 7
Jan,2026
7
Jan,2026
Every year, millions of people in Australia and around the world take over-the-counter (OTC) medications without thinking twice. A headache? Grab some ibuprofen. A cold? Reach for the multi-symptom relief tablet. Trouble sleeping? Diphenhydramine is right there on the shelf. But here’s the thing most people don’t realize: OTC medications aren’t harmless. They can react dangerously with the prescription drugs you’re already taking - sometimes with life-threatening results.
You might think, "I’m just taking a little painkiller," or "It’s just a sleep aid." But if you’re on blood pressure medication, an antidepressant, or a blood thinner, that "little" pill could be setting off a hidden chemical bomb in your body. The FDA says OTC meds can make your prescription less effective, cause unexpected side effects, or even turn a safe drug into a dangerous one. And the worst part? Most people never tell their doctor they’re taking them.
Why OTC Medications Are Riskier Than You Think
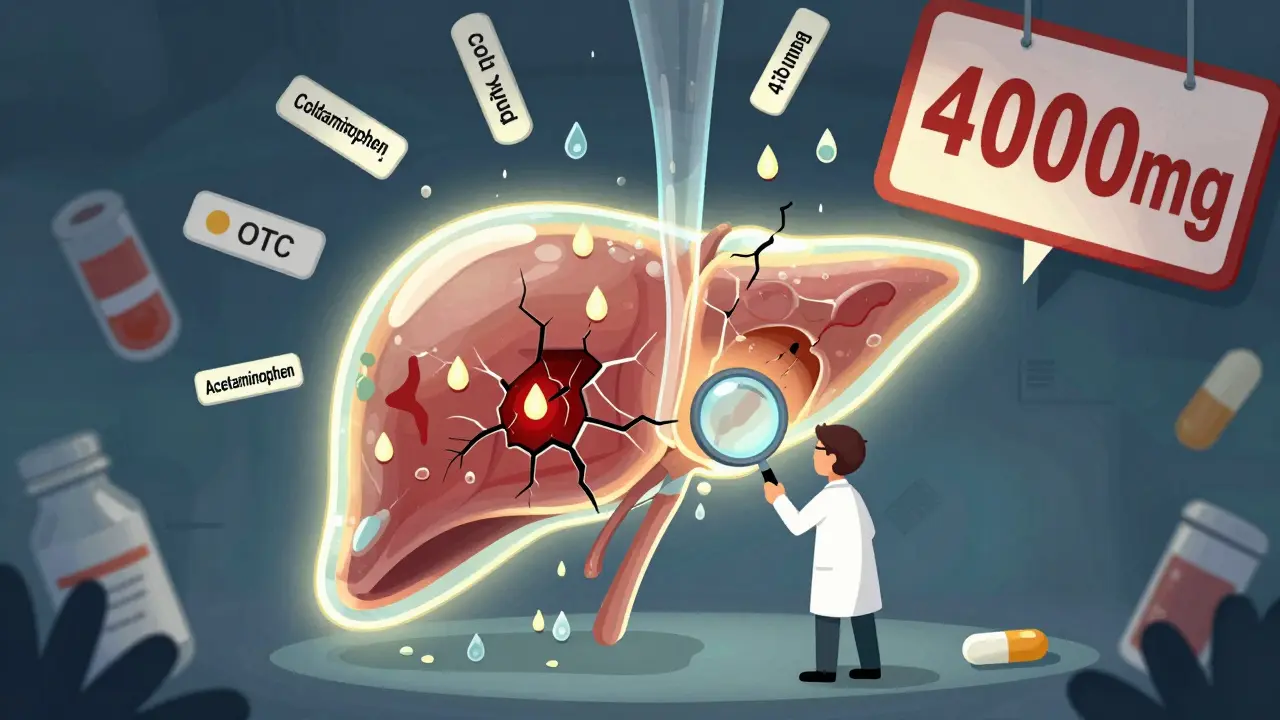
OTC drugs aren’t tested in isolation. They’re tested for safety when taken alone - not when mixed with five other pills you’re swallowing every day. The problem gets worse when you don’t even know what’s in them. Take acetaminophen, for example. It’s in more than 200 different products: pain relievers, cold medicines, flu remedies, sleep aids, even some prescription painkillers. If you take two of these at once - say, a cold tablet and a headache pill - you could easily hit 7,000 mg in a day. The safe limit? 4,000 mg. Exceed that, and you risk acute liver failure. No warning. No symptoms until it’s too late.
