 25
Apr,2025
25
Apr,2025
Understanding the Surge in Amoxicillin Resistance
So, here’s the reality check: We once leaned hard on amoxicillin for everything from ear infections to sinusitis. Now, a growing number of bugs are just shrugging it off. In the past decade, resistance rates in common pathogens like Streptococcus pneumoniae and H. influenzae have shot up, especially in spots with high antibiotic use—think busy city clinics and crowded households. In Australia, recent data flagged resistance rates over 20% in some respiratory tract pathogens. This means one in five patients could walk out with a script that stands little chance of working. Makes you think twice about fallback plans, right?
The problem doesn’t stop at underwhelming recoveries. Failed treatment means longer sickness, higher risks of complications, and the potential for these resilient bugs to invite their friends. Hospitals worldwide are clocking more admissions for everyday infections simply because first-line drugs like amoxicillin keep striking out. For patients, it can mean more time off work and, honestly, more frustration. Clinicians—even those outside infectious diseases—are now re-jigging their mental lists of go-to antibiotics. Time to get serious about beta-lactam-sparing options.
Why is this happening? Amoxicillin resistance boils down to overuse and incomplete courses. Bacteria are smart: they adapt, pass survival tricks to their mates, and multiply. That’s where things get dicey. When a GP or ED doc prescribes amoxicillin for a suspected infection that happens to be viral, it basically gives bacteria target practice to get even tougher. Eventually, those bacteria become the new normal, and our hands get tied. Surveillance programs, both global and in Australia, keep sounding the alarm—resistant bugs are climbing fast, especially after the pandemic when antibiotic use spiked in the community due to telehealth habits.
Now, not every resistant infection is a medical emergency, but each one chips away at our arsenal. For context, Macquarie University’s 2023 surveillance noted a 15% jump in amoxicillin-resistant urinary E. coli. That’s not some far-off theory, that’s right in our own backyard. The ripple effect is huge: more hospital visits, more IV antibiotics, and more side effects for patients. For GPs and other prescribers, it’s pressure to stay nimble without reaching into the big-gun antibiotics on every visit. If you’re treating patients or you’ve danced with repeat infections yourself, this stuff matters—big time. So, let’s talk about actual alternatives that work in the trenches, beyond amox.
Beta-Lactam-Sparing Antibiotics: Why, When, and How?
Once amoxicillin is off the table, it’s not just about grabbing the next available option. The whole point of beta-lactam-sparing antibiotics is to dodge cross-resistance and limit toxic fallout—because not all antibiotics play nice with every patient or bug. What does that mean? Infections like community-acquired pneumonia, complicated UTIs, and resistant skin infections often make life difficult for former favourite drugs. This is why alternative classes have earned a spot in Aussie prescribing guidelines and hospital protocols. The right choice depends on a bunch of factors: infection site, bug likelihood, patient kidney function, allergies, your local resistance map, and, of course, cost or PBS availability.
First up, macrolides like azithromycin and clarithromycin. GPs love these for their simple dosing and strong reach against respiratory bacteria. Unlike amoxicillin, macrolides can handle not just bacteria, but also some atypicals—making them a must-have for community-acquired pneumonia, especially in smokers or the elderly. But watch out: macrolide resistance emerged too, especially in the eastern states. Make sure you know your patient’s history and check the latest state health bulletins—resistance can swing wildly between suburbs and hospitals.
Then there are the tetracyclines, with doxycycline the reigning champ. It knocks out a wide range of bugs, from acne-causing nasties to walking pneumonia, and it’s super simple to take—one pill with food and you’re sorted. It’s got a good long half-life and doesn’t mess too much with your gut. Still, not for kids under 8 or pregnant folks, because of risks to teeth and bones. Not everything suits everyone, which is why running through allergies and drug history makes all the difference.
