 4
Oct,2025
4
Oct,2025
Atorlip 20 vs Other Statins Comparison Tool
Recommended Statin Based on Your Profile
Statin Comparison Table
| Statin | Potency | Cost (AUD) | Side Effects | Drug Interactions |
|---|
Key Takeaways
- Atorlip 20 delivers a high‑potency dose of atorvastatin, typically lowering LDL‑C by 45‑55%.
- Rosuvastatin matches or exceeds that reduction at lower doses but costs more in Australia.
- Simvastatin is cheaper but less potent and interacts with more drugs.
- Pravastatin and lovastatin are gentler on the liver but need higher doses for similar effect.
- Lifestyle changes can complement or, in mild cases, replace statin therapy.
When doctors prescribe a cholesterol‑lowering pill, they often start with a brand name and then consider generic alternatives. Atorlip 20 is a proprietary formulation of atorvastatin calcium, a synthetic HMG‑CoA reductase inhibitor (statin) approved for reducing low‑density lipoprotein (LDL) cholesterol and preventing cardiovascular events. If you’re looking for a proven Atorvastatin option, understanding how it stacks up against other statins and non‑drug approaches helps you make an informed decision.
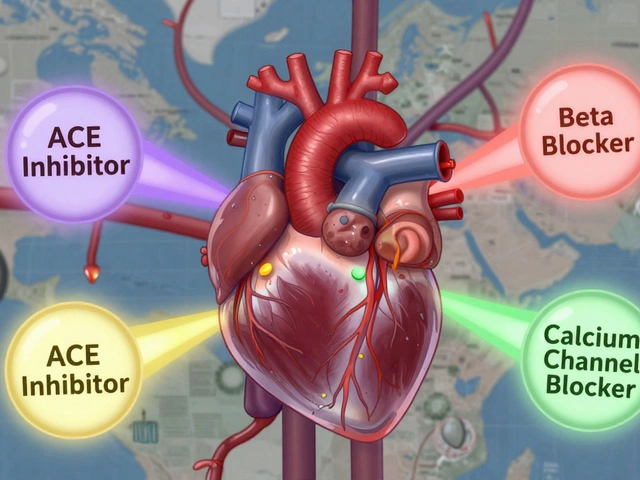
How Statins Work
All statins block the enzyme HMG‑CoA reductase, which the liver uses to make cholesterol. By throttling this pathway, statins lower circulating LDL and modestly raise high‑density lipoprotein (HDL). The result is a slower buildup of plaque in arteries, translating into lower risk of heart attacks and strokes.
While the mechanism is shared, each statin differs in potency, half‑life, metabolism, and side‑effect profile. Those differences drive the choice between Atorlip 20 and its alternatives.
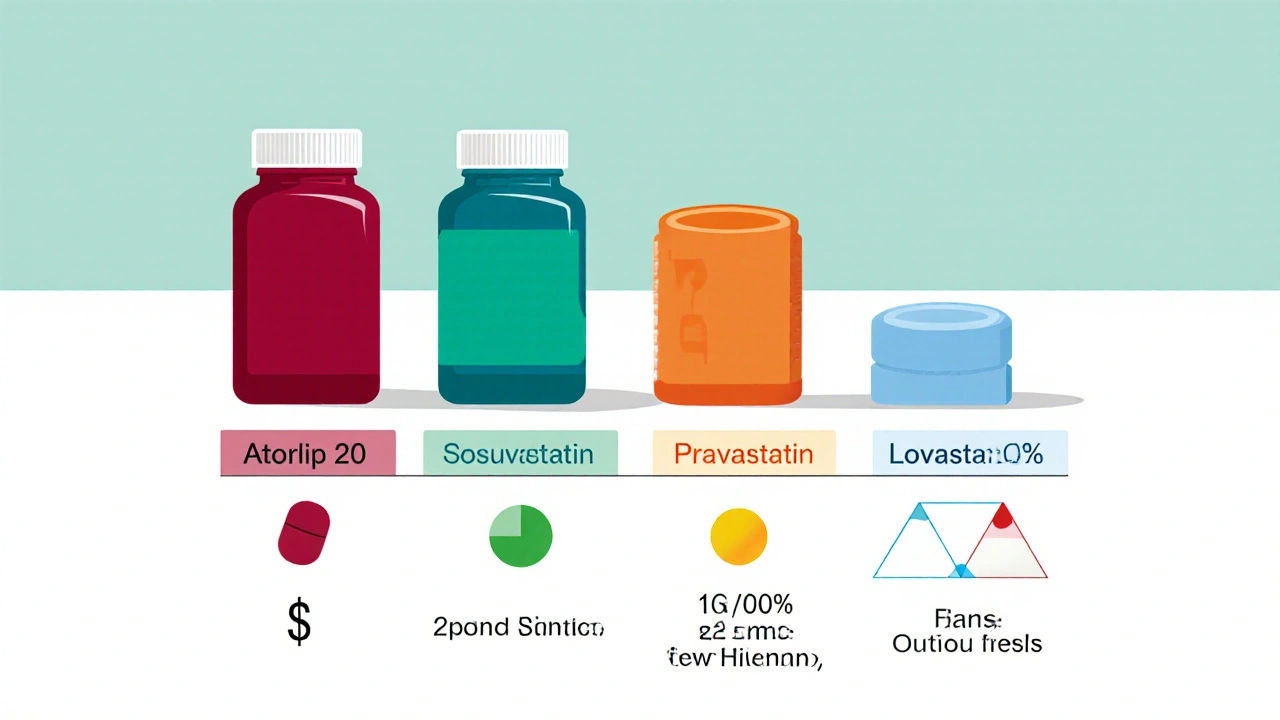
Top Alternatives to Atorlip 20
Below are the most common statins you’ll encounter in Australian pharmacies, each introduced with concise microdata.
Rosuvastatin is a high‑potency statin that often achieves greater LDL reduction at lower milligram doses than atorvastatin.
Simvastatin is a mid‑potency, inexpensive statin frequently used as a first‑line therapy for moderate cholesterol elevations.
