Pharmacy Safety: Protect Yourself from Medication Risks
When you walk into a pharmacy, you expect the medicine you get to be safe, accurate, and effective. But pharmacy safety, the system of practices that ensures medications are dispensed correctly and without harm. Also known as medication safety, it’s not just about the pharmacist’s accuracy—it’s about how well you, the patient, can spot red flags before it’s too late. Every year, hundreds of thousands of people in the U.S. end up in the hospital because of preventable medication errors. Some are from mix-ups in dosage. Others come from hidden drug interactions or counterfeit pills that look real but contain nothing—or worse, fentanyl.
Drug interactions, when two or more medicines react in harmful ways inside your body. Also known as medication conflicts, they’re one of the most dangerous but overlooked risks. Think of it like mixing bleach and ammonia—some combinations are silent killers. Opioids with alcohol or benzodiazepines? That’s a deadly combo. Even something as simple as grapefruit juice can turn a normal dose of a blood pressure pill into a toxic one. And if you’re taking multiple meds for different conditions, you’re not just at risk—you’re playing Russian roulette without knowing the chamber.
FDA safety communications, official alerts from the U.S. Food and Drug Administration about newly discovered risks with approved drugs. Also known as drug safety alerts, they’re your best defense against hidden dangers. These aren’t marketing emails or social media rumors—they’re urgent, science-backed warnings. A recent alert told doctors to stop prescribing certain diabetes drugs because they caused rare but fatal pancreas damage. Another warned that a popular statin could cause muscle breakdown in people with a specific gene. If you’re on long-term medication, checking these alerts every few months isn’t paranoia—it’s survival.
And then there’s the rise of counterfeit drugs, fake medications sold online or in unlicensed pharmacies that may contain no active ingredient, wrong ingredients, or dangerous contaminants. You might think you’re saving money buying cheap gabapentin or Zovirax online, but you could be swallowing chalk, rat poison, or synthetic opioids. The FDA has seized thousands of fake pills labeled as Adderall, Xanax, and even insulin. If a deal seems too good to be true, it’s not a deal—it’s a trap.
Pharmacy safety doesn’t end when you leave the counter. It starts with asking questions: Why am I taking this? What happens if I miss a dose? What should I avoid mixing with it? It means checking the pill’s color, shape, and imprint against official databases. It means keeping a written list of everything you take—including supplements—and bringing it to every doctor visit. It means knowing how to spot a fake pharmacy website, how to safely carry liquid meds through airport security, and when to walk away from a pharmacist who won’t answer your questions.
What you’ll find below isn’t theory. These are real stories from people who nearly died because they didn’t know the risks—and what they did to fix it. From how genetic testing can prevent statin side effects, to why some generic creams fail to work, to how to read an FDA alert without panicking—this collection gives you the tools to take control. No fluff. No jargon. Just what you need to stay safe when your health depends on a tiny pill.
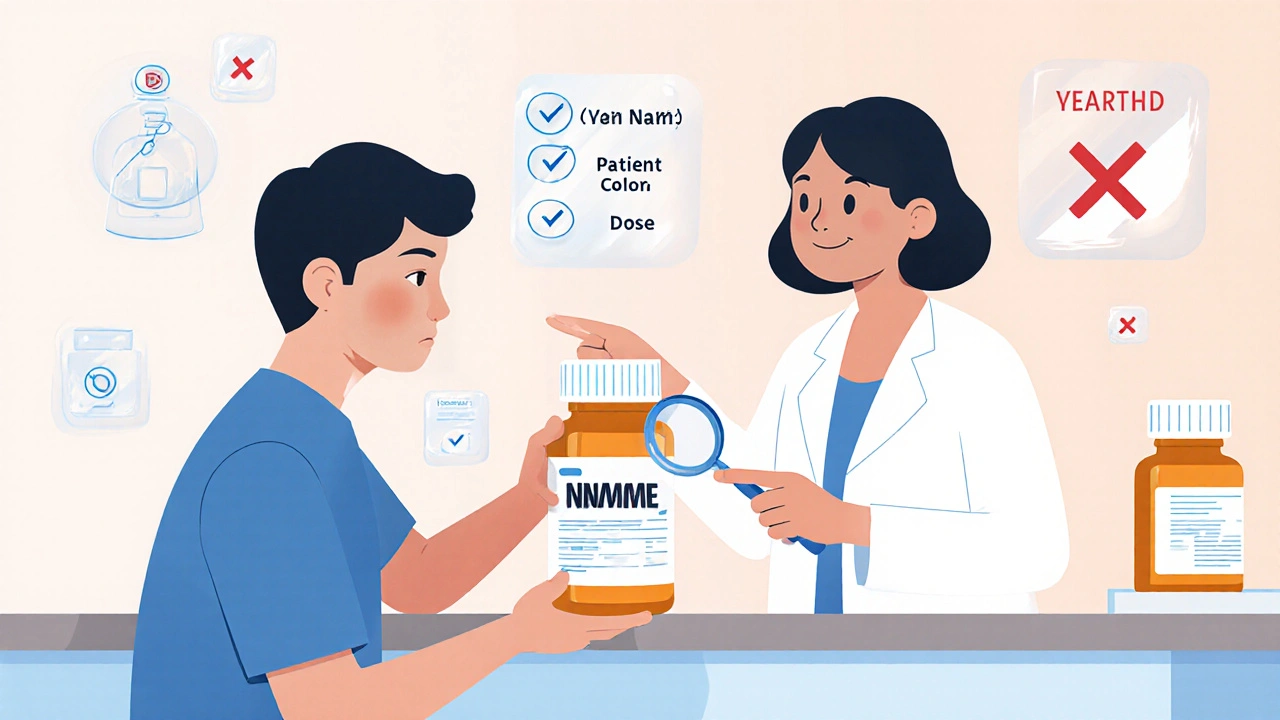
Verifying Your Prescription at the Pharmacy: A Simple Patient Checklist to Avoid Medication Errors
Learn how to check your prescription at the pharmacy with this simple 7-point checklist to avoid dangerous medication errors. Your eyes could save your life.
View more