Sulfa drugs, particularly trimethoprim-sulfamethoxazole (say that three times fast), have a bad rep with some for allergies, but can be absolute lifesavers for UTIs and certain skin infections. These are especially handy when E. coli isn’t playing fair with beta-lactams. Tip: always check renal function, as these drugs won’t forgive much if the kidneys are sluggish. People on blood thinners need extra caution here too—the side effect list can be longer than your shopping receipt, but for straightforward infections, TMP-SMX often hits the mark.
Fluoroquinolones—so, ciprofloxacin, norfloxacin, and the like—are the real heavy lifters for tough urinary or prostate infections. They cut deep, but their Achilles’ heel is tendon trouble and a range of neuropsychiatric side effects. You don’t want to give these out for a sore throat but, for certain infections, they’ve bailed out patients when all else failed. Pro tip: always warn your patients not to hit the gym hard for a bit after starting these—Achilles tears are no joke, especially in older adults.
For some tricky cases, like multi-resistant skin wounds or hospital exposures, lincosamides like clindamycin, or even glycopeptides such as vancomycin, come into focus. These are seldom first choice outside the hospital, but they’re a lifeline for MRSA or stubborn gram-positive infections. Side note: clindamycin can mess with gut flora and trigger C. difficile colitis—always counsel on diarrhoea red flags.
Some folks do well with nitrofurantoin for UTIs, especially young women with healthy kidneys. Nitro’s whole trick is that it concentrates in urine, so it’s useless for most other infections, but a total star for bladder bugs even when first-lines flop. If UTIs keep boomeranging back, and amoxi fails, this option deserves attention—especially given its low impact on gut flora and relatively mild resistance rates here in Australia.

Top 10 Alternatives to Amoxicillin: When Each Shines
Navigating all these choices can make your head spin. Here's a breakdown, so you know what works best, and when:
- Azithromycin: Perfect when a simple sinus or chest infection needs quick, short-course punch. Great for travel, since it’s once-daily and packs small. Not so handy for serious hospital bugs, but super reliable for community-acquired pneumonia, pharyngitis, and skin infections (when strep isn’t the only player).
- Clarithromycin: A sibling of azithro, works well for upper and lower respiratory bugs—especially if you suspect more exotic bacteria like Mycoplasma. More drug interactions than azithro, so always check patient’s other meds.
- Doxycycline: Rising in popularity for everything from bronchitis to skin abscesses, and even for things like chlamydia. No dose adjustments for mild-moderate kidney issues. Cheap and easily accessible on PBS, which matters for monthly scripts.
- Trimethoprim-sulfamethoxazole (TMP-SMX): The UTI-specialist, but also one to consider for skin and soft tissue infections, especially if MRSA is a worry. Sensitive patients will need to watch for rash or a funny taste in the mouth, and keep hydrated.
- Ciprofloxacin: Best for older boys with stubborn prostate or pyelonephritis issues, not your go-to for basic UTI. Fast-acting and available in both oral and IV—handy from city clinics to outback hospitals. Serious side effects, so keep the use short and targeted.
- Nitrofurantoin: The UTI maven for uncomplicated, community-acquired bladder infections. Easy dosing, minimal resistance locally, and safe for long-term use in specific cases (post-menopausal women, recurrent infections) with regular renal checks.
- Clindamycin: When skin or soft tissue abscesses don’t melt with standard drugs, this one covers most gram-positives, even MRSA. Not for the faint-hearted—watch gut health closely and educate patients on diarrhoea as an urgent warning sign.
- Vancomycin: Usually kept for the sickest patients in hospital, battling MRSA and enterococci in blood or joints. Needs regular blood level monitoring, but if you’re fighting for a limb, it’s on your team.
- Fosfomycin: Single-dose magic for female lower UTIs, especially when everything else fails or allergies rule out other options. It’s in powder form here in Australia and can reduce the rattle of daily pills.
- Linezolid: Reserved for nastier, multi-resistant staph or enterococcal infections. Expensive, but real-world life-saver in the right hands. GPs usually coordinate with infectious disease specialists for this one, especially to monitor for side-effects like bone marrow suppression.
