 23
Oct,2025
23
Oct,2025
Ethambutol Renal Dosing Calculator
Enter Patient Information
Key Guidelines
Ethambutol is primarily renally excreted (80%), so dose adjustment is critical for renal impairment. According to the article: "Reduce dose by 50% when CrCl < 30 mL/min; consider extending the dosing interval to every 24 hours for end-stage renal disease."
Note: This calculator provides general guidance. Always consult clinical guidelines and consider individual patient factors before making dosing decisions.
Dosing Recommendation
When you hear the word ethambutol pharmacokinetics, you’re really asking how the drug moves through the body, how long it stays there, and what factors change its behavior. Understanding this helps clinicians dose correctly, avoid toxicity, and predict how the medication will work alongside other TB drugs.
Ethambutol is a synthetic antitubercular agent that inhibits arabinosyl transferase, disrupting the synthesis of the mycobacterial cell wall. It’s a key component of the standard four‑drug regimen for active Tuberculosis. Below we break down each pharmacokinetic phase, then dive into dosing tweaks for special groups, drug interactions, and therapeutic monitoring.
Absorption: How Ethambutol Enters the Bloodstream
Ethambutol is administered orally as tablets or liquid suspension. Bioavailability in healthy adults averages 80‑90% after a single dose, meaning most of the swallowed drug reaches systemic circulation. Food modestly slows the rate of absorption (increasing Tmax by 1‑2 hours) but does not reduce the overall exposure (AUC). For patients with gastrointestinal malabsorption-think Crohn’s disease or after bariatric surgery-clinicians may need to check plasma levels.
Distribution: Where the Drug Goes
After absorption, Ethambutol distributes widely. The volume of distribution (Vd) is about 0.7 L/kg, indicating moderate tissue penetration. Mycobacterium tuberculosis resides in lung tissue, macrophages, and granulomas; Ethambutol reaches therapeutic concentrations in these sites, which is why it’s effective in pulmonary TB.
Protein binding is low (about 30%), so free drug levels remain relatively high. The drug crosses the placenta and appears in breast milk at low concentrations, prompting caution in pregnant or nursing women.
Metabolism: What Happens Inside the Body
Unlike many antibiotics, Ethambutol undergoes minimal hepatic metabolism. Less than 5% of the dose is metabolized, primarily by oxidation to inactive metabolites. This makes liver disease a less critical factor for dosing, though severe hepatic dysfunction still warrants monitoring for overall drug tolerance.
Excretion: The Final Step
Renal clearance is the dominant elimination route-about 80% of an administered dose is excreted unchanged in the urine. The drug’s half‑life in individuals with normal renal function is 3‑4 hours, allowing twice‑daily dosing in most regimens. CrCl (creatinine clearance) below 30 mL/min markedly prolongs the half‑life, and dose reduction becomes essential to avoid optic neuritis.
Key Pharmacokinetic Parameters Compared with Other First‑Line TB Drugs
| Parameter | Ethambutol | Isoniazid | Rifampicin |
|---|---|---|---|
| Bioavailability | 80‑90% | ~95% | ~90% |
| Cmax (peak plasma level) | 2-3 µg/mL (400 mg dose) | 3-5 µg/mL (300 mg dose) | 8-10 µg/mL (600 mg dose) |
| Tmax (time to Cmax) | 2-3 h | 1-2 h | 2-4 h |
| Half‑life | 3‑4 h (normal renal function) | 1‑2 h | 3‑4 h |
| Clearance route | 80% renal (unchanged) | Hepatic (acetylation) | Hepatic (biliary) |
Dosing Adjustments for Special Populations
- Renal impairment: Reduce dose by 50% when CrCl < 30 mL/min; consider extending the dosing interval to every 24 hours for end‑stage renal disease.
- Pediatric patients: Weight‑based dosing (15‑20 mg/kg/day) is standard; split into two doses to keep Cmax within safe limits.
- Pregnancy: Use standard adult dosing (15 mg/kg/day) but monitor visual acuity closely, as pregnancy can increase fluid retention.
