 23
Nov,2025
23
Nov,2025
When your feet feel like they’re on fire, or your hands go numb for no reason, it’s not just aging-it could be peripheral neuropathy. This isn’t a single disease but a group of conditions caused by damage to the nerves outside your brain and spinal cord. These nerves control sensation, movement, and even automatic functions like digestion. When they’re damaged, you don’t just feel pain-you lose balance, struggle to walk, and sometimes can’t even tell if you’ve stepped on something sharp.
What Causes Peripheral Neuropathy?
The most common cause by far is diabetes. About half of all people with diabetes develop some form of nerve damage over time. High blood sugar slowly poisons the nerves, especially in the feet and legs. Keeping your HbA1c below 7% cuts your risk of developing neuropathy by 60%, according to long-term studies like the Diabetes Control and Complications Trial. But diabetes isn’t the only culprit.Vitamin Deficiencies
Vitamin B12 deficiency is responsible for about 8% of cases. This isn’t just about being vegetarian-older adults, people on acid reflux meds like proton pump inhibitors, and those with gut absorption issues are at risk. Without enough B12, nerves lose their protective coating. Symptoms can start subtly: tingling fingers, a feeling of walking on cotton. A simple blood test can catch this early, and treatment with monthly B12 injections often reverses symptoms within weeks.Chemotherapy and Toxins
About one in three cancer patients on chemo drugs like vincristine or paclitaxel will develop neuropathy. It’s called chemotherapy-induced peripheral neuropathy (CIPN). Numbness in the hands and feet is common, and sometimes it doesn’t go away after treatment ends. Alcohol abuse is another major cause-chronic heavy drinking damages nerves directly and often comes with poor nutrition, making things worse.Autoimmune Disorders and Infections
Conditions like lupus, rheumatoid arthritis, and Guillain-Barré syndrome can attack nerves. Even infections like Lyme disease, shingles, or HIV can trigger nerve damage. In some cases, the body’s own immune system gets confused and starts damaging nerves, thinking they’re foreign invaders.Idiopathic Neuropathy
About 20% of cases have no clear cause, even after full testing. Doctors call this idiopathic neuropathy. It’s frustrating-not because it’s untreatable, but because you can’t target the root. Still, pain can be managed, and progression slowed.How Do You Know It’s Neuropathy?
Symptoms usually start in the toes or fingertips and creep upward. You might feel:- Sharp, stabbing, or burning pain
- Tingling or a "pins and needles" feeling
- Numbness that makes you lose balance
- Extreme sensitivity to light touch-even sheets feeling painful
- Muscle weakness or cramps
Pain Management: What Actually Works
Pain from neuropathy doesn’t respond well to regular painkillers like ibuprofen. They might help 10-15% of the time. What does work? Here’s what the evidence shows.Medications That Help
