 13
Nov,2025
13
Nov,2025
Statin Tolerance Calculator
Find the Safest Statin for Your Genetics
Enter your SLCO1B1 genotype to see your risk of muscle pain and which statins are safest for you.
Personalized Statin Recommendations
Based on your genotype, here's what you need to know:
Simvastatin Risk:
Atorvastatin Risk:
Rosuvastatin Risk:
Pravastatin Risk:
Fluvastatin Risk:
Recommendations
How This Works
The SLCO1B1 gene affects how your body processes statins. People with the CC genotype have a significantly higher risk of muscle pain with simvastatin. Other statins like pravastatin and fluvastatin are safer options for those with high-risk genotypes.
Over 35 million Americans take statins every year to lower cholesterol and prevent heart attacks. But for up to 1 in 3 people, the benefits come with a painful cost: muscle pain, weakness, or cramps so bad they quit the drug. Many assume it’s just bad luck or aging. But for some, it’s written in their DNA.
Why Some People Can’t Tolerate Statins
Statin intolerance isn’t just about being sensitive to medicine. It’s often tied to how your body absorbs and clears these drugs. The main culprit? A gene called SLCO1B1. This gene makes a protein that shuttles statins from your blood into your liver, where they do their job. If your version of this gene has a specific mutation - called c.521T>C (or rs4149056) - your liver can’t grab statins fast enough. That leaves more of the drug floating in your muscles, causing damage. The risk isn’t the same for everyone. People with two copies of the C variant (CC genotype) are 4.5 times more likely to get severe muscle damage on high-dose simvastatin than those with two T copies (TT). About 1-2% of people of European descent fall into this high-risk group. Another 15% carry one copy (TC), doubling their risk. The problem? Most doctors don’t test for this. Patients are told to “tough it out” or switch to another statin without knowing why the first one failed.Not All Statins Are Created Equal
Here’s the twist: the SLCO1B1 gene problem mostly matters for simvastatin. It’s the most affected. Atorvastatin and rosuvastatin? Not so much. A 2021 study of nearly 12,000 people found no clear link between SLCO1B1 and muscle symptoms with these two statins. That’s why clinical guidelines only recommend genetic testing before prescribing simvastatin - not the others. If you’ve had muscle pain on simvastatin, switching to pravastatin or fluvastatin often fixes it. Why? These statins don’t rely as much on the SLCO1B1 transporter. One study showed people with the high-risk CC genotype had 80% less muscle damage on pravastatin than on simvastatin. That’s not a small difference - it’s life-changing for someone who thought they’d never be able to take a statin again.What Other Genes Might Be Involved
SLCO1B1 is the star, but it’s not the whole cast. Other genes play smaller roles. Variants in CYP2D6, CYP3A4, and CYP3A5 affect how your liver breaks down certain statins. If you’re a slow metabolizer, drugs can build up. The ABCB1 and ABCG2 genes control how statins are pushed out of cells - if those don’t work right, statins stick around longer. Then there’s GATM and CACNA1S, linked to muscle energy and calcium flow, and SOAT1, a newer find with strong statistical ties to muscle symptoms but no clear mechanism yet. The truth? No single gene explains all cases. SLCO1B1 accounts for only about 6% of statin-related muscle pain. That means most people who can’t tolerate statins don’t have this variant. Other factors - age, kidney function, diabetes, thyroid issues, alcohol use, and even vitamin D levels - matter too. Genetics is one piece. Not the whole puzzle.Who Should Get Tested?