- Elderly: Assess renal function first; age‑related decline in GFR often necessitates a modest dose cut.
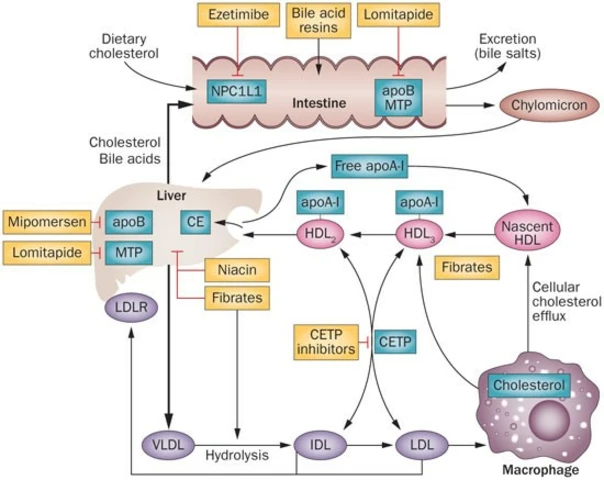
Drug-Drug Interactions That Influence Pharmacokinetics
Ethambutol’s minimal metabolism means fewer interactions than rifampicin or isoniazid, but a few still matter:
- Rifampicin: Induces hepatic transporters, modestly increasing Ethambutol clearance; clinicians may need a slight dose bump (up to 25 mg/kg) when both are used together.
- Antiretrovirals (e.g., efavirenz): No significant PK change, yet overlapping toxicities (optic neuritis vs visual disturbances) require vigilance.
- Loop diuretics: Can heighten the risk of electrolyte imbalance, indirectly affecting Ethambutol renal excretion.
Therapeutic Drug Monitoring (TDM) and Clinical Implications
Routine TDM for Ethambutol isn’t common, but it becomes valuable in:
- Patients with severe renal failure where accumulation risks optic toxicity.
- When using high‑dose Ethambutol (≥25 mg/kg) for multidrug‑resistant TB.
- Concurrent use with potent inducers or inhibitors of renal transporters.
Target trough concentrations (Cmin) should stay below 2 µg/mL to minimise neuro‑ophthalmic side effects, while maintaining Cmax above 2 µg/mL for efficacy.
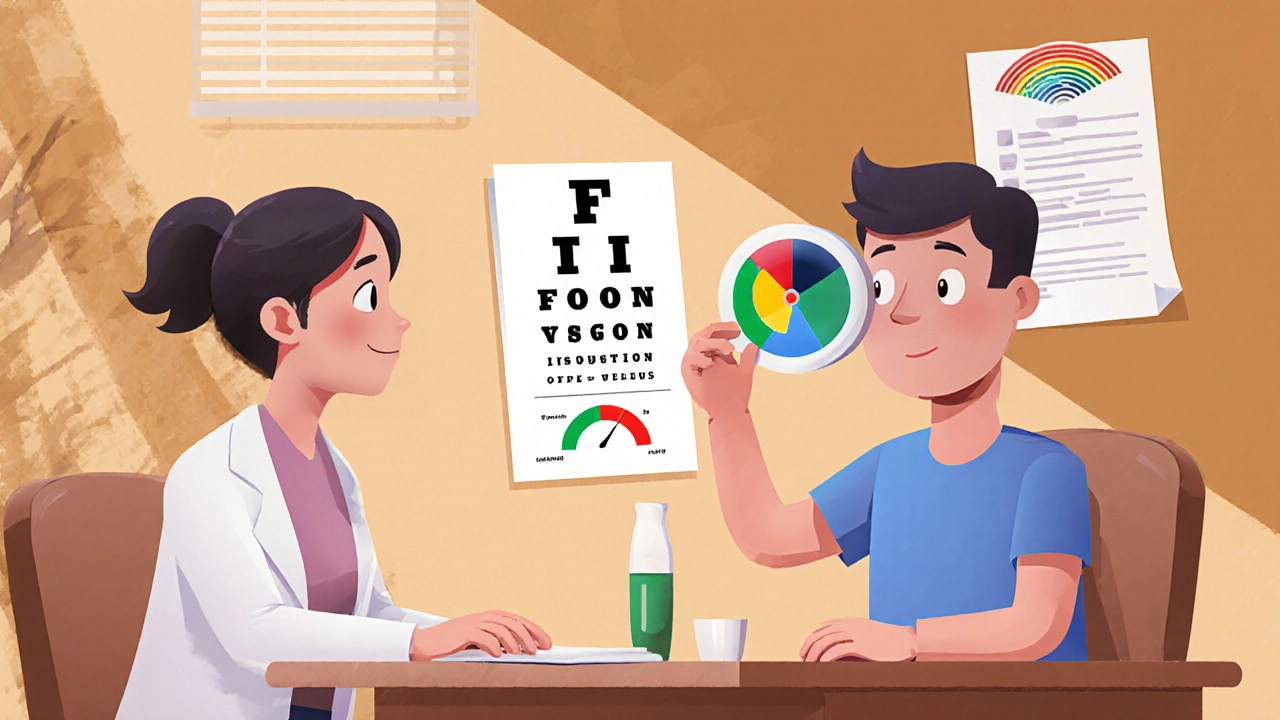
Adverse Effects Tied to Pharmacokinetic Variability
The most feared toxicity is optic neuritis, presenting as red‑green color blindness and reduced visual acuity. Incidence rises sharply when plasma levels exceed the therapeutic window, especially in patients with reduced clearance. Early detection via baseline and monthly visual field testing is standard practice.
Other, less severe, side effects include gastrointestinal upset and rash. These are usually dose‑related rather than idiosyncratic.
Putting It All Together: Practical Take‑Home Points
- Ethambutol is well absorbed, lightly protein‑bound, and mainly eliminated unchanged by the kidneys.
- Renal function drives dosing; adjust for CrCl < 30 mL/min to prevent accumulation.