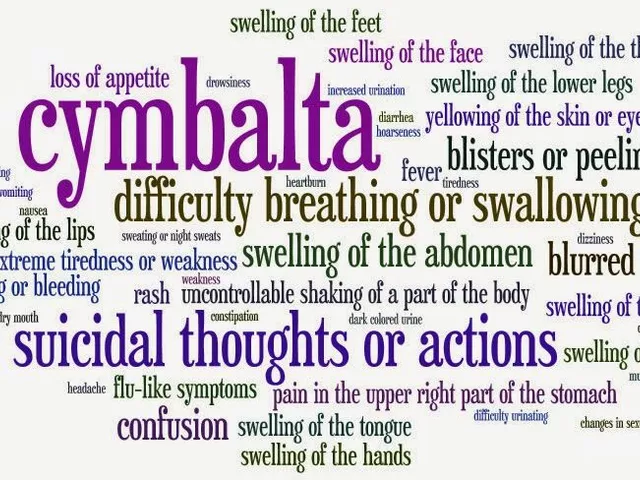
- Pregabalin (Lyrica): Reduces pain by 50% in about 37% of users. Side effects? Dizziness and weight gain. Many people stop because they feel "drugged." - Duloxetine (Cymbalta): Works in 35% of people. Helps with both pain and depression, which often comes with chronic pain. But nausea hits hard for some-up to 30% quit within weeks. - Amitriptyline: An old antidepressant that’s surprisingly effective. 41% get 50% pain relief. But dry mouth affects 75%, drowsiness 60%. Best taken at night. The American Academy of Neurology rates pregabalin and duloxetine as "Level A" evidence-the strongest recommendation. Amitriptyline is "Level B," still useful but with more side effects.Non-Drug Treatments That Deliver Results
- Scrambler Therapy: A machine sends mild electrical signals to "trick" the brain into not feeling pain. After 10 sessions, 85% of patients report 50% pain reduction. It’s not covered by all insurance, but it works where meds fail. - Spinal Cord Stimulation: A tiny device implanted near the spine sends pulses to block pain signals. Works in 65% of severe, long-term cases. Used when nothing else helps. - Qutenza Patch: A high-dose capsaicin patch applied in a doctor’s office. One 30-minute treatment can give relief for up to 3 months. It burns during application-like chili pepper on nerves-but the pain fades fast after.Physical Therapy and Daily Habits
Balance training is critical. People with neuropathy are 3 times more likely to fall. A 12-week physical therapy program focusing on leg strength and balance improves "up and go" test times by 25%. That means fewer trips to the ER from falls. Daily foot checks are non-negotiable. Look for cuts, blisters, or redness-twice a day. You might not feel them, but infection can spread fast. Wear therapeutic shoes with custom orthotics. Studies show 82% of users report less pain and better stability.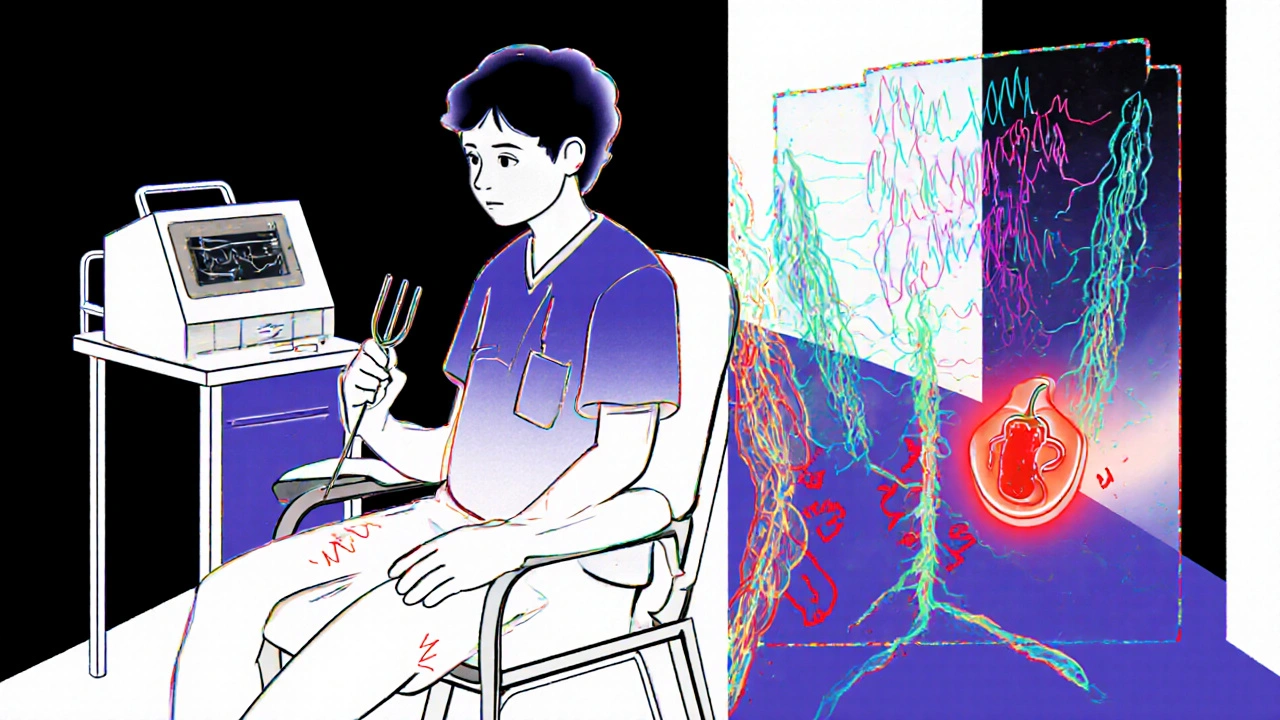
What Doesn’t Work (And Why)
Opioids are a trap. They reduce neuropathic pain in only 30% of cases, and addiction rates hit 15% with long-term use. The American Diabetes Association and Harvard Medical School both warn against them. They don’t fix the nerve damage-they just mask the pain while risking dependence. Over-the-counter creams with lidocaine or capsaicin? They offer minor, short-term relief for some. But they won’t change the course of the disease.Real People, Real Stories
On Reddit’s r/neuropathy, users share what works and what doesn’t. One person, u/SarahJ72, says Lyrica dropped her foot pain from 8/10 to 3/10-but she couldn’t drive for two weeks because of dizziness. Another, u/DaveM45, tried Cymbalta but quit after two weeks: "My doctor didn’t warn me about the nausea." Physical therapy gets 4.2 out of 5 stars from over 1,800 reviews. Custom orthotics? 82% satisfaction. But meds? Only 3.5 out of 5, mostly because side effects make people quit.
