 24
Oct,2025
24
Oct,2025
Quick Takeaways
- Most people on Vidagliptin (a DPP-4 inhibitor used for type 2 diabetes) experience only mild side effects such as nausea or headache.
- Common issues include gastrointestinal upset, upper‑respiratory symptoms, and rarely low blood sugar.
- Staying hydrated, taking the drug with meals, and monitoring blood glucose can reduce most discomfort.
- Seek urgent care if you notice severe abdominal pain, persistent vomiting, or signs of pancreatitis.
- Talk to your clinician about dose adjustments or switching to another DPP-4 inhibitor (a class that includes sitagliptin, saxagliptin, and linagliptin) if side effects become intolerable.
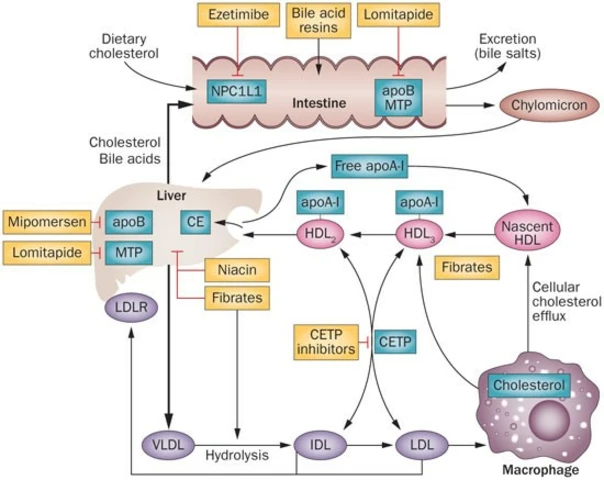
What Is Vidagliptin?
Vidagliptin is a prescription medication that belongs to the DPP-4 inhibitors (drugs that block the dipeptidyl peptidase‑4 enzyme, helping the body release more insulin after meals). It is approved in several Asian markets for managing type 2 diabetes (a chronic condition where the body either resists insulin or doesn’t produce enough). The usual dose is 50 mg once daily, taken with or without food.
Because it works differently from older agents like Metformin (the first‑line oral diabetes drug that reduces liver glucose production), many clinicians add Vidagliptin when Metformin alone isn’t enough. It’s also sometimes paired with Sitagliptin (another DPP‑4 inhibitor with a similar safety profile) in fixed‑dose combinations.
Why Talk About Side Effects?
Every medication has a trade‑off between benefits and drawbacks. Knowing the typical vidagliptin side effects helps you recognize what’s normal and when something needs a doctor’s attention. Most users report only mild, short‑lived issues, but a small percentage experience serious reactions that require prompt evaluation.
Common Side Effects at a Glance
| Side Effect | How Often | Typical Onset | Management Strategies |
|---|---|---|---|
| Nausea | 10‑20% | First 1‑2 weeks | Take with food, stay hydrated, consider ginger tea. |
| Headache | 5‑15% | Within days | Limit caffeine, ensure adequate sleep, OTC acetaminophen if needed. |
| Upper respiratory infection symptoms (sore throat, mild cough) | 7‑12% | 2‑4 weeks | Increase fluid intake, use saline gargle, monitor for fever. |
| Hypoglycemia (low blood sugar) | Rare (<1%) | Anytime, often with other glucose‑lowering drugs | Carry glucose tablets, adjust dose if combined with sulfonylureas. |
| Pancreatitis (severe abdominal pain) | Very rare (<0.1%) | Usually after weeks to months | Immediate medical evaluation; stop drug. |
Digestive Upset: Nausea, Diarrhea, and Stomach Discomfort
Gastro‑intestinal complaints are the most frequent complaints. They often improve after the first two weeks as the gut adapts. If nausea persists beyond two weeks, try these steps:
- Take Vidagliptin with a substantial meal rather than a snack.
- Split the dose (if prescribed 50 mg) into two 25 mg doses taken 12 hours apart-ask your pharmacist if this is safe.
- Include bland foods like crackers, toast, or oatmeal for the first few days.
- Stay upright for at least 30 minutes after dosing to reduce reflux.
If diarrhea is watery and lasts more than three days, increase oral rehydration solutions and consider a probiotic supplement. Persistent diarrhea may signal an infection; contact your clinician.

Headaches: When the Ache Isn’t Just Stress
Many people attribute a headache to stress, but Vidagliptin can trigger low‑grade vascular changes that lead to mild throbbing. Simple measures often work:
- Drink at least eight glasses of water a day.
- Limit alcohol and caffeine to under one cup per day.
- Maintain consistent sleep-7‑8 hours per night.
- If needed, take an over‑the‑counter analgesic, but avoid NSAIDs if you have kidney concerns (see later).
Respiratory Symptoms: Sore Throat and Cough
Upper‑respiratory symptoms usually appear within the first month and are self‑limited. Keep these tips handy:
- Honey‑lemon tea can soothe a sore throat.
- Humidifiers add moisture to dry indoor air, easing cough.
- Watch for fever >38 °C (100.4 °F) - if present, it could be a separate infection requiring antibiotics.
