/kg every 6hours.
Can I take Cefaclor with food?
Food modestly slows absorption but does not compromise effectiveness. If stomach upset is an issue, taking it with meals can help.
What makes Azithromycin a popular alternative?
Its long half‑life allows a simple once‑daily regimen, and it covers many atypical organisms that Cefaclor does not. However, it can affect heart rhythm in susceptible patients.
How does renal impairment affect Cefaclor dosing?
Since the kidneys clear most of the drug, patients with CrCl<30mL/min need a reduced dose (often 250mg every 12hours) to avoid accumulation and toxicity.
When should I choose a third‑generation cephalosporin over Cefaclor?
If the infection involves resistant Gram‑negative bacteria-such as certain Enterobacteriaceae-or if local patterns show high cefaclor resistance, a third‑generation agent like Cefdinir provides stronger coverage.
Is there cross‑reactivity between Cefaclor and penicillins?
Cross‑reactivity exists but is lower than with first‑generation cephalosporins-about 2‑5%. Patients with a severe penicillin allergy should generally avoid Cefaclor and use a macrolide or tetracycline instead.
Can Cefaclor be used for COVID‑19‑related bacterial pneumonia?
Only if a bacterial co‑infection is documented. Cefaclor’s spectrum covers typical Streptococcus pneumoniae but not atypical pathogens like Mycoplasma, which would need a macrolide.




The safety profile for pregnant patients is clearly highlighted.
Choosing a pregnancy‑safe antibiotic can feel like navigating a maze, but amoxicillin often cuts through the confusion!
Its well‑documented safety in trimester‑specific studies makes it a reliable first‑line option.
Meanwhile, the alternative agents each bring their own quirks that can either simplify or complicate therapy.
When weighing Cefaclor against its alternatives, the first factor to examine is the spectrum of activity and how it aligns with the suspected pathogen.
Cefaclor covers many Gram‑positive organisms and a modest range of Gram‑negative species, yet it falters against beta‑lactamase‑producing strains.
Amoxicillin, while sharing a similar beta‑lactam backbone, boasts superior coverage of Haemophilus influenzae, which is a common culprit in sinus infections.
Azithromycin steps in with a completely different mechanism, inhibiting the 50S ribosomal subunit, and its prolonged half‑life allows for a convenient three‑day regimen.
However, azithromycin’s propensity to provoke QT prolongation makes it less attractive for patients with cardiac risk factors.
Cefuroxime raises the stakes by offering enhanced Gram‑negative activity and higher oral bioavailability, positioning it as a solid second‑line choice when resistance looms.
Cefdinir pushes the envelope further into third‑generation territory, delivering robust coverage of atypical organisms but at the cost of increased expense.
If a patient cannot tolerate beta‑lactams, macrolides such as clarithromycin provide a viable plug, though cross‑reactivity remains a concern for true penicillin allergies.
Doxycycline serves a niche role for intracellular pathogens and certain resistant UTIs, but its contraindication in pregnancy limits its use in that demographic.
Renal function is another pivotal consideration; because Cefaclor is primarily renally excreted, dose adjustments are mandatory for patients with impaired glomerular filtration.
In contrast, azithromycin’s hepatic metabolism offers a safety cushion for those with compromised kidneys.
From a pharmacokinetic standpoint, the time‑dependent killing of beta‑lactams underscores the importance of maintaining serum concentrations above the MIC for the entire dosing interval.
This principle explains why multiple daily dosing of Cefaclor may be preferable to a once‑daily macrolide in severe infections.
Cost‑effectiveness also swings the pendulum; generic amoxicillin and cefuroxime often undercut the price tags of newer agents like azithromycin.
Ultimately, the clinician must balance microbial coverage, patient comorbidities, safety in special populations, and economic factors before settling on the optimal therapy.
In practice, many providers start with amoxicillin for uncomplicated sinusitis in pregnant patients, reserving Cefaclor or cefuroxime for cases with documented beta‑lactamase production.
In the grand tapestry of antimicrobial stewardship, each drug weaves its own filament, tugging at the delicate balance between efficacy and safety.
When one pulls too hard on the thread of broad‑spectrum coverage, the pattern of resistance can become knotted beyond repair.
Thus, the choice of Cefaclor versus its cousins is less a matter of simple substitution and more a philosophical negotiation with microbial ecology.
The clinician, acting as both carpenter and curator, must decide whether to reinforce the structure with a familiar beam or to experiment with an avant‑garde alloy.
Such decisions reverberate beyond the immediate infection, echoing into community health, pharmacoeconomics, and even patient trust.
Therefore, an informed selection is not merely a prescription but a covenant with future generations of patients.
That perspective really brings the bigger picture into focus, reminding us that every antibiotic choice has ripple effects.
Thanks for sharing such a thoughtful reflection.