 11
Dec,2025
11
Dec,2025
More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the twist: up to 90% of them aren’t. That’s not a typo. Most people who think they’re allergic to penicillin can safely take it again-after proper testing. The same goes for NSAIDs like ibuprofen and aspirin. Yet, because of mislabeled allergies, patients end up on stronger, costlier, and sometimes riskier antibiotics. This isn’t just a personal health issue-it’s a systemic problem in healthcare. So how do you know if you’re truly allergic? And what can you do if you need a drug you’re labeled allergic to?
What Really Counts as a Drug Allergy?
Not every bad reaction to a drug is an allergy. A true drug allergy involves your immune system. It’s not just a stomach ache or a headache. It’s your body treating the drug like a threat. Symptoms like hives, swelling, trouble breathing, or a sudden drop in blood pressure? Those are red flags. They usually show up within an hour of taking the drug. That’s called an immediate-type reaction, and it’s the kind that triggers desensitization protocols.But here’s where it gets messy. Many people report a penicillin allergy because they got a rash as a kid, or their mom said they were allergic. But rashes from viruses, like mononucleosis, are often mistaken for penicillin allergies. Skin testing and drug challenges can clear this up. The American Academy of Allergy, Asthma & Immunology says the gold standard is a negative skin test followed by a full dose of amoxicillin. If nothing happens, you’re not allergic.
Penicillin Allergy: The Most Misunderstood Drug Reaction
Penicillin is the most common drug allergy reported. But it’s also the most overdiagnosed. Studies show that people labeled penicillin-allergic are more likely to get broad-spectrum antibiotics like vancomycin or ciprofloxacin. These drugs cost more, cause more side effects, and increase the risk of resistant infections like C. diff. Hospitals lose money. Patients lose time. And the cycle continues because no one questions the label.Penicillin skin testing uses two components: major determinant (penicilloyl-polylysine, or PPL) and minor determinant (a mix including penicillin G and metabolites). But here’s the catch: PPL alone can give false positives. Up to 70% of people who react to PPL don’t react to actual penicillin. That’s why testing must include both. If the skin test is negative, a supervised oral challenge with amoxicillin confirms safety. Most patients pass without issue.
Even if you had a severe reaction years ago-like anaphylaxis-it doesn’t mean you’re allergic forever. Allergies can fade. The risk of re-sensitization after a negative test is less than 2%. That’s why experts now say: if you were told you were allergic to penicillin decades ago, get retested.
NSAID Allergies: Different Mechanism, Same Problem
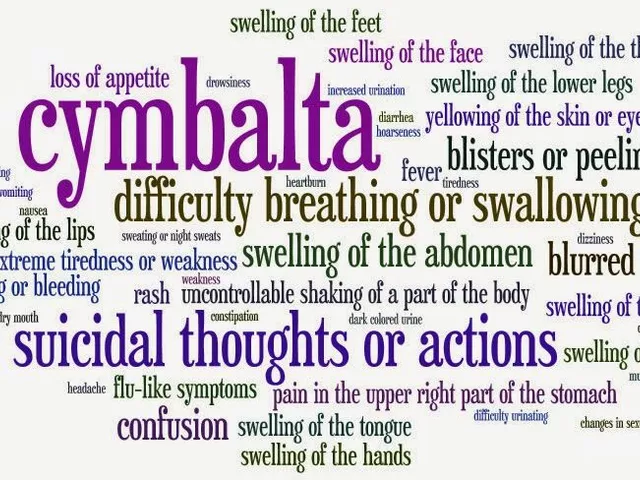
NSAIDs like aspirin, ibuprofen, and naproxen cause a different kind of reaction. It’s not IgE-mediated like penicillin. Instead, it’s often linked to how they block enzymes in your body, triggering inflammation in the airways. People with asthma or nasal polyps are especially prone. Symptoms? Wheezing, nasal congestion, hives, sometimes anaphylaxis. It’s not rare. About 1 in 20 people with asthma react to NSAIDs.Unlike penicillin, you can’t test for NSAID allergy with a skin prick. Diagnosis is based on history and, sometimes, a supervised challenge. But here’s the good news: for many, daily low-dose aspirin can actually help. Desensitization protocols for NSAIDs involve slowly increasing doses-starting at 30 mg of aspirin, then 60 mg, 100 mg, up to 325 mg over several hours. Once desensitized, patients can take daily aspirin without reactions. This isn’t just about pain relief. For people with chronic sinus disease or heart conditions, it’s life-changing.
