 28
Dec,2025
28
Dec,2025
When you think of a generic drug, you picture a small pill-cheap, simple, and identical to the brand-name version. But biosimilars? They’re not that simple. These aren’t chemical copies like traditional generics. They’re complex, living molecules made inside living cells. And getting them right? That’s where things get incredibly hard.
The Core Problem: You Can’t Just Copy a Recipe
Generics are made by mixing chemicals in a lab. If you know the formula, you can make the exact same molecule every time. Biosimilars? They’re proteins-sometimes bigger than a virus-grown inside cells like Chinese hamster ovary (CHO) cells. The cell doesn’t follow a recipe. It responds to its environment: temperature, nutrients, oxygen, pH, even how hard you stir the tank. Change one thing, and the protein changes. That’s why experts say: the process defines the product.You’re not copying a drug. You’re reverse-engineering a living system you can’t see. Imagine trying to recreate a gourmet dish without knowing the ingredients, the chef’s technique, or even what stove they used. That’s what biosimilar manufacturers face.
Glycosylation: The Silent Killer of Consistency
One of the biggest headaches? Glycosylation. That’s when sugar molecules attach to the protein backbone. Sounds small? It’s not. These sugars control how long the drug stays in your body, how well it binds to targets, and whether your immune system reacts to it.Even tiny differences in glycosylation can turn a safe drug into a risky one. A biosimilar might have 99% the same structure-but if 1% of its sugar chains are off, it could clear from your blood faster, or trigger an immune response. The originator company spent years optimizing this. The biosimilar maker has to guess how.
That means testing hundreds of samples, using advanced tools like mass spectrometry and HPLC, to map out the exact sugar pattern of the reference drug. Then, they have to tweak their cell culture conditions-media, feeding schedules, oxygen levels-until the sugars match. And they have to do it every single batch. No room for error.
Scale-Up: Bigger Tanks Don’t Mean Better Results
Getting a biosimilar to work in a 5-liter lab bioreactor is one thing. Getting it to work in a 20,000-liter commercial tank? That’s a whole new problem.In small tanks, everything mixes evenly. In big ones, you get dead zones. Oxygen doesn’t reach all the cells. Temperature varies by degrees. Stirring speed that worked in the lab might shear the protein in production. The cells feel different. They behave differently. The protein changes.
Manufacturers have to rebuild the entire process from scratch at each scale. It’s not just buying a bigger machine. It’s re-engineering the whole environment so the cells think they’re still in the small tank. Many companies fail here. They get a perfect product at lab scale-then lose it when scaling up. That’s why some biosimilars never make it to market.

Supply Chain and Cold Chain: One Mistake, Millions Lost
Biosimilars don’t just need careful production. They need careful handling.These proteins are fragile. If a storage bag leaks during transport, or a freezer fails for two hours, the whole batch can be ruined. That’s not a minor loss. A single 10,000-liter batch can cost over $10 million to produce. One broken pump, one mislabeled container, and it’s all gone.
And it’s not just temperature. Time matters too. From harvest to final filling, the clock is ticking. The longer the protein sits, the more it degrades. That’s why manufacturers are moving toward closed, automated systems-fewer hands, fewer chances for error. Single-use bags and tubing are now standard. No cleaning. No cross-contamination. Less risk.
Regulatory Hurdles: Proving You’re Similar, Not Identical
The FDA and EMA don’t just want you to say, “It’s similar.” They want proof. And not just one proof. They want dozens.You need analytical data showing structural similarity down to the amino acid level. Functional data proving it binds the same way. Preclinical data showing it works the same in animals. And often, clinical trials to confirm safety and efficacy in humans. All of this costs hundreds of millions and takes 7-10 years.
And it’s not the same everywhere. The EU has stricter requirements than some other regions. The FDA updated its guidance in 2023 to demand more detailed analytical comparisons. Companies without state-of-the-art labs-think advanced chromatography, NMR, cryo-EM-simply can’t compete.
Complex Biosimilars Are Getting Even Harder
The easiest biosimilars to copy are monoclonal antibodies-like those for rheumatoid arthritis. But the next wave? Bispecific antibodies, antibody-drug conjugates, fusion proteins. These are engineered to do multiple things at once. More parts. More steps. More places to fail.Take an antibody-drug conjugate: you’re attaching a toxic drug to an antibody. But the drug must attach at exactly the right spot, in exactly the right number. Too few? The drug doesn’t work. Too many? It becomes toxic. The process requires extra purification, refolding, and testing. Each step adds cost and risk.
These aren’t just harder to make. They’re harder to test. The tools to analyze them are still evolving. That’s why only a handful of companies have successfully brought them to market.