What You Can Do Today
If you have diabetes: Get your HbA1c checked. If it’s above 7%, work with your doctor to bring it down. Even a 1% drop reduces nerve damage risk. If you’re numb or tingling: Don’t wait. See a neurologist. The average time to diagnosis is 18 months-and early treatment improves outcomes by 40%. Start foot checks. Buy supportive shoes. Try a 10-minute balance exercise daily-stand on one foot while holding the counter. Do it twice a day. If you’re on chemo: Ask your oncologist about nerve-sparing drug options or preventive supplements like alpha-lipoic acid (studies show mixed results, but low risk).The Future Is Getting Brighter
Research is moving fast. The FDA approved Qutenza in 2020. The "Neuropathy Genomics Project" launched in 2023 to find genetic causes of 50+ types by 2026. Wearable nerve stimulators are in trials and could hit the market in 2024. AI tools are being trained to spot early nerve damage from simple foot scans-cutting diagnosis time from 18 months to under 6 months by 2025. Combination therapies targeting both pain and nerve repair are expected to become standard by 2030.Final Thoughts
Peripheral neuropathy isn’t a death sentence. It’s a signal-your body is telling you something’s wrong. Whether it’s high blood sugar, a vitamin gap, or something else, fixing the cause matters more than just treating the pain. And even when the cause isn’t clear, you still have options: physical therapy, targeted devices, and smart medication choices. You don’t have to live with burning feet or constant numbness. The tools to help you are here. The key is acting early, staying consistent, and refusing to accept pain as normal.Can peripheral neuropathy be reversed?
Yes, in some cases. If the cause is treatable-like vitamin B12 deficiency, hypothyroidism, or early-stage diabetes-nerve damage can improve or even reverse with proper treatment. For example, B12 injections often restore sensation within 4 to 8 weeks. But if damage is long-standing, especially from uncontrolled diabetes or chemo, nerves may not fully heal. The goal then shifts to stopping further damage and managing symptoms.
Is peripheral neuropathy the same as carpal tunnel?
No. Carpal tunnel is a type of mononeuropathy-it affects just one nerve, the median nerve in the wrist. Peripheral neuropathy usually means damage to many nerves, often symmetrically in both feet and hands. Carpal tunnel causes numbness mostly in the thumb, index, and middle fingers. Peripheral neuropathy affects the whole foot or hand, often starting in the toes or fingertips. Both are nerve issues, but the scope and cause are different.
Why do my symptoms get worse at night?
At night, your body is still, and distractions fade. With less movement and fewer sensory inputs, your brain focuses more on the abnormal nerve signals. Also, cortisol (a stress hormone that helps dampen pain) drops at night. Some people find their pain spikes because of changes in body temperature or even because their feet are covered in bed sheets, which can irritate hypersensitive nerves.
Can I still drive with peripheral neuropathy?
It depends. If you have severe numbness in your feet, you might not feel the gas or brake pedal properly. Dizziness from medications like pregabalin can also affect reaction time. Many people with mild neuropathy drive safely with proper footwear and regular foot checks. But if you’ve had near-misses or can’t tell if your foot is on the pedal, get evaluated. Some states require a medical review for drivers with neuropathy.
