Ethambutol Dosing: What You Need to Know
When working with Ethambutol dosing, the process of calculating the correct amount of ethambutol for treating tuberculosis based on patient factors. Also known as Ethambutol dosage, it is a key part of Tuberculosis, a bacterial infection caused by Mycobacterium tuberculosis therapy. The standard regimen pairs ethambutol with Isoniazid, a first‑line drug that inhibits mycolic acid synthesis and Rifampin, a potent inducer of bacterial RNA polymerase. Together they form the backbone of modern TB treatment, and proper dosing ensures the combination works without excess toxicity.
Key Factors That Shape Ethambutol Dosing
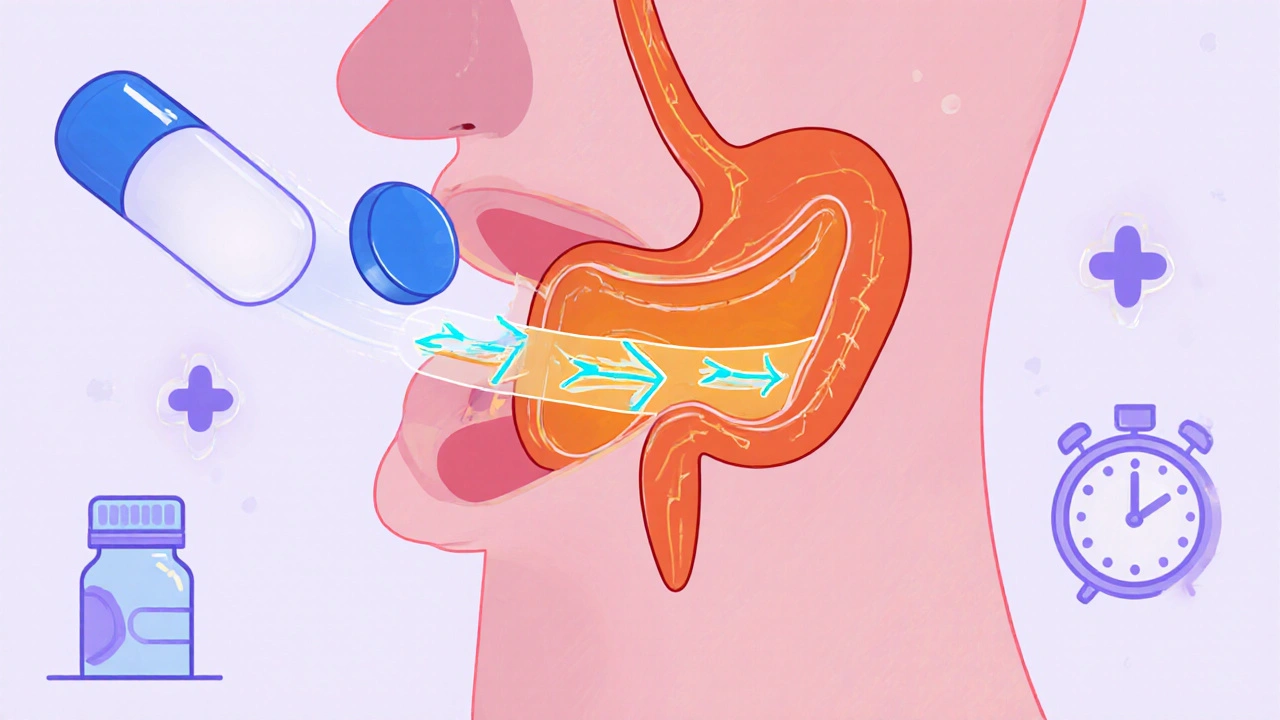
Ethambutol dosing encompasses weight‑based calculations, renal function assessment, and age‑specific adjustments. For adults, the classic formula is 15‑25 mg per kilogram of body weight per day, divided into one or two doses. However, Renal impairment, reduced kidney clearance that leads to drug accumulation forces clinicians to drop the dose by 30‑50 % when the estimated glomerular filtration rate falls below 50 mL/min. Pediatric patients aren’t just “small adults”; they need a separate dosing chart that caps at 25 mg/kg to avoid optic neuritis, a rare but serious side effect.
Another semantic link: Drug interactions, situations where one medication alters the effect of another can shift ethambutol levels. For example, co‑administration with aminoglycosides like streptomycin may heighten ototoxic risk, while concurrent use of antacids can reduce absorption. Understanding these connections helps you plan the right timing and monitoring schedule, especially when the regimen also includes Pyrazinamide, a drug that works best in acidic environments inside TB lesions for the intensive phase.
The treatment plan also dictates duration. In the intensive phase (first 2 months), ethambutol is given daily, while the continuation phase (next 4–7 months) often drops it if susceptibility testing shows the bacteria are sensitive to the other drugs. This shift is a classic example of “Ethambutol dosing requires adaptation based on microbiological response.” Monitoring liver enzymes, visual acuity, and kidney function throughout the course provides the safety net that lets clinicians tweak doses without compromising efficacy.
Practical tips for clinicians: start with the patient’s exact weight, round to the nearest whole tablet, and double‑check renal labs before finalizing the prescription. Use a dosing chart that lists both adult and pediatric ranges side by side; this visual aid minimizes errors when switching between patient populations. Educate patients to report any changes in color vision or blurred sight immediately—early detection of optic neuritis can prevent permanent damage.
Finally, remember that the success of ethambutol dosing isn’t isolated. It sits inside a larger ecosystem of TB management that includes sputum monitoring, adherence support, and public health reporting. By aligning dose calculations with these broader steps, you create a seamless workflow that improves outcomes and keeps resistance at bay.
Below you’ll find a curated set of articles that dive deeper into dosing tables, renal adjustment calculators, pediatric guidelines, and safety monitoring tools—everything you need to apply the right dose the right way.
Ethambutol Pharmacokinetics Explained: Absorption, Distribution, Metabolism, Elimination
A clear, practical guide to Ethambutol pharmacokinetics covering absorption, distribution, metabolism, excretion, dosing tweaks, interactions, and safety monitoring.
View more