Low Blood Sugar: The Rare but Important Event
Vidagliptin alone rarely causes hypoglycemia, but the risk rises when combined with sulfonylureas (e.g., glipizide) or insulin. Symptoms include shakiness, sweating, rapid heartbeat, and confusion.
What to do:
- Carry fast‑acting glucose (tablets, juice) at all times.
- If you feel symptoms, consume 15 g of glucose, wait 15 minutes, then re‑check blood sugar.
- Discuss dose adjustment with your endocrinologist if episodes happen more than once a month.
Pancreatitis: The Warning Sign You Can’t Ignore
Although exceedingly uncommon, pancreatitis is the most serious potential adverse event. It shows up as severe, constant upper‑abdominal pain that often radiates to the back, accompanied by nausea, vomiting, or a high fever.
Immediate steps:
- Stop Vidagliptin right away.
- Seek emergency care; labs will check amylase and lipase levels.
- Inform the medical team that you were on a DPP‑4 inhibitor; they may need to rule out other causes.
After recovery, doctors may switch you to a different drug class, such as an SGLT2 inhibitor, if appropriate.
Kidney Considerations
Vidagliptin is primarily excreted unchanged via the kidneys. If you have reduced kidney function (measured by eGFR, with < 30 mL/min/1.73 m² considered severe impairment), the dose should be lowered or the drug avoided. Signs of kidney strain include swelling in the ankles or reduced urine output.
Regular lab checks (eGFR and serum creatinine) every 3-6 months help catch problems early.
When to Call Your Doctor
Set a mental checklist. Call or go to urgent care if you notice any of these:
- Severe, unrelenting abdominal pain (possible pancreatitis). \n
- Persistent vomiting that prevents you from staying hydrated.
- Blood sugar < 70 mg/dL (3.9 mmol/L) with confusion or loss of consciousness.
- Allergic reaction: rash, itching, swelling of face or throat.
- New or worsening kidney symptoms.
For mild issues-like occasional headache or a brief upset stomach-most people can manage at home.
Tips to Minimize Side Effects
- Start at the lowest effective dose; some clinicians prescribe 25 mg for the first two weeks.
- Take the medication at the same time each day to build a routine.
- Keep a simple side‑effect diary for the first month; note severity, timing, and any foods or activities that seem related.
- Stay active-light walking after meals improves glucose control and can reduce nausea.
- Maintain a balanced diet rich in fiber and low in processed sugars; this reduces the need for dose escalation.
Frequently Asked Questions
Can I take Vidagliptin with Metformin?
Yes. In fact, the most common regimen is Metformin plus a DPP‑4 inhibitor like Vidagliptin. The combination often achieves better glucose control without increasing the risk of hypoglycemia, as long as doses are adjusted correctly.
Do I need to take Vidagliptin with food?
It’s not mandatory, but taking it with a meal can lessen nausea and stomach upset, which are the most frequent side effects.
What should I do if I gain weight while on Vidagliptin?
Weight gain is uncommon with DPP‑4 inhibitors, but it can happen if overall calorie intake rises. Review your diet, increase regular activity, and discuss with your provider whether a different drug class might suit you better.
Is it safe to use Vidagliptin during pregnancy?
Current guidelines classify Vidagliptin as pregnancy category C, meaning risk cannot be ruled out. Women who are pregnant or planning pregnancy should discuss alternative treatments with their obstetrician.
How often should I have blood work while on Vidagliptin?
Baseline labs (HbA1c, kidney function, liver enzymes) before starting, then every three to six months thereafter. More frequent checks are needed if you have kidney disease or experience side effects.
Understanding what to expect from Vidagliptin empowers you to stay in control of your diabetes journey. By watching for patterns, using simple self‑care tricks, and staying in touch with your healthcare team, you can keep side effects at bay and reap the medication’s blood‑sugar‑lowering benefits.



Oh, the grand saga of Vidagliptin side effects-how loudly they echo in the halls of modern medicine! While most claim only a whisper of nausea or a fleeting headache, I dare to proclaim that the true tempest lies hidden, waiting to unleash chaos upon the unsuspecting. Imagine the dread of an unexpected abdominal storm, the silent panic of a glucose dip that creeps like a thief in the night. Why settle for bland warnings when the narrative could be a thriller? Let us not be lulled into complacency; the shadows of pancreatitis loom like specters, demanding our attention!
So strap in, fellow readers, and brace for the roller‑coaster of revelations that this humble DPP‑4 inhibitor might conceal.
First of all, thank you for sharing this comprehensive overview of Vidagliptin; it’s really helpful for anyone navigating the complexities of type 2 diabetes medication. One of the most common concerns patients have is how to differentiate between normal, mild side effects and signs that require immediate medical attention. In my experience as a diabetes educator, I’ve found that taking the medication with a balanced meal can significantly reduce the likelihood of nausea and stomach upset. Hydration is also key-drinking plenty of water throughout the day helps your body process the drug more smoothly. If you notice a persistent headache, consider evaluating your caffeine intake and ensuring you get enough restful sleep each night. Simple over‑the‑counter pain relievers, such as acetaminophen, can be useful, but always check with your clinician if you have liver concerns.