What’s the best shoe for neuropathy?
Look for shoes with a wide toe box, no seams inside, cushioned soles, and firm heel support. Brands like New Balance, Drew, and Hoka have therapeutic lines. Custom orthotics made from a mold of your foot reduce pressure points and improve balance. Avoid flip-flops, high heels, or tight shoes. Many insurance plans cover therapeutic footwear if you have diabetes or confirmed neuropathy.
Does exercise help neuropathy?
Yes-especially walking, swimming, and cycling. Exercise improves blood flow to nerves, helps control blood sugar, and strengthens muscles that support balance. Avoid high-impact activities if you have foot numbness. Aim for 30 minutes, 5 days a week. Even 10-minute walks after meals help lower blood sugar spikes that damage nerves. Physical therapy programs specifically designed for neuropathy show 30% fewer falls after 12 weeks.
How long does it take to see improvement after treatment?
It varies. For B12 deficiency, you might feel better in 4 to 8 weeks. For diabetes, it takes 3 to 6 months of stable blood sugar to see nerve symptoms improve. Medications like pregabalin or duloxetine often work within 1 to 2 weeks, but full effect takes 4 to 6 weeks. Scrambler therapy needs 10 sessions over 2 to 3 weeks. Patience is key-nerve healing is slow, but consistent management makes a real difference.




Man this post is gold. I’ve been living with this for 5 years and no one ever told me about Scrambler Therapy until now. I’m booking an appointment this week. If it cuts my pain in half I’ll be dancing in the kitchen.
Thanks for laying it out so clear.
B12 deficiency is way more common than people think. I had numb hands for 8 months. Doctor said it was carpal tunnel. Turned out my HbA1c was fine but my B12 was 180. One injection later and the tingling was gone.
Get tested if you’re over 50 or on acid reflux meds.
So I’m Irish and we’ve got this thing where we treat pain like it’s a personal failure. You don’t complain. You just suffer. But this? This is the first time I’ve seen someone actually talk about neuropathy without sugarcoating it.
Lyrica made me feel like a zombie. Amitriptyline? Dry mouth so bad I slept with a water bottle in my hand. But the balance exercises? Yeah. Standing on one foot while brushing my teeth. I’ve been doing it for 3 months. No more faceplanting into the fridge.
And yeah I know I misspelled faceplanting. I’m not a robot. I’m just a guy trying not to break his hip again.
Qutenza burns like hell but worth it. One session. Three months pain free. My doc said I’d need a second but I haven’t gone back. Why fix what ain’t broke?
Wear the damn socks. Don’t wait till you can’t walk.
It’s funny how we think of nerves as wires. But they’re alive. They heal. They remember. When your feet stop feeling the ground it’s not just pain. It’s isolation.
That’s why the foot checks matter. It’s not about avoiding injury. It’s about remembering you still have a body.
And yeah I know that sounds like a TED Talk. But I’ve been there. And I’m still here.
Chemo neuropathy hit me hard. Took 3 years to get diagnosed. My oncologist said it was normal. I told him my socks felt like sandpaper. He shrugged.
Finally found a neurologist who listened. Started alpha-lipoic acid. Walked 20 mins a day. Now I can feel my toes again. Not perfect. But better.
Don’t let them tell you it’s just part of the process.
People act like neuropathy is just a side effect. It’s not. It’s a warning. A scream from your body saying something’s wrong.
Diabetes isn’t the villain. Ignorance is. Waiting 18 months to get diagnosed? That’s the real tragedy.
I’ve seen people lose their feet because they thought numbness was just getting old.
It’s not. It’s treatable. But only if you act. No more waiting. No more hoping it goes away.
Go see a neurologist. Today. Not tomorrow. Today.
They’re hiding the truth. The real cause is 5G towers and the FDA selling out to Big Pharma. Lyrica was designed to keep you docile. Qutenza? Just a distraction. The real cure is magnesium and grounding. But they don’t want you to know.
Check your EMF levels. Your feet are screaming because the grid is poisoning you.
Wake up.