How Desensitization Works: Temporary Tolerance, Not a Cure
Desensitization isn’t a cure. It’s a temporary reset. Your immune system is tricked into tolerating the drug-for one treatment cycle. Once you stop taking it, the tolerance fades. You’ll need to go through it again if you need the drug later.The most common protocol is the 12-step method, used for penicillin and other beta-lactams. It starts with a tiny fraction of the dose-sometimes one ten-thousandth of the full amount. Every 15 to 20 minutes, the dose doubles. The whole process takes 4 to 8 hours. Some hospitals use accelerated versions. One protocol at Brigham and Women’s Hospital finishes in just 2 hours and 15 minutes by tripling the dose every 15 minutes.
It’s done in a hospital setting, with IV access, epinephrine ready, and staff trained to handle anaphylaxis. If a patient gets severe hypotension or swelling that doesn’t respond to treatment, the process stops. No exceptions. Safety comes first.
Desensitization isn’t just for penicillin. It’s been done successfully with cephalosporins like cefazolin and ceftriaxone, chemotherapy drugs like paclitaxel, and even antifungals like fluconazole. The key is: no safe alternative exists. If you have a life-threatening infection and the only effective drug is one you’re allergic to, desensitization becomes your best-and sometimes only-option.
Who Can Get Desensitized? And Who Shouldn’t?
Not everyone qualifies. You need two things: a confirmed immediate allergic reaction to the drug, and no other reasonable alternative. If you can take a different antibiotic or painkiller, you won’t be offered desensitization.Children are trickier. Most protocols were designed for adults. Pediatric use is growing, but guidelines are still catching up. Kids with cancer, cystic fibrosis, or recurrent infections are the best candidates. If they’ve had a clear IgE-mediated reaction, desensitization can be lifesaving. But it requires close coordination between allergists, pediatricians, and infectious disease specialists.
People with non-immediate reactions-like a rash that shows up days later-are usually not candidates. Those reactions are T-cell mediated and don’t respond to desensitization. And if you’ve had a severe reaction like Stevens-Johnson syndrome, desensitization is off the table. Too risky.
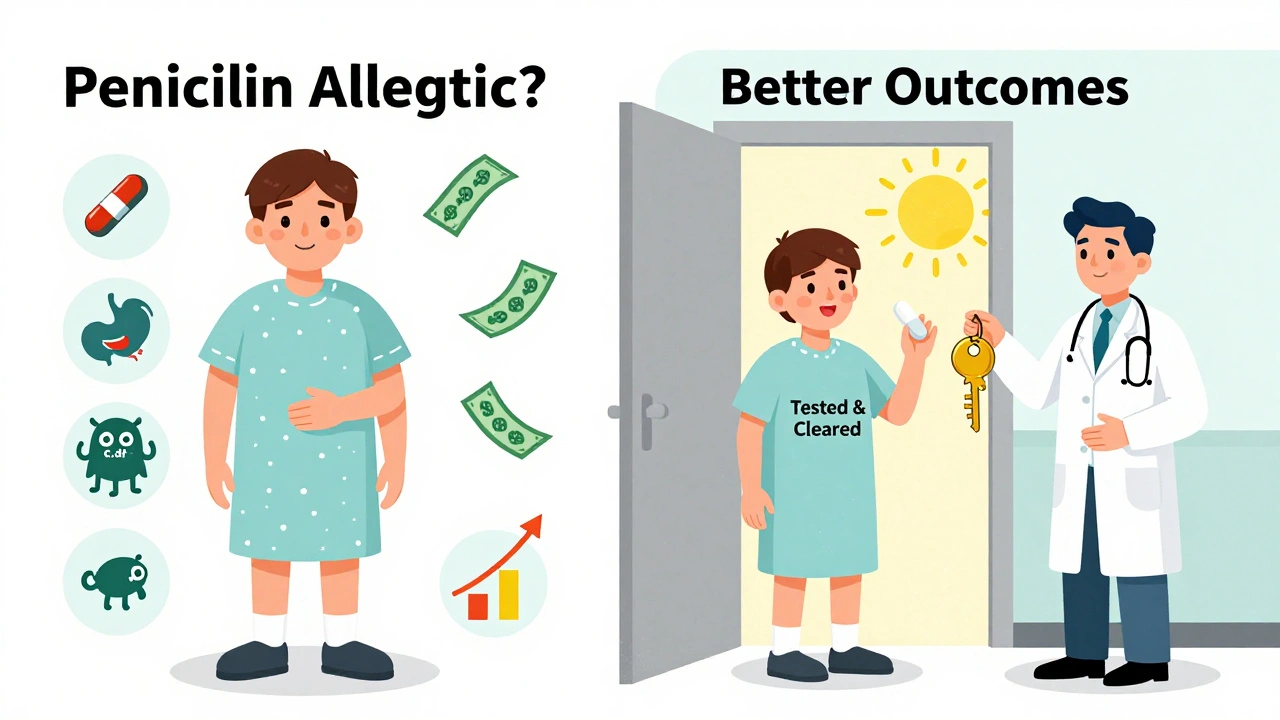
Why This Matters: Cost, Safety, and the Bigger Picture
Labeling someone penicillin-allergic adds about $500 to their hospital bill. Why? Because they get broader-spectrum antibiotics-drugs that are more expensive and harder on the gut microbiome. That leads to longer stays, more complications, and higher rates of antibiotic resistance.Desensitization flips the script. It lets patients get the right drug, safely. It reduces costs. It saves lives. But it’s underused. Only a handful of hospitals have dedicated allergy teams trained in desensitization. Most general practitioners don’t know how to refer patients. And many patients don’t even know they can be retested.
The solution? Better education. Better testing. Better access. If you’ve been told you’re allergic to penicillin-or any drug-ask: Was it confirmed? Can I get tested? Is there a way to safely use this drug again? Don’t assume the label is permanent. It might not be.
What to Do If You Think You’re Allergic