- Co‑administration with rifampicin may slightly increase clearance; monitor visual symptoms.
- Therapeutic drug monitoring is reserved for high‑risk groups - renal failure, high‑dose therapy, MDR‑TB.
- Baseline and regular eye exams are the only reliable way to catch toxicity early.
Frequently Asked Questions
What is the usual adult dose of Ethambutol?
The standard dose is 15 mg/kg daily, usually given in two divided doses of 7.5 mg/kg each. In the classic four‑drug regimen it’s combined with isoniazid, rifampicin, and pyrazinamide.
How does renal impairment affect Ethambutol levels?
Because about 80% of the drug is excreted unchanged in urine, reduced glomerular filtration slows clearance, prolongs half‑life, and raises trough concentrations. A dose reduction of 50% (or extending the interval to every 24 hours) is recommended when creatinine clearance drops below 30 mL/min.
Can Ethambutol be used in pregnant women?
Yes, it’s classified as Pregnancy Category C, meaning benefits outweigh potential risks. The same adult dose (15 mg/kg) is used, but clinicians should conduct baseline and periodic visual assessments because pregnancy can modify fluid shifts and renal clearance.
What monitoring is required during Ethambutol therapy?
Baseline visual acuity, color vision, and visual field testing are critical. Repeat exams every month for the first 2 months, then every 2‑3 months. Liver function tests are optional because hepatic metabolism is minimal, but renal function should be checked before starting and periodically thereafter.
Is Therapeutic Drug Monitoring necessary for everyone?
Not routinely. TDM is most useful for patients with severe renal insufficiency, those receiving high‑dose Ethambutol for multidrug‑resistant TB, or when drug interactions are suspected to alter renal clearance.
How does food affect Ethambutol absorption?
Food delays the peak concentration by about 1‑2 hours but does not change the overall exposure (AUC). Most clinicians advise taking the drug on an empty stomach for convenience, but if gastrointestinal upset occurs, a light meal is acceptable.