You don’t need to be tested before your first statin. But if you’ve had muscle pain on any statin - especially simvastatin - testing makes sense. The Clinical Pharmacogenetics Implementation Consortium (CPIC) says: if you’ve had muscle symptoms and your doctor wants to try simvastatin again, test your SLCO1B1 first. If you’re CC, avoid high-dose simvastatin. Pick something else. Some clinics now test preemptively - before any statin is prescribed - especially for people with high heart disease risk. One 2021 study found that patients who got tested before starting statins were 18.7% more likely to stick with them long-term. That’s huge. If you’re young, healthy, and planning to be on statins for decades, knowing your risk early could save you years of trial and error.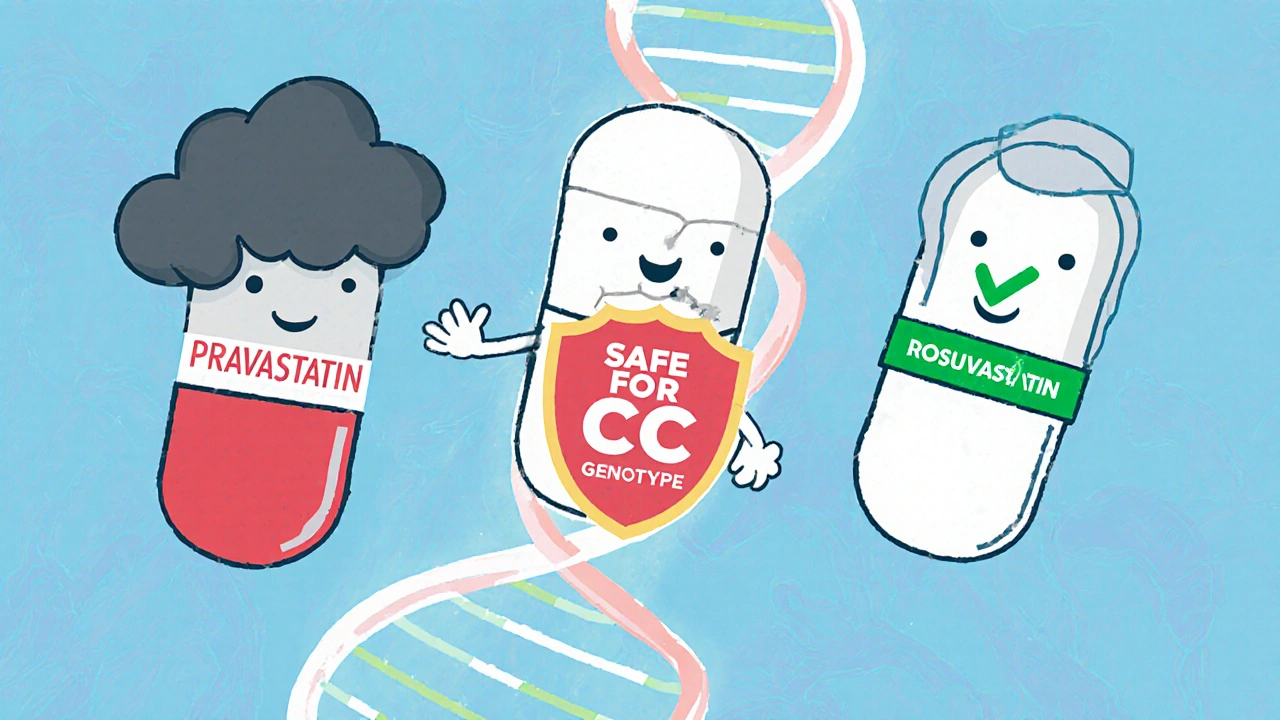
How Testing Works - and What It Costs
Testing is simple. A cheek swab or blood draw, sent to a lab. Results come back in 5 to 10 days. Companies like Mayo Clinic, ARUP, OneOme, and Color offer these tests. Some are bundled into broader pharmacogenomic panels that check dozens of genes at once. Costs vary. Standalone SLCO1B1 tests run $150-$400 out-of-pocket. Insurance coverage? Patchy. Only about 28% of private insurers covered it in 2022. Medicare only pays in limited cases. If you’re paying yourself, ask if your lab offers a cash discount - many do. But here’s the catch: not all reports are helpful. Some direct-to-consumer tests just give you raw data - a string of A’s, C’s, G’s, and T’s. That’s useless without expert interpretation. Look for labs that provide clear, actionable recommendations: “Avoid simvastatin 80mg,” “Consider pravastatin,” “Dose adjustment needed.”Do Test Results Actually Help People?
The evidence is mixed. On one hand, a Mayo Clinic survey found 78% of patients with prior statin intolerance were able to restart statin therapy after genetic guidance. On Reddit, 62% of users said switching based on their genes improved their symptoms. But a major 2020 trial in JAMA Network Open found something surprising: giving doctors SLCO1B1 results didn’t improve patient adherence or reduce muscle pain. Why? Because many doctors didn’t know what to do with the info. A 2021 survey showed only 43% of primary care doctors felt confident interpreting these results. Cardiologists? 82% were comfortable. The gap is real. The solution? Better tools. Electronic health records like Epic and Cerner now have built-in alerts. If a doctor tries to prescribe simvastatin 80mg to someone with a CC genotype, the system pops up: “High risk of myopathy. Consider alternative.” That’s how you make genetics useful - not by handing patients a report, but by embedding the advice into the workflow.What’s Next for Pharmacogenomics and Statins
The future isn’t single genes. It’s polygenic scores - combining SLCO1B1 with 10-15 other small-effect variants to build a better risk profile. Early studies show this can improve prediction accuracy from 58% to 67%. That’s not perfect, but it’s getting closer. A new group called the Statin Pharmacogenomics Implementation Consortium is working to standardize testing across 50 U.S. hospitals by 2025. The goal? Make genetic guidance routine, not rare. Meanwhile, the market is booming. The global pharmacogenomics industry is expected to hit $21 billion by 2030. Statin testing makes up a big chunk of that. But money alone won’t fix the problem. We need better education, clearer guidelines, and smarter tech - not just more tests.
What You Can Do Today
If you’ve stopped statins because of muscle pain:- Don’t assume you can’t take any statin. You might just need a different one.
- Ask your doctor about SLCO1B1 testing - especially if you were on simvastatin.
- Request pravastatin or fluvastatin as alternatives - they’re less likely to cause issues.