You’ll notice the choices above run the spectrum—from oral options for everyday fixes to harsh IV drugs reserved for hospital battlegrounds. The key is knowing when to escalate. If your local antibiogram (yes, every hospital has one!) shows high resistance to one class, jump to the next, but don’t just cycle randomly. Each decision should hinge on bug, site, patient allergies, and logistics. By the way, for a more detailed breakdown and charts of the top alternatives, check out alternatives to Amoxicillin for in-depth prescribing pearls for both GPs and patients.
| Antibiotic | Main Infection Targets | Common Side Effects | Best Use Setting |
|---|---|---|---|
| Azithromycin | Respiratory, skin, STIs | Nausea, QT prolongation | Outpatient/GP clinic |
| Doxycycline | Lung, skin, acne, STIs | Photosensitivity, GI upset | Both GP and hospital |
| Clindamycin | Skin, abscess, bone | Diarrhoea, C.diff colitis | GP (selected), hospital |
| Ciprofloxacin | Prostate, complicated UTI | Tendinopathy, confusion | Hospital/informed outpatient |
| Nitrofurantoin | Lower UTI | Nausea, rare lung effects | GP outpatient |
Practical Tips and Pitfalls: Choosing the Right Alternative
There are some things textbooks just don’t say out loud. For starters: always grab a recent culture if the infection has failed amoxicillin or keeps coming back. Yes, even if it means waiting a day for the lab—random guessing is what got us into this mess. If you live in Melbourne or Sydney, you know some areas swap advice on WhatsApp or pharmacy groups—keep an ear to the ground for local resistance spikes. It might sound old school, but actual phone calls to local pathology can give you up-to-the-hour updates on current outbreaks or quirky strains causing trouble. In fact, Melbourne’s western suburbs saw a run-in with highly resistant E. coli last year that quietly shut down some first-line scripts.
When switching drugs, interactions matter. For instance, clarithromycin bumps up levels of common heart medications or statins—it’s not a trivial thing for older patients juggling half a dozen pills. If you’re using fluoroquinolones, warn about sun sensitivity and keep a lookout for confusion in the elderly. These details matter, especially as Australia’s population ages and polypharmacy is the new normal. Keep an eye on simple stuff too: doxycycline with food lowers gut upset but can cut strength a bit—balance matters. Some drugs can mess with contraception, heighten risks on blood thinners, or even tick off a rash after a glass of wine (like metronidazole).
It’s tempting to go big when a bug breaks the rules, but hold back on the heavy guns if it’s a simple, non-severe infection. Save vancomycin, linezolid, and carbapenems for clear cases of hospital-acquired or multi-resistant bugs—they’re not for a Tuesday cold or a GP’s first pass at a suspected UTI. The more we use those last-resort antibiotics in the community, the less effective they’ll be when we really need them for sepsis or immunocompromised patients. Australia, funnily enough, still gets new antibiotic launches far behind Europe, so burn through your shelves sparingly.
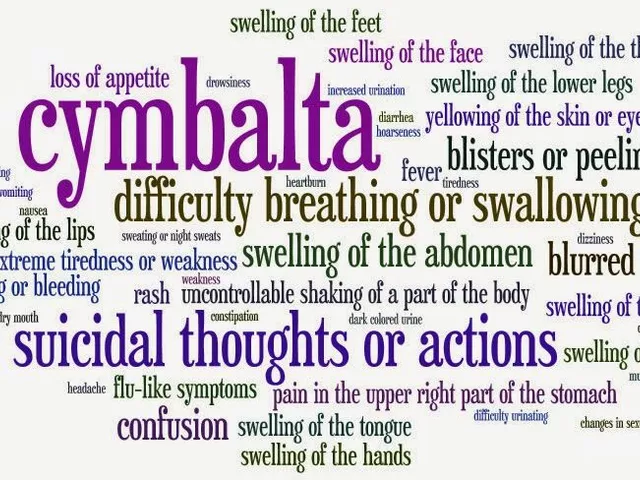
Remember patient allergies and preferences. Anyone with a history of anaphylaxis to penicillins can react to cephalosporins or carbapenems, even if the risk is low. Chat openly about it—reactions can spiral quickly and ruin a GP’s week, not to mention the patient’s year. Tip: have patients write down or snap a pic of all old antibiotic scripts, so they’re not guessing allergies from memory. And explain red-flag symptoms: rash, facial swelling, sudden abdo pain, dark urine—don’t mess about, straight to ED if these show up.