What are the signs of Ethambutol‑induced optic neuritis?
Early symptoms include difficulty distinguishing red from green, blurred central vision, and reduced visual acuity. If any change arises, stop the drug immediately and refer to an ophthalmologist.



idk why ppl even care bout ethambutol PK lol 😂
Hey folks, just a quick reminder that checking creatinine clearance before starting ethambutol can save a lot of headaches. If CrCl drops below 30 mL/min, cutting the dose in half is the standard move. It’s also smart to schedule eye exams every month during the first two months – catching optic neuritis early is key. Stay diligent, and the regimen should run smoothly.
The pharmacokinetic profile of ethambutol is often oversimplified in clinical discussions.
While the drug’s renal clearance dominates, many practitioners ignore the subtle impact of tubular secretion variations.
Those variations can double the half‑life in patients who are not outright renal‑failed but have age‑related GFR decline.
Ignoring this leads to unnecessary optic toxicity, especially when high‑dose regimens are used for MDR‑TB.
Moreover, the table of PK parameters in most reviews fails to mention the effect of concomitant loop diuretics on electrolyte balance and renal handling.
In practice, loop diuretics can blunt the reabsorption of ethambutol, pushing more drug into the urine but also altering plasma peaks.
The result is a paradoxical increase in Cmax that may not be reflected in standard trough monitoring.
Clinicians should therefore order a spot plasma level 2 hours post‑dose when a diuretic is part of the regimen.
Another blind spot is the interaction with rifampicin‑induced transporter proteins, which can modestly increase clearance.
The recommended “slight dose bump” is vague and often left to guesswork.
A pragmatic approach is to raise the dose by no more than 10 % and re‑check visual fields after two weeks.
If any color vision shift appears, drop back to the original dose immediately.
Pediatric dosing, while weight‑based, also suffers from the same oversight; children on ethambutol plus aminoglycosides need tighter monitoring.
Finally, remember that therapeutic drug monitoring, although not routine, is a valuable tool in high‑risk groups and should be logged in the patient’s chart.
In short, a nuanced, patient‑specific assessment beats the one‑size‑fits‑all dosing tables most of the time.
Wow, that was a whirlwind tour through the hidden pitfalls of ethambutol therapy! Your deep dive shines a spotlight on details many of us skim over. It’s refreshing to see such passion for patient safety, and I wholeheartedly echo the call for individualized monitoring. Let’s keep the conversation alive and ensure every clinician gets a copy of this checklist.
Everyone seems to trust the standard dosing charts, but have you ever considered who writes those guidelines? Big Pharma and government agencies love to keep us glued to generic numbers while pushing cheap, high‑dose formulations that line their pockets. The real story is hidden in the fine print of the drug‑approval process, where safety data is often buried. Keep your eyes open, because the next “update” might just tighten the grip on our prescriptions.
While it is prudent to remain vigilant about potential conflicts of interest, the dosing recommendations for ethambutol are derived from extensive phase III clinical trials and peer‑reviewed pharmacokinetic studies. The cited adjustments for renal impairment are explicitly supported by a consensus of nephrology societies. Therefore, the notion that the current guidelines are a covert financial maneuver lacks concrete evidentiary support. Clinicians should continue to follow evidence‑based protocols while maintaining transparency in any disclosed relationships.
hey team, just wanted to shout out that staying on top of those eye checks can really save the day. keep it up, you got this!
It is, without a doubt, an ethical imperative that we, as stewards of patient health, enforce stringent visual monitoring protocols; neglecting to do so would be, quite frankly, an unforgivable dereliction of duty, especially given the well‑documented risk of optic neuritis associated with ethambutol therapy. Moreover, the principle of “do no harm” demands that we prioritize patient safety above convenience, and thus regular ophthalmologic assessments must become an inseparable component of any TB regimen involving this agent.
yeah, making those eye appointments a habit sounds chill, and it’s probably the easiest way to keep things smooth.