Then there’s the NSAID family: ibuprofen, naproxen, diclofenac. These are common painkillers, but they don’t play nice with heart medications. If you’re on low-dose aspirin to prevent a heart attack, taking ibuprofen can block aspirin’s protective effect. That’s not theoretical - it’s been proven in clinical studies. One study found that people on daily aspirin who also took ibuprofen had a 30% higher risk of heart events. And if you’re on warfarin or another blood thinner? NSAIDs can triple your risk of internal bleeding.
The Silent Killer: Acetaminophen Overdose
Acetaminophen is the most common cause of accidental poisoning in hospitals. Why? Because it’s everywhere. You take it for your back pain. Your partner takes it for their migraine. You both grab the same bottle. Or worse - you take a cold medicine that has it, then take Tylenol for your fever. You don’t realize you’re doubling up. The liver doesn’t scream. It doesn’t warn you. By the time you feel sick, it’s often too late.
Here’s what you need to know: every tablet, capsule, or spoonful of acetaminophen adds up. If you’re taking more than one product, check the label. Look for "acetaminophen" - not just "Tylenol" or "paracetamol." If it’s listed, count it. Keep your total under 4,000 mg per day. If you have liver disease, diabetes, or drink alcohol regularly, talk to your pharmacist. You might need to cut that limit in half.
NSAIDs and Blood Pressure: A Dangerous Mix
If you’re on medication for high blood pressure - like lisinopril, losartan, or amlodipine - NSAIDs can make it worse. They don’t just interfere. They can raise your blood pressure by 5 to 15 mmHg. That’s enough to undo months of careful control. It’s not just about the painkiller, either. Topical NSAIDs like Voltaren gel can get absorbed through the skin and cause the same problem.
And if you’re also on a diuretic - a water pill - the risk of kidney damage spikes. NSAIDs reduce blood flow to the kidneys. Diuretics already stress them. Together, they can cause acute kidney injury. This isn’t rare. Studies show it’s one of the top reasons older adults end up in the ER after starting a new OTC painkiller.
Antidepressants and Serotonin Overload
SSRIs like sertraline or escitalopram are common antidepressants. But if you take them with certain OTC cold medicines - especially those containing dextromethorphan (DXM) - you risk serotonin syndrome. This isn’t just nausea or dizziness. It’s a medical emergency. Your body overheats. Your muscles spasm. Your heart races. You can slip into a coma. And it happens fast.
Dextromethorphan is in cough syrups, cold tablets, and even some sleep aids. It’s labeled as "cough suppressant," but it’s also a serotonin booster. Combine it with your antidepressant, and you’re playing Russian roulette with your brain chemistry. Tramadol, a painkiller sometimes sold OTC in lower doses, does the same thing. So does linezolid, an antibiotic sometimes used for stubborn infections. If you’re on an SSRI, avoid all of them unless your doctor says it’s safe.
Antacids and Thyroid Meds: A Hidden Sabotage
Levothyroxine, the most common thyroid medication, needs to be absorbed in the stomach. But if you take an antacid - like Tums or Rolaids - at the same time, it blocks that absorption. Studies show your thyroid hormone levels can drop by up to 25%. That means you’ll feel tired, gain weight, and your cholesterol might spike - even if you’re taking your pill "correctly."
Same thing happens with proton pump inhibitors (PPIs) like omeprazole. These are common for heartburn. But they lower stomach acid so much that levothyroxine can’t be absorbed properly. The fix? Take your thyroid pill first thing in the morning on an empty stomach. Wait at least 4 hours before taking any antacid or PPI. If you’re unsure, ask your pharmacist to map out your schedule.
Who’s at Highest Risk?