Last but not least, follow up. Resistant bugs love to play hide-and-seek, and your first choice, no matter how well researched, might strike out. Give patients a plan: when to call back, when to go to hospital, what symptoms to watch for. Not only does it keep them safe, but it gives you a better shot at seeing patterns early—could be the sign of a wider resistance problem in your clinic, practice, or suburb. Use paper, apps, group messages—whatever works to keep track and spot trouble before everyone else is chasing their tails.
Pushing back against antibiotic resistance isn’t glamorous, but getting it right matters, especially when amoxicillin doesn’t stand a chance. The new playbook covers everything from macrolides and tetracyclines to more niche options, each with its perfect use case and odd pitfall. Keep it practical, stay curious, and when in doubt, call an ID mate or check your latest local antibiogram—next week, it could all shift again.





This is such an important topic, especially nowadays when antibiotic resistance is becoming a serious concern worldwide. The guide’s emphasis on beta-lactam-sparing options is refreshing because it reminds us that relying solely on amoxicillin isn't the best practice anymore.
From a clinical perspective, it’s critical that both patients and providers see these alternatives as viable and understand when each one is appropriate. It’d be really helpful if the guide also mentioned the role of culture and sensitivity testing in guiding these antibiotic choices, no?
Also, does anyone know if these alternatives have the same side effect profile or if we should be cautious with certain patient populations? I’ve seen some cases where renal function affects antibiotic choice, for instance.
Looking forward to you all sharing your experiences with these drugs. It’s crucial that articles like this keep the conversation alive with practical insights rather than just textbook explanations.
What a timely and well-constructed topic!
Antibiotic resistance really challenges our traditional treatment paradigms. It's fascinating how these beta-lactam-sparing antibiotics not only expand our arsenal but also encourage judicious use of certain classes, helping to preserve their efficacy long-term.
I appreciate the article’s practical approach; theory alone rarely influences clinical decision-making effectively. The input from specialists, as mentioned, cannot be overstated. Infectious disease experts bring insights that help tailor treatments for complex cases.
One angle worth considering is the global disparity in access to these alternatives. What’s readily available and affordable in one region could be a luxury in another.
Let’s keep this discussion going. What are your thoughts on the balance between guideline-directed therapy and individualized patient needs?
Oh, great, yet another '10 best alternatives' list—I was prepared for some overhyped hype, but I have to say, this actually delivers on the promise of being practical instead of just fluff.
Though, I’m curious if the guide addresses the common pitfalls many clinicians encounter when switching from amoxicillin, like underestimating drug interactions or the impact on gut flora.
It could also do with some deeper dives into when NOT to use these alternatives, because every antibiotic has a dark side and risks of secondary infections or resistance.
Still, the snippet about specialist input being a game changer is dead on. Sometimes it feels like GPs get stuck in a rut thinking they've got to push through with amoxicillin no matter what.
Does anyone here regularly consult with specialists for these cases, or do you mostly wing it with guidelines?
Alright, let me just throw some shade because honestly, ‘best alternatives’ always sounds so grand but then you open the list and it’s the same tired options that have been trotted out for years.
If you want my take, the whole beta-lactam-sparing idea is probably a stopgap to mask the pharmaceutical industry's slow progress on truly novel antibiotics.