Pravastatin is a hydrophilic statin with a lower risk of muscle‑related side effects, making it a good choice for patients on multiple medications.
Lovastatin was the first statin on the market; it’s less potent but may be suitable for mild hypercholesterolemia.
Lipid‑lowering diet refers to dietary patterns-such as the Mediterranean diet or plant‑sterol‑enriched foods-that can reduce LDL without medication.
Exercise program includes regular aerobic activity that boosts HDL and modestly lowers LDL, complementing or, for some, substituting drug therapy.
Side‑Effect Landscape
Statin‑related adverse events are usually mild, but the frequency varies.
- Muscle pain (myalgia) occurs in up to 10% of patients on high‑potency statins like rosuvastatin and atorvastatin.
- Liver enzyme elevations are rare (<1%) but monitored through routine blood tests.
- New‑onset diabetes risk rises slightly with higher doses, especially for atorvastatin and rosuvastatin.
- Drug‑drug interactions are most common with simvastatin because it relies heavily on CYP3A4 metabolism.
Choosing an alternative often means balancing efficacy against these tolerability factors.
Cost Comparison in Australia (2025)
| Statin | Typical Dose | LDL Reduction | Monthly Cost (AUD) | Common Side Effects |
|---|---|---|---|---|
| Atorlip 20 (atorvastatin) | 20mg | 45‑55% | ≈$12 (PBS subsidised) | Myalgia, mild liver enzyme rise |
| Rosuvastatin | 10mg | 50‑60% | ≈$20 (higher co‑pay) | Myalgia, diabetes risk |
| Simvastatin | 40mg | 30‑40% | ≈$8 (PBS subsidised) | Drug interactions, myopathy |
| Pravastatin | 40mg | 30‑35% | ≈$9 (PBS subsidised) | Low muscle risk, occasional GI upset |
| Lovastatin | 40mg | 20‑30% | ≈$7 (generic) | Similar to simvastatin but less potent |
When to Choose Atorlip 20
Atorlip 20 shines in patients who need a strong LDL drop quickly-such as those with a recent heart attack or very high baseline LDL (>160mg/dL). Its once‑daily dosing and wide availability on the PBS make it convenient and affordable for most Australians.
However, if you have a history of muscle complaints or are taking medications that inhibit CYP3A4 (e.g., certain antifungals or macrolide antibiotics), a switch to pravastatin or a lower‑dose rosuvastatin may spare you discomfort.