It’s not just older people. But they’re the most vulnerable. The average Australian over 65 takes five or more medications a day - including OTCs. That’s a recipe for collisions. But younger people aren’t safe either. If you have kidney disease, liver problems, heart failure, or diabetes, your body processes drugs differently. What’s safe for someone else could be toxic for you.
People on blood thinners, antidepressants, or heart medications need to be especially careful. So do those with glaucoma, enlarged prostate, or breathing problems. First-generation antihistamines like diphenhydramine can make these worse. They cause drowsiness, dry mouth, urinary retention - and can trigger falls in the elderly. Second-generation antihistamines like loratadine or cetirizine are safer, but still not risk-free.
What You Should Do Right Now
Here’s a simple checklist. Do this today:
- Write down every pill, capsule, gel, or syrup you take - even if it’s "just once in a while." Include OTC meds, vitamins, herbal supplements, and CBD oil.
- For each one, write the active ingredient. Don’t trust the brand name. Look on the label. "Acetaminophen" is the active ingredient in Tylenol, Panadol, and many cold meds.
- Take that list to your pharmacist. Not your doctor. Your pharmacist sees this every day. They know which combinations are dangerous. Ask: "Which of these could interact with my prescription drugs?"
- Don’t start any new OTC medicine without checking first. Even "natural" remedies like St. John’s Wort or garlic supplements can interfere with blood thinners and antidepressants.
- Use a single pharmacy for all your prescriptions and OTC buys. They’ll flag interactions in their system.

Red Flags You Can’t Ignore
If you start feeling any of these after taking a new OTC medicine, stop it and call your doctor or go to the ER:
- Sudden confusion, agitation, or hallucinations
- Unexplained bruising, bleeding gums, or blood in stool
- Severe dizziness, fainting, or rapid heartbeat
- Yellowing of skin or eyes (jaundice)
- Swelling in hands, feet, or face
- Difficulty breathing or chest tightness
These aren’t side effects. They’re warning signs. And they’re preventable.
What’s Changing in 2026
Regulators are waking up. In March 2022, the FDA required clearer labels on OTC products that carry high interaction risks. You’ll now see warnings like: "Do not use if taking blood thinners" or "May interfere with thyroid medication." It’s a start. But the real change is happening in pharmacies. Most now offer free interaction checks when you pick up a prescription. Ask for it. Use it.
Apps are catching up too. Tools like WebMD’s Drug Interaction Checker now include over 24,000 medications - including OTCs and supplements. You can scan your pills or type them in. It’ll tell you if something’s dangerous. But don’t rely on it alone. Talk to a human. Algorithms miss things. Pharmacists catch them.
Final Thought: You’re Not Being Careless - You’re Misinformed
Most people don’t take OTC meds to be reckless. They take them because they’re easy, cheap, and sold next to gum and candy. No one warns them. No one asks. But your body doesn’t care if it’s prescription or OTC. It reacts to chemicals. And those chemicals don’t read labels - they react with each other.
So next time you reach for that painkiller, cold tablet, or sleep aid, pause. Ask yourself: "Is this safe with what I’m already taking?" Then go ask your pharmacist. They’re trained for this. They’re not selling you anything. They’re keeping you alive.
Can I take ibuprofen with my blood pressure medicine?
It depends. Ibuprofen and other NSAIDs can raise your blood pressure and reduce the effectiveness of your medication. If you have heart disease, kidney issues, or are on a diuretic, the risk is higher. Talk to your pharmacist before using ibuprofen. Alternatives like acetaminophen may be safer - but only if you don’t exceed 4,000 mg per day.
Is it safe to take Tylenol with antidepressants?
Yes, acetaminophen (Tylenol) is generally safe with most antidepressants, including SSRIs. Unlike NSAIDs, it doesn’t increase bleeding risk or affect serotonin levels. But be careful not to exceed 4,000 mg per day, especially if you drink alcohol or have liver problems. Always check if your cold or sleep medicine also contains acetaminophen.
Why do I need to tell my pharmacist about vitamins and supplements?