Step one: Don’t panic. Don’t avoid all antibiotics. Don’t assume you’re allergic just because you had a reaction years ago.Step two: Talk to your doctor. Ask if you’ve ever had a proper allergy evaluation. If not, ask for a referral to an allergist. Skin testing for penicillin takes 30 minutes. A drug challenge takes a few hours. Both are safe when done right.
Step three: If you need a drug you’re allergic to, ask about desensitization. It’s not magic. But it’s science-and it works. Hospitals like Brigham and Women’s, Johns Hopkins, and Mayo Clinic have done hundreds of these procedures. You don’t need to be in a big city to access them. Many regional centers now offer it too.
Step four: Update your records. If testing shows you’re not allergic, make sure your medical chart, pharmacy profile, and emergency bracelet reflect that. A simple change can prevent years of unnecessary risk.
Drug allergies are real. But they’re often misunderstood. The truth is, you don’t have to live with a label that doesn’t fit. With the right testing and protocols, you can get back to the drugs you need-safely, effectively, and without fear.
Can I outgrow a penicillin allergy?
Yes. Many people lose their penicillin allergy over time, especially if it was diagnosed in childhood. Studies show that up to 90% of people who report a penicillin allergy can tolerate it after proper testing. Skin tests and oral challenges are the best way to confirm this. Even if you had a severe reaction years ago, retesting is safe and often reveals you’re no longer allergic.
Is NSAID desensitization permanent?
No. NSAID desensitization only lasts as long as you keep taking the drug daily. If you stop for more than a few days, your body may lose tolerance. That’s why it’s mainly used for patients who need daily aspirin-for heart protection or chronic sinus issues. You can’t just take it once and expect to be protected forever. It’s a maintenance therapy, not a cure.
Can children be desensitized to drugs?
Yes, but it’s more complex. Most protocols were developed for adults and adapted for kids. Children with cancer, cystic fibrosis, or serious infections are the best candidates. Desensitization has been done successfully with antibiotics, chemotherapy, and monoclonal antibodies in kids. It requires a team approach-pediatric allergists, infectious disease specialists, and oncologists working together. Standardized pediatric guidelines are still being developed.
What happens if I have a reaction during desensitization?
The procedure is stopped immediately. Medical staff are trained to treat anaphylaxis with epinephrine, antihistamines, and IV fluids. Most reactions are mild-flushing, itching, or nausea-and can be managed with medication while continuing the protocol. But if you develop severe breathing trouble, low blood pressure, or swelling that doesn’t respond quickly, the process is halted permanently. Safety is always the priority.
Do I need to be hospitalized for desensitization?
Yes. Desensitization must be done in a controlled medical setting with immediate access to emergency equipment and trained personnel. This includes hospitals or specialized allergy clinics. It’s not something you can do at home or in a regular doctor’s office. The process takes several hours, and reactions can happen at any point. You’ll be monitored closely the entire time.