That said, I didn’t hate the guide entirely because it was practical and not drowning in jargon—which is rare.
But, really, what’s going to change if clinicians just swap one drug for another without addressing the root problem of antibiotic misuse and overprescribing?
Rhetorical, I know, but come on. We need real innovation, not just repackaged old news.
I actually found this guide super motivating! It’s easy to get overwhelmed with all the antibiotic resistance news, but having a clear layout of alternatives makes it feel like there’s hope and tools at hand.
One thing I’d love to see in future updates is patient-friendly explanations because not everyone gets the medical lingo, and that kind of education empowers patients to ask the right questions.
For those of you who’ve dealt with resistant infections, how do you help your patients understand why amoxicillin might no longer be their best bet?
Sharing those narratives could be invaluable for building trust and compliance.
Also, the emphasis on specialist input is key—teamwork saves the day in complicated cases!
Look, I get that alternatives are necessary and all, but aren’t we just prolonging the inevitable? Pathogens evolve faster than we can whip up new drugs or alternatives.
It’s like a never-ending soap opera where we’re the doomed heroes making temporary fixes.
The guide is thorough, sure, but I wonder how many clinicians really follow through with these options, or if they just default to what they know, because hey, less resistance to change, right?
There’s gotta be a better way to tackle this plague of resistance than just swapping antibiotics.
What’s everyone’s take on this cycle? Over-treatment, under-treatment, rinse and repeat?
I find this discussion quite meaningful, especially since antibiotic stewardship is crucial not just for individual patient outcomes but for public health.
One point I’d highlight is the importance of precision in documentation when switching from amoxicillin to these alternatives. Errors or miscommunications can cause bigger headaches down the line.
Has anyone noticed improvements in clinical workflows after integrating such alternatives into practice? How do your electronic health systems support or hinder that?
Also, the guide could expand on follow-up protocols post-prescription to monitor effectiveness and adverse effects.
Ensuring a loop of feedback optimizes treatment and enhances our overall understanding of resistance patterns.
Honestly, the way people blindly trust these so-called ‘alternatives’ without a shred of skepticism is wild to me.
Resistance isn’t just a hiccup; it’s a symptom of systemic failure in overprescribing and complacency in healthcare systems, especially in our country.
Most alternatives listed are just variations on the same mechanisms, so resistance will catch up—mark my words.
We need not only new drugs but also ruthless accountability and public education on not demanding antibiotics for every sniffle.
I appreciate the guide’s practical nature but feel it misses the bigger picture: the sociopolitical factors fueling this crisis.
Okay, here’s a thought: what if the pharmaceutical industry is just using these beta-lactam-sparing antibiotics to keep us hooked on expensive cycles of meds? Ever think about that?
The guide’s practical approach is nice, sure, but who certifies that the alternatives aren’t just a shiny distraction from more radical solutions like phage therapy or immunomodulation?
Plus, I’d be interested in seeing if these alternatives are really vetted across all demographics or mostly studied on typical Western samples.
Antibiotic resistance could be a gold mine for some—and a nightmare for us, the unsuspecting patients.
hey, big fan of how the guide simplified such a complex issue without dumbing it down.
like, i’m not a doc, but even a layperson can grasp the urgency behind amoxicillin resistance and why alternatives matter.
also appreciate the casual tone mixed with solid info. makes learning less painful lol.
wonder if the alternatives come with different dosing regimens because that can make or break adherence for patients.
any thoughts from the clinicians here about patient compliance when switching antibiotics?
Man, this read was longer than the wait at my last doc appointment, but honestly, that was a good thing because it’s dense with info.
I’m thrilled to see topics like this getting attention because so many folks don’t realize that amoxicillin isn’t a magic bullet anymore.
That said, I would have liked some more engaging real-world examples or case studies to break up the technical bits.
Still, great resource and a wake-up call to all us weekend warriors trying to self-medicate or push docs for the same prescription every time we’re sick.
Cheers for the fresh perspective!