Because they’re not harmless. St. John’s Wort can make birth control, antidepressants, and blood thinners less effective. Calcium and iron supplements can block thyroid medication absorption. Even vitamin K can reduce the effect of warfarin. Pharmacists track these interactions daily. If you don’t tell them, they can’t help you.
Can OTC meds cause kidney damage?
Yes. NSAIDs like ibuprofen and naproxen reduce blood flow to the kidneys. When taken with diuretics, ACE inhibitors, or ARBs - common for high blood pressure and heart failure - they can cause acute kidney injury. This is especially dangerous for older adults or people with diabetes. If you’re on these meds, avoid long-term NSAID use. Ask your pharmacist for alternatives.
What’s the safest OTC painkiller for someone on blood thinners?
Acetaminophen (Tylenol) is usually the safest choice. NSAIDs like ibuprofen and naproxen increase bleeding risk by 2-4 times when taken with warfarin or similar drugs. Even topical NSAIDs can be risky. But remember: don’t exceed 4,000 mg of acetaminophen per day. And if you have liver disease, talk to your doctor first.
How do I know if my OTC medicine has the same active ingredient as my prescription?
Always read the "Active Ingredients" section on the label. Don’t rely on brand names. For example, Vicodin contains acetaminophen - so does Tylenol, DayQuil, and many cold remedies. If you’re taking both, you’re doubling your dose. Write down the active ingredient for every medicine you take. Compare them. If two have the same one, don’t take them together.





just took ibuprofen for my headache and now i’m scared lol
India’s got the same problem - people buy OTC meds like candy from roadside stalls. No prescription? No problem. Then they end up in the ER with liver failure and wonder why. This isn’t just a Western issue - it’s a global ignorance crisis.
Pharmacists here? Most don’t even speak English. And the ones who do? They’re too busy counting cash to care. We need mandatory labeling in regional languages - not just English and Hindi. If your grandma can’t read it, it’s useless.
Isn’t it fascinating how we’ve outsourced our biological autonomy to corporate chemistry? We live in a world where a painkiller sold next to chewing gum holds more power over our nervous systems than our own willpower - and yet we treat it like a snack.
The pharmaceutical industry doesn’t sell medicine - it sells convenience disguised as safety. They design products to be addictive in their accessibility. Acetaminophen? It’s not a drug - it’s a social contract. We all agree to ignore the fine print because the alternative is discomfort. And discomfort? That’s un-American. That’s un-Indian. That’s un-human.
But here’s the irony: our bodies don’t negotiate. They don’t care about your cultural identity, your nationalism, your Instagram aesthetic. They just react. And when they do? You’re left wondering why your liver gave up on you - while the label on the bottle says ‘safe for daily use.’
This post is vital. I work in primary care and see this every week. People come in with jaundice, confused because they ‘only took Tylenol for a fever’ - and didn’t realize their cold medicine had it too.
Don’t wait until you’re in the ER. Take 10 minutes today. Write down every pill, supplement, gel, or tea you take - even ‘natural’ stuff like turmeric or St. John’s Wort. Bring it to your pharmacist. They’re not judging you. They’re saving your life.
And if you’re a caregiver for an older adult? Do this for them. They’re not being careless. They’re just not told.
I used to think OTC meant ‘safe’ - until my mom ended up in the hospital after taking ibuprofen with her blood pressure med. She didn’t know it could raise her BP. She thought ‘if it’s on the shelf, it’s fine.’
Now I keep a little notebook in my purse with all my meds and their active ingredients. I show it to every pharmacist. I’ve started asking my friends too. It’s not scary - it’s just smart. You don’t need to be a doctor to protect yourself. You just need to be curious.
And if you’re like me and hate reading tiny print? Use the WebMD app. Scan the barcode. Boom. Instant warning. No excuse anymore.
Wait - so if I take a cold medicine with acetaminophen and then take Tylenol for my headache… I’m overdosing? That’s wild. I’ve done that like three times.
And I thought I was being smart - using OTC stuff to avoid the doctor. Turns out I was just being dumb.