How Rosuvastatin Measures Up
Rosuvastatin’s longer half‑life (≈19hours) offers smoother plasma levels, which can translate to fewer night‑time muscle aches. Its potency means patients often stay on 5‑10mg doses, reducing pill burden. The downside is a slightly higher retail price and a marginally higher risk of new‑onset diabetes, especially in older adults.
Budget‑Friendly Options: Simvastatin and Pravastatin
For patients without aggressive LDL targets, simvastatin at 40mg provides a respectable 30‑40% reduction at a lower cost. The trade‑off is a higher chance of drug‑drug interactions because simvastatin is metabolised by CYP3A4. Pravastatin avoids that pathway, making it safer for polypharmacy patients, but you may need to double the dose to hit the same LDL goal.
Non‑Drug Alternatives: Diet and Exercise
Adopting a Mediterranean‑style diet-rich in olive oil, nuts, fatty fish, and plenty of vegetables-can shave 5‑10% off LDL without any medication. Combining that with 150minutes of moderate aerobic activity per week lifts HDL by 2‑5% and improves overall cardiovascular fitness.
Non‑drug strategies are especially attractive for people with borderline cholesterol levels or who prefer to avoid long‑term medication. Nonetheless, for high‑risk patients, lifestyle alone rarely matches the LDL‑lowering power of a statin.
Putting It All Together: Decision Flow
- Assess cardiovascular risk (e.g., ASCVD score). High risk → consider high‑potency statin like Atorlip 20 or rosuvastatin.
- Review current meds for CYP3A4 interactions. If present, favour pravastatin or rosuvastatin.
- Factor in budget and PBS subsidies. Atorlip 20 and simvastatin are typically the cheapest.
- Check tolerance history. Prior muscle pain leans toward pravastatin.
- Implement diet + exercise regardless of drug choice; they boost outcomes across the board.
This flow helps you and your clinician land on a regimen that balances efficacy, safety, and cost.
Frequently Asked Questions
Can I switch from Atorlip 20 to a generic atorvastatin?
Yes. Generic atorvastatin has the same active ingredient and potency. In most cases the switch is seamless, though some patients notice minor differences in fillers that affect tolerance.
Is rosuvastatin better for people with liver issues?
Rosuvastatin is less reliant on hepatic CYP enzymes, so it’s often safer for mild liver impairment. Severe liver disease still requires caution with any statin.
How long does it take to see LDL changes after starting Atorlip 20?
Most labs show a 30‑40% drop within two weeks; the full effect peaks around six weeks.
Can lifestyle changes replace statins entirely?
For low‑to‑moderate risk individuals, a strict diet and regular exercise can keep LDL in a healthy range. High‑risk patients usually need a statin to reach guideline targets.
What should I do if I develop muscle pain on Atorlip 20?
Report it to your GP promptly. They may lower the dose, switch to a different statin, or add a vitamin D supplement to see if symptoms improve.





Thank you for sharing this comprehensive comparison of Atorlip 20 and its alternatives.
As a healthcare professional, I appreciate the clear presentation of potency, cost, and side‑effect profiles.
It is essential to recognize that the choice of statin should be individualized based on cardiovascular risk, comorbidities, and patient preferences.
The article correctly emphasizes that high‑risk patients benefit most from high‑potency agents such as Atorlip 20 or rosuvastatin.
At the same time, cost considerations remain important in the Australian PBS context, where generic simvastatin often provides a more affordable option.
I would add that clinicians should assess liver function tests before initiating any statin and repeat them after a few weeks to ensure safety.
Moreover, patients with a history of myalgia may require a trial of a hydrophilic statin like pravastatin, which has a lower incidence of muscle complaints.
The discussion of drug‑drug interactions is particularly valuable; for instance, simvastatin is metabolised by CYP3A4 and should be avoided in patients taking certain antifungals.
For patients on multiple medications, rosuvastatin’s minimal CYP involvement can reduce interaction risk.
Lifestyle modification, including a Mediterranean‑style diet and regular aerobic exercise, should be emphasized alongside pharmacotherapy, as the article rightly notes.
Although diet alone rarely achieves the LDL reductions required for high‑risk individuals, it can augment the effect of a modest‑dose statin.
