Ethambutol absorption – what you need to know
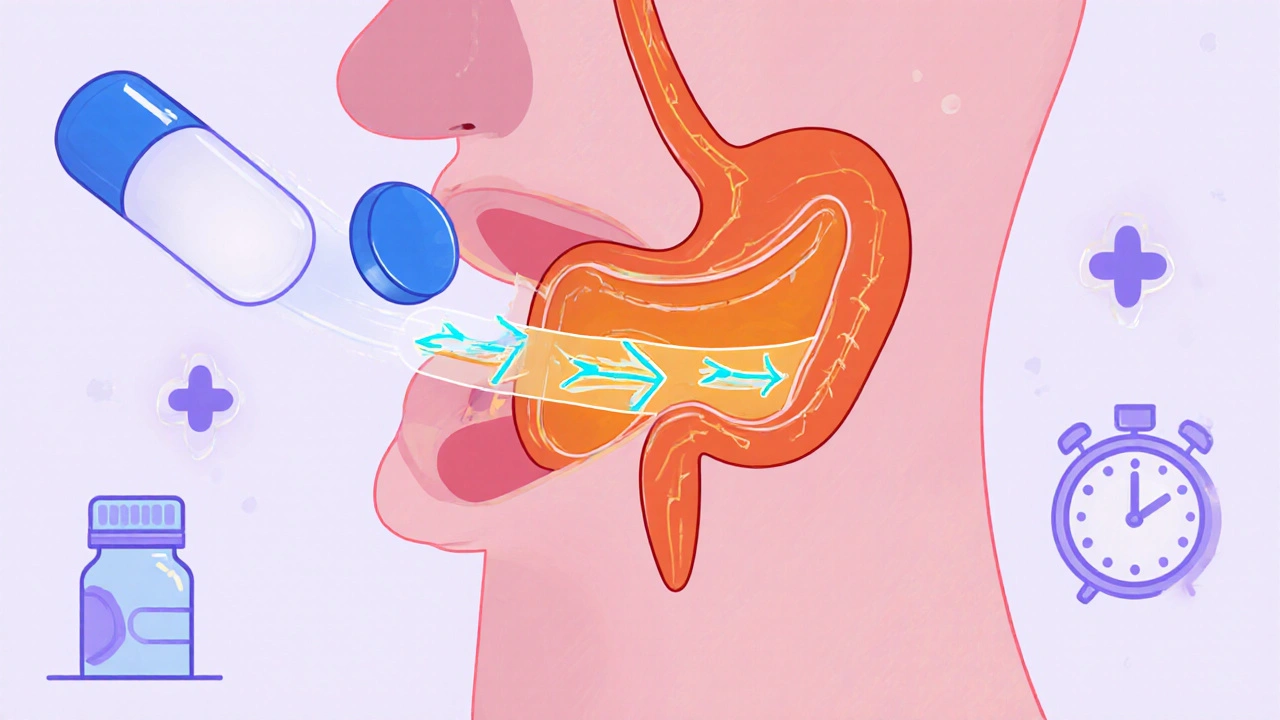
When working with ethambutol absorption, the process by which the anti‑TB drug ethambutol enters the bloodstream after oral intake. Also known as ethambutol bioavailability, it determines how much of the dose becomes available to fight Mycobacterium tuberculosis. In the same breath, ethambutol, a first‑line medication used in combination therapy for active tuberculosis relies on drug absorption, the movement of a drug from the gut lumen into systemic circulation and the resulting bioavailability, the fraction of an administered dose that reaches systemic circulation in an active form. Understanding these concepts helps clinicians optimize dosing, avoid sub‑therapeutic levels, and reduce resistance risk.
Key factors that affect ethambutol absorption
First, the gastrointestinal environment matters. Ethambutol is a weakly basic compound, so an acidic stomach pH favors its dissolution. When patients take antacids or proton‑pump inhibitors, the higher pH can slow dissolution, leading to lower peak concentrations. Second, food intake plays a role; a high‑fat meal may delay gastric emptying, modestly reducing the rate but not the total amount absorbed. Third, transporter proteins such as organic anion transporting polypeptides (OATPs) can facilitate ethambutol uptake in the intestinal epithelium. Genetic variations or concurrent drugs that inhibit these transporters—like certain macrolide antibiotics—can blunt absorption. Finally, renal function indirectly influences apparent absorption because ethambutol is cleared unchanged; impaired kidneys raise plasma levels, which may be misinterpreted as increased absorption.
Clinical guidelines tie these factors together in a simple rule: give ethambutol on an empty stomach whenever possible, separate it from acid‑reducing agents by at least two hours, and monitor serum levels in patients with compromised kidney function. This approach aligns with the broader principle that drug absorption requires proper timing and awareness of interacting substances. Studies show that adherence to these timing recommendations improves treatment success rates for multidrug‑resistant TB regimens. Moreover, the same principles apply to other anti‑TB drugs—like isoniazid and rifampin—so the knowledge extends beyond a single molecule.
Beyond pharmacokinetics, adverse effects are linked to absorption patterns. High systemic exposure can increase the risk of optic neuritis, the most serious ethambutol side effect, while low exposure may lead to treatment failure and resistance. Detecting early visual changes and adjusting the dose based on renal function are practical steps clinicians can take. For patients on combination therapy, be aware that some drugs (e.g., pyridoxine for isoniazid‑induced neuropathy) do not interfere with ethambutol absorption, while others (e.g., fluoroquinolones) may compete for the same transport pathways. Understanding these relationships helps build a safer, more effective TB regimen.
The collection below brings together detailed articles on ethambutol absorption, related pharmacokinetic topics, and practical management tips. Whether you’re looking for guidance on food interactions, transporter genetics, or monitoring strategies, you’ll find concise, evidence‑based information to support your clinical decisions.
Ethambutol Pharmacokinetics Explained: Absorption, Distribution, Metabolism, Elimination
A clear, practical guide to Ethambutol pharmacokinetics covering absorption, distribution, metabolism, excretion, dosing tweaks, interactions, and safety monitoring.
View more