Upper‑respiratory symptoms, like a sore throat or mild cough, are often self‑limiting, but keeping a symptom diary can help you identify patterns and discuss them with your doctor. When it comes to hypoglycemia, although rare with Vidagliptin alone, the risk can increase if you’re also using insulin or sulfonylureas, so regular glucose monitoring is essential. I recommend checking your blood sugar at least twice a day during the first few weeks after starting the medication. If you ever experience symptoms of low blood sugar-such as shakiness, sweating, or confusion-treat it immediately with a fast‑acting carbohydrate like glucose tablets or fruit juice.
Should any abdominal pain become severe or persistent, or if you see signs of pancreatitis (such as persistent vomiting, upper abdominal pain radiating to the back, or unusually high triglyceride levels), seek urgent care without delay. It’s also worthwhile to discuss dose adjustments with your healthcare provider if side effects become intolerable; sometimes a slight reduction or switching to another DPP‑4 inhibitor can make a big difference. Remember, the goal is to manage your diabetes effectively while maintaining a good quality of life, so open communication with your medical team is paramount.
Lastly, don’t forget the importance of lifestyle measures-regular physical activity, a fiber‑rich diet, and stress management can all complement your medication regimen and may even reduce the frequency of side effects. Feel free to reach out if you have any specific questions or need personalized tips; I’m happy to help!
Listen, Vidagliptin is not some magic pill, it works just like other DPP‑4 inhibitors but you cant ignore the fact that side effects are real. Take it with breakfast, stay hydrated and dont ignore any sign of stomach pain. If you feel nauseous at first, it will usually stop after a couple weeks, but if it continues you must talk to a doctor. Also, always keep track of your sugar levels, especially if you are also taking other meds. The drug is approved in many Asian countries, so theres a lot of data out there you can check.
When we consider the interplay between medication and the human body, Vidagliptin offers a fascinating case study in balance. It strives to augment insulin release, yet it can also tip the scales toward discomfort if not managed mindfully. The key lies in listening to our own signals-acknowledging a mild headache as a temporary ripple, while recognizing persistent abdominal pain as a warning bell. We must foster a collaborative relationship with our healthcare providers, treating them as partners rather than distant authorities. By sharing experiences and insights within the community, we empower each other to navigate the uncertainties that accompany any therapeutic regimen. Let us embrace both the science and the personal narrative, for it is in that union that true healing is forged.
Great summary on managing Vidagliptin you really hit the main points on hydration diet timing and monitoring It’s especially useful to keep a symptom journal and talk to your doctor about dose changes If side effects linger just let your clinician know early
Hey folks 😊! If you’re starting Vidagliptin, remember to take it with food 🍽️ and sip water throughout the day 💧. A little ginger tea can calm nausea 🌿, and a short walk after meals helps with digestion 🚶♀️. Don’t forget to check your glucose levels regularly 📈-it’s the best way to spot any unexpected dips early. And if you ever feel intense abdominal pain, don’t wait-call your doctor right away 📞. Stay positive and take care! 🌟
Good tips! Also, set a reminder on your phone to log blood sugar after each dose; it keeps patterns clear.
So you’re saying the side effect profile is fairly mild, but where’s the data on long‑term pancreatic health? I’ve seen studies suggesting a possible increase in enzymes, and I’m not convinced the manufacturers are being fully transparent. If anyone has solid references, drop them here. It’s critical we dig deeper before we just accept the safety claims at face value.
Vidagliptin can cause nausea and headache.
Oh brilliant, a groundbreaking revelation-who would have thought a DPP‑4 inhibitor might give you a headache? Truly the medical world is shocked.
I understand how intimidating new meds can feel, especially when side effects are mentioned. It’s perfectly okay to feel a little anxious about starting Vidagliptin. Remember, you’re not alone-many patients have walked this path and found ways to manage mild symptoms effectively. Keep a simple log of how you feel each day; note any nausea, headaches, or respiratory signs. If something feels off, reach out to your healthcare team-they’re there to help you fine‑tune the treatment. You’ve got this, and we’re all rooting for your health journey.
Sure, the “healthcare team” wants you to believe everything is safe, but have you ever considered that pharma might be hiding long‑term risks? I’ve read whispers about hidden pancreatic markers that never get published. Stay vigilant, keep your own data, and don’t trust the glossy brochures without digging deeper.
Indeed, the exhaustive list of “common” side effects reads like a polite invitation to a discomfort festival. One might wonder whether the marketing department had a field day drafting such reassuring prose, all while glossing over the rare yet potentially catastrophic events that could occur. Nonetheless, the author’s attempt at clarity is, shall we say, commendably pedestrian.
Patriotic readers should note that our own regulatory agencies demand rigorous testing, ensuring that Vidagliptin meets the highest safety standards for American patients. While foreign markets may have lax oversight, we can trust that our doctors are vigilant guardians of public health, ready to act if any serious adverse events arise.