Can I be desensitized to multiple drugs at once?
No. Desensitization is done one drug at a time. Trying to desensitize to multiple drugs simultaneously increases the risk of confusion and complications. If you need two drugs you’re allergic to, they’re done separately, with at least a few days between. Each desensitization is a standalone procedure.
Are there alternatives to desensitization?
Yes-if a safe alternative exists. For penicillin allergies, doctors may switch to macrolides like azithromycin or tetracyclines. For NSAID allergies, acetaminophen or COX-2 inhibitors like celecoxib may be options. But in cases of severe infection, cancer, or autoimmune disease, alternatives may be less effective, more toxic, or unavailable. That’s when desensitization becomes the best choice.





I used to say I was allergic to penicillin because my mom said so. Turned out I never was. Got tested last year after a bad UTI and they gave me amoxicillin like it was nothing. No hives, no swelling, just a really boring afternoon in the clinic. Wish I’d known sooner.
Now I feel dumb for avoiding it for 12 years.
Of course 90% of people aren’t really allergic. That’s why we need to stop coddling people who think a rash from a virus means they’re allergic to everything. You get a rash, you get a virus. Not a drug allergy. Stop making healthcare more expensive because you’re scared to take a pill.
And stop calling it a "systemic problem." It’s just people being lazy and misinformed.
My brother was told he was allergic to penicillin as a kid after a rash. He’s 42 now. Last year he needed it for a serious lung infection. They did the skin test, then the oral challenge. He’s fine. No reaction.
They updated his records. His pharmacy now knows. He didn’t have to take vancomycin. Saved thousands. And he didn’t get C. diff.
Stop assuming. Get tested. It’s not that hard.
My cousin was allergic to NSAIDs and had asthma. She couldn’t take ibuprofen for her arthritis. Tried aspirin desensitization. Started at 30 mg. Took three hours. Now she takes 81 mg daily. Her joints don’t hurt. Her sinuses cleared up. She hasn’t had a flare in two years.
It’s not magic. It’s science. And it works.
If you think you’re allergic to something, don’t just live with it. Ask. Push. Get help. You deserve to feel better.
And if you’re a doctor? Refer them. It’s not that complicated.
so like… i got a rash once when i was 7 and now im allergic to penicillin forever? no thanks. i mean, come on. i think people just wanna be special. "oh i can’t take that, i’m allergic" like its a badge. i had a rash from chicken pox and they called it penicillin allergy. dumb.
also why is this even a thing? why do hospitals not just test people? they dont care. they just want to give you the expensive stuff.
Desensitization protocols for penicillin are safe, effective, and underused. The 12-step method has been validated in hundreds of studies. The risk of reaction during the process is less than 5%, and most reactions are mild.
Patients who undergo desensitization have shorter hospital stays, lower rates of antibiotic resistance, and better outcomes.
If you’re told you’re allergic, ask for a referral to an allergist. It takes 30 minutes to test. It takes hours to desensitize. But it can change your life.
This isn’t niche medicine. It’s standard care. And it’s available in most major hospitals.
Don’t let a childhood label decide your treatment for the next 50 years.
Everyone deserves to be safe. Everyone deserves to be heard. If you think you’re allergic, don’t be afraid to ask. Don’t be ashamed to get tested. You’re not weak for wanting to be healthy. You’re smart.
And if you’re a doctor? Help them. Don’t just write a script. Ask questions. Look deeper. You might save someone from years of unnecessary pain.
It’s not about being right. It’s about being kind.
90% of people aren’t allergic? That’s because they’re idiots who can’t tell the difference between a rash and an allergy. You get a rash from a virus? That’s not an allergy. That’s a virus. Stop blaming the drug.
And desensitization? It’s a scam. You’re not "resetting" your immune system. You’re just risking anaphylaxis for no reason. Why not just take the expensive antibiotic like everyone else?
People need to stop being so dramatic about their health. It’s not a superhero origin story.
wait so you’re telling me… i could’ve taken amoxicillin all this time?? i thought i was allergic because my grandma said so… and now i’m supposed to go to a hospital and get poked and prodded for hours?? why didn’t anyone tell me this before??
my doctor just said "don’t take penicillin" and that was it. no test. no explanation. just a label.
why is healthcare like this?? why do we just accept these labels??
also… i think i’m allergic to doctors who don’t explain things.