- If your doctor says no to testing, ask for a referral to a cardiologist or pharmacogenomics clinic.
- Check PharmGKB.org for free, evidence-based summaries on gene-drug interactions.
Frequently Asked Questions
Can genetic testing predict if I’ll get muscle pain from statins?
Yes - but only partially. The SLCO1B1 gene variant c.521T>C strongly predicts risk for simvastatin-related muscle damage, especially in people with two copies of the C allele. But it doesn’t explain most cases of statin intolerance. Other genes, lifestyle factors, and medical conditions also play a role. Testing can reduce risk, but it can’t eliminate it.
Is pharmacogenomic testing covered by insurance?
Sometimes. As of 2023, only about 28% of private insurers cover SLCO1B1 testing for statin intolerance. Medicare covers it only in specific cases under the Molecular Diagnostic Services Program. Out-of-pocket costs range from $150 to $400. Always ask your lab for a price quote and check if your plan requires prior authorization.
Should I get tested before my first statin prescription?
It’s not routinely recommended for everyone. But if you have a strong family history of statin intolerance, are over 65, have kidney disease, or plan to take statins long-term, preemptive testing may help avoid future problems. Studies show it improves adherence by nearly 20%. Talk to your doctor about whether it makes sense for your situation.
What statins are safest if I have the SLCO1B1 CC genotype?
Pravastatin and fluvastatin are the safest choices. They don’t rely heavily on the SLCO1B1 transporter to enter the liver, so they’re much less likely to cause muscle damage in people with the CC genotype. Rosuvastatin and atorvastatin are also generally safe options. Avoid simvastatin, especially at 80mg daily, if you’re CC.
Can I trust direct-to-consumer genetic tests like 23andMe for statin advice?
Some direct-to-consumer tests include SLCO1B1 data, but they rarely interpret it for statin use. You might see your genotype (TT, TC, or CC), but not whether you should avoid simvastatin. These reports aren’t designed for clinical use. Always confirm results with a clinical lab and discuss them with a doctor or pharmacist trained in pharmacogenomics.






Man I wish I knew this before I quit simvastatin last year. Muscle pain was brutal, thought I was just getting old. Switched to pravastatin on my doc’s suggestion and boom-no issues. Genetics isn’t magic but it’s way better than guessing.
slco1b1 is real. my cousin had the cc variant. tried simvastatin, couldn’t walk for weeks. switched to rosuvastatin, zero problems. doctors need to stop treating everyone the same.
This is why medicine is broken. You test one gene and act like it’s the whole story. Meanwhile people die from heart attacks because they’re too scared to take statins after one bad experience. Stop overcomplicating it.
While the genetic component is scientifically compelling, one must consider the broader clinical context. The absence of standardized implementation protocols across primary care settings renders such testing, in many instances, functionally inert.
So now we’re paying for DNA tests just to avoid a pill? In India we don’t even have clean water but you want me to spend $400 on a gene test? This is rich people medicine. My uncle took simvastatin for 10 years, never had a problem. Stop overthinking.
As someone from India who’s been on statins for 8 years, I can say this: most doctors here don’t even know what SLCO1B1 is. But I switched to pravastatin after muscle pain and it worked. You don’t need a test if you listen to your body. Try another statin first, then think about genes.
Of course you need genetic testing. If you’re dumb enough to take simvastatin without checking your genes, you deserve the muscle pain. I’m not joking. This isn’t ‘maybe’-it’s basic science. Stop being a coward and get tested.
I got tested after my third statin failed. Turns out I’m TC. Switched to atorvastatin and now I’m running 5Ks again. No more fear. This saved my health. If you’re struggling, just ask. Seriously.
Thank you for writing this. I’ve been trying to explain this to my GP for months. He said ‘it’s just side effects.’ I showed him the CPIC guidelines. He still shrugged. People need to stop treating genetic info like a luxury. It’s medicine.
The polygenic risk score data is still nascent, but preliminary cohort analyses suggest a 9.2% incremental predictive value over SLCO1B1 alone when combined with CYP2D6 and ABCG2 variants. Clinical utility remains constrained by EHR integration deficits.
It is profoundly lamentable that the medical establishment continues to rely on empirical trial-and-error methodologies in the face of unequivocal pharmacogenomic evidence. The persistence of such archaic practices constitutes a systemic failure of epistemic responsibility.
My brother got the test, found out he’s CC, switched to fluvastatin. Now he’s healthy. But my cousin? He’s TT, took simvastatin for 12 years, never had an issue. So what’s the point? Genetics doesn’t mean anything if you don’t know how to use it.
It is my understanding that the Clinical Pharmacogenetics Implementation Consortium has issued formal guidelines regarding the use of SLCO1B1 genotyping in the context of simvastatin administration. These guidelines are not universally adopted. The disparity between evidence and practice is concerning
Just got my 23andMe results. I’m CC. My doctor said ‘eh, you’ll be fine.’ So I’m off statins. Guess I’ll just eat kale and pray.