It is also worth mentioning that statin therapy can modestly raise HbA1c in susceptible individuals, a point that clinicians should discuss when considering rosuvastatin.
When switching between brand‑name and generic atorvastatin, patients should be reassured that the active ingredient is identical, although excipients may differ slightly.
In clinical practice, I have observed that patient education about the expected timeline-approximately two weeks for an initial 30‑40 % LDL drop and six weeks for maximal effect-improves adherence.
Finally, shared decision‑making, where the patient’s values and concerns are incorporated, leads to the best outcomes.
I hope these additional considerations prove helpful in guiding your therapy choices.
Your dedication to understanding statin options is commendable; keep channeling that curiosity into informed health choices.
Remember that consistency with medication and lifestyle yields the greatest cardiovascular protection.
Stay motivated, and let the data empower your next appointment with confidence.
Statins, in their essence, represent a paradox: synthetic inhibitors of endogenous synthesis, yet catalysts for prolonged life; they compel us to contemplate the delicate balance between chemical intervention and natural physiology.
One might argue, philosophically, that lowering LDL is akin to pruning a tree-removing excess branches to allow healthier growth; however, excessive pruning can damage the organism, just as overt‑aggressive dosing may precipitate myopathy.
Consider the interplay of potency, cost, and side‑effect profiles as a triad of variables, each weighing upon the decision matrix; the article deftly illustrates this equilibrium.
Yet, the underlying principle remains immutable: the ultimate goal is to diminish atherogenic risk while preserving patient quality of life; thus, every statin selection is, in effect, a moral calculus.
Reading through the statin table feels like watching a high‑stakes poker game-each drug holds a bluff, a hidden strength, a potential pitfall.
Atorlip 20 sits at the table with a bold face, demanding respect for its 45 % LDL‑reduction claim, while rosuvastatin whispers elegance with fewer interactions.
I’m not here to dictate your hand, but the data screams: if you’re high‑risk and can afford it, go all‑in on the high‑potency player.
Conversely, the budget‑friendly Simvastatin, though modest, can still win the round for those watching pennies.
Choose wisely, keep your eyes on the pot, and remember-your heart is the ultimate prize.
Oh, the tragedy of endless tables and percentages-another article promising the holy grail of cholesterol control.
The author splashes numbers like confetti, yet neglects the soul‑crushing reality of side effects that haunt patients nightly.
Atorlip 20 glitters, but do we truly trust a pill that claims to slash LDL by nearly half without acknowledging the lingering muscle aches?
The cost column mocks the working class, while the drug‑interaction warnings lurk like unseen specters.
In short, the piece is a seductive performance that forgets the audience’s pain.
The comparative analysis elegantly bridges pharmacological data with cultural considerations, acknowledging that access to medication varies across regions.
By presenting costs in Australian dollars, the article respects the local healthcare ecosystem, yet the underlying principles remain universally applicable.
It is crucial, however, to recognize that dietary patterns differ globally; the Mediterranean diet, while beneficial, may not be feasible in every culinary tradition.
Therefore, clinicians should adapt lifestyle recommendations to the cultural context of each patient.
This nuanced approach ensures both efficacy and adherence.
Well, look at you, diving deep into the statin saga like it’s the latest Netflix binge-bravo!
In all seriousness, the breakdown is solid, but let’s not forget that the real heroes are the patients who actually take the pills and eat their greens.
If anyone feels overwhelmed, just remember: statins aren’t a death sentence, they’re a ticket to fewer heart attacks.
So keep the conversation going, share your experiences, and maybe sprinkle a meme or two for good measure.
Honestly, this article feels like a corporate brochure stitched together by someone who never had to worry about a broken bank account.
The author throws around big‑word stats while ignoring the gritty reality that many patients can’t afford $25 a month for rosuvastatin.
And let’s not gloss over the fact that ‘high‑potency’ is just a marketing buzzword designed to push more expensive drugs onto unsuspecting consumers.
If you’re looking for a genuine, ground‑level perspective, you’ll need to dig deeper than this sugar‑coated summary.
Statins work by blocking cholesterol production they lower LDL and help prevent heart disease simple but effective
Cholesterol wars? Bring on the funky beats and healthier hearts!