Thanks for the checklist. I’m printing it out. I’m putting it on my fridge. I’m showing my dad. He’s 72 and takes like 8 things a day. He’s gonna hate this, but he needs it.
I used to think pharmacists were just people who handed out pills. Then I started asking them questions. Turns out they know way more than my doctor sometimes. They’ve seen every bad combo imaginable.
Now I go to the pharmacy first - even before I see my doctor - and say, ‘Hey, here’s my list. What’s gonna kill me?’
They laugh. Then they give me a 15-minute lecture. Worth it.
Chemistry doesn’t care about your intentions - only your dosage.
We live in a world of invisible wars: between molecules, between enzymes, between the quiet, unassuming pill on the shelf and the one in your medicine cabinet that you forgot you were taking.
Acetaminophen isn’t a drug - it’s a silent assassin. It doesn’t shout. It doesn’t scream. It just… stops your liver from working.
And yet - we treat it like a handshake. A nod. A ‘sure, why not.’
What if your car had a button that said ‘press for engine failure’ and you pressed it every Tuesday because ‘it was just a little bit’?
That’s what we’re doing.
Wake up.
OMG I JUST REALIZED I’VE BEEN TAKING DAYQUIL AND TYLENOL TOGETHER FOR WEEKS 😭
my head hurts, my stomach’s weird, and now i’m paranoid. i’m going to the pharmacy tomorrow. no more guessing. no more ‘it’s just a little’. i’m done.
also - why is there no app that scans your whole cabinet and says ‘YOU’RE ABOUT TO DIE’? we need this.
ps: i’m telling my mom. she’s got 12 bottles on her counter. she thinks she’s healthy. she’s not.
NSAID-induced renal hypoperfusion in polypharmacy patients is a well-documented phenomenon. The COX-2 inhibition reduces glomerular filtration rate, especially when combined with RAS inhibitors or diuretics. Risk stratification is critical in elderly populations with comorbidities.
Bottom line: don’t take ibuprofen if you’re on lisinopril. Period.
So let me get this straight - the same company that sells me Advil also sells me NyQuil… and both have acetaminophen? And I’m supposed to read the tiny print on the back of the box while I’m half-asleep and in pain?
That’s not a warning. That’s a trap.
Someone’s making bank off this. And we’re the dumbasses buying it.
I’m a nurse. I’ve seen people come in with liver failure because they took ‘just one’ extra Tylenol for a cold. They didn’t know their cold medicine had it. They didn’t know their doctor didn’t ask.
Please, if you’re reading this - write down your meds. Even the vitamins. Even the ‘herbal’ stuff. Take it to your pharmacist. They’re not trying to sell you anything. They’re trying to keep you alive.
And if you’re a doctor - ask. Just ask. Don’t assume they’re telling you everything.
Why is this even a thing? If you can’t read a label, don’t take the pill. Simple. Stop blaming Big Pharma. Stop pretending you’re too busy. Your life isn’t that hard. If you can scroll TikTok for an hour, you can read 10 words on a bottle.
Also - ‘natural’ supplements? Most are garbage. St. John’s Wort? It’s not a tea. It’s a drug. And it’s illegal to mix with SSRIs in some countries. But here? We just shrug and take it with Lexapro. Classic.
I’m 68 and I’ve been on blood pressure meds for 15 years. I never thought about OTC meds interacting - until my pharmacist sat me down last month and said, ‘You’re taking ibuprofen three times a week for your knees. That’s not okay.’
I cried. Not because I was scared - but because no one had ever taken the time to explain it to me like a human.
Thank you for this. I’m going to make a chart. I’m going to stick it on my fridge. And I’m going to tell my friends.
Knowledge isn’t power. It’s survival.
Wait - so the whole ‘OTC is safe’ thing is a lie? Like… the entire marketing campaign? The ads? The shelves next to candy? The ‘ask your pharmacist’ stickers?
So what’s next? Are we gonna find out that ‘sugar-free’ soda is secretly poisoning us too?
Maybe the real danger isn’t the pills - it’s the fact that we’ve been conditioned to trust everything that looks like medicine.
Who designed this system? And why?
…I think I need to go live in a cabin now.