How the Industry Is Fighting Back
Manufacturers aren’t sitting still. They’re using new tools to fight complexity.- Single-use systems cut contamination risk and speed up changeovers. The market for these is expected to hit $29.5 billion by 2029.
- Process analytical technology (PAT) lets them monitor quality in real time-measuring pH, sugar levels, protein shape as the batch runs. If something drifts, they fix it before it’s too late.
- Automation reduces human error. Robots handle filling, labeling, and testing. Fewer mistakes. Fewer recalls.
- AI and machine learning are being used to predict how changes in temperature or nutrient mix will affect the final product. Instead of trial and error, they run virtual simulations.
These aren’t luxuries anymore. They’re survival tools.
The Market Is Growing-But Only for the Strong
The global biosimilars market was worth $7.9 billion in 2022. By 2030, it’s expected to hit $58.1 billion. That’s huge. But only a few companies will win.Why? Because the cost to enter is astronomical. You need:
- Millions in R&D
- Advanced labs with $10M+ equipment
- Experience with biologics
- Regulatory expertise
- Supply chain control
Smaller players are getting squeezed out. We’re already seeing consolidation. Big pharma is buying up biosimilar startups. If you don’t have the infrastructure, you don’t have a shot.
And even if you make it to market, you’re not done. You have to prove consistency every single batch. Every year. Every change. The bar doesn’t lower after approval-it stays high forever.
Why This Matters to Patients
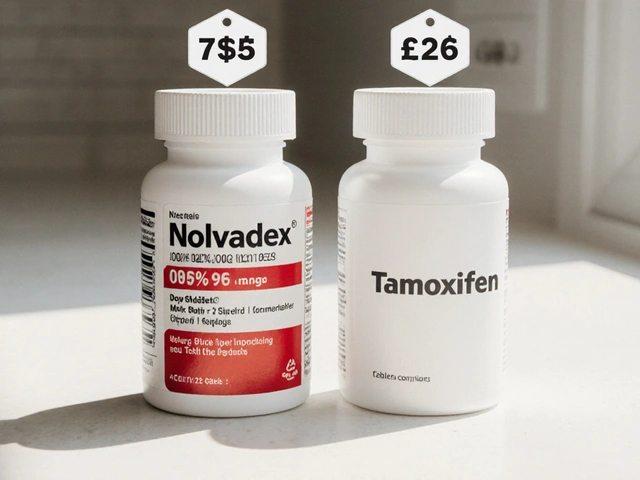
Biosimilars are meant to lower costs. A good biosimilar can cut the price of a biologic by 30-50%. That means more patients can afford life-saving drugs for cancer, autoimmune diseases, and rare conditions.But if the manufacturing is flawed? That’s not savings. That’s risk. A poorly made biosimilar could be less effective-or worse, trigger serious side effects.
That’s why regulators demand so much proof. It’s not bureaucracy. It’s safety.
The truth? Biosimilars are the most complex generics ever made. They’re not just copies. They’re miracles of engineering. And the people making them are solving problems no one else can.
Are biosimilars the same as generics?
No. Generics are small-molecule drugs made from chemicals, and they’re chemically identical to the brand-name version. Biosimilars are large, complex proteins made in living cells. They’re highly similar to the original biologic, but not identical due to natural biological variability. You can’t make a biosimilar by following a chemical formula-you have to recreate a living process.
Why is glycosylation such a big deal in biosimilars?
Glycosylation-sugar chains attached to proteins-affects how the drug behaves in the body. It changes how long it lasts, how well it binds to targets, and whether the immune system reacts. Even small differences can reduce effectiveness or cause side effects. Matching the reference product’s glycosylation pattern is one of the hardest parts of biosimilar development.
Can biosimilars be made cheaper than the original biologics?
Yes, but not easily. While biosimilars cost less to produce than the original biologic, the upfront investment is enormous-often over $100 million. The savings come from avoiding early R&D costs, but manufacturing complexity, regulatory testing, and quality control keep prices higher than traditional generics. Still, they typically cost 30-50% less than the originator drug.
What’s the biggest barrier to entering the biosimilars market?
The biggest barrier is the combination of technical complexity and regulatory burden. You need advanced analytical tools, deep expertise in biologics, massive capital for facilities, and years of experience. Most small companies can’t afford it. That’s why only a few large biopharma firms dominate the market.
Are biosimilars safe?
Yes, when properly developed and manufactured. Biosimilars approved by the FDA, EMA, and other major agencies have undergone rigorous testing and are used safely by millions of patients worldwide. The key is consistent quality control-every batch must match the reference product. That’s why ongoing monitoring and strict manufacturing standards are non-negotiable.





Man, I never realized how wild biosimilars are compared to regular generics. I thought it was just about copying a pill, but this is like trying to clone a chef’s secret recipe while blindfolded. Crazy stuff.
And glycosylation? Never heard of it before, but now I get why it’s such a nightmare. One sugar chain off and boom - your drug’s useless or dangerous. Wild.
This is why big pharma owns everything 😭💸
Small companies don’t stand a chance. They spend $100M and still get rejected because some sugar molecule was 0.3% off. Absolute joke. 🤡
Oh wow, so we’re paying $10,000 for a drug because some hamster cells had a bad day? 🤦♂️
Let me get this straight - you can’t just make the same protein because the cell ‘feels’ different? That’s not science, that’s witchcraft with a bioreactor.
And now we’re supposed to trust these things? I’d rather just keep paying for the original and save myself the existential dread.
Really appreciate this breakdown - especially the PAT and AI angle. Real-time process analytics is a game-changer. You’re not just QA’ing the end product anymore, you’re controlling the entire bioprocess dynamically.
Single-use systems + closed-loop automation + ML-driven optimization? That’s the future. The companies that invest in these now will dominate the next decade. It’s not about being cheap - it’s about being precise.
Also, cryo-EM for glycosylation mapping? That’s next-level. We’re talking atomic-resolution imaging of protein glycan structures. Mind blown.
This is why we need to stop letting corporations play god with medicine. If it’s this hard to make, why are we even trying? Just make the original cheaper. People are dying because of profit motives, not science.
Honestly? This is one of the coolest things in modern medicine. Think about it - we’re reverse-engineering biology at a molecular level using tools that didn’t exist 15 years ago.
It’s like trying to rebuild a living, breathing organism from scratch using only its shadow. And somehow, people are doing it.
Shoutout to the lab techs working 18-hour shifts with HPLC machines, just to match a sugar chain. We don’t hear enough about them.
It’s funny how we call these ‘biosimilars’ like they’re just copies. But if you think about it, every human is a biosimilar of their parents - genetically similar, but never identical. Maybe we’re just learning to make biosimilars of molecules, and that’s actually pretty human.
There’s beauty in imperfection. The fact that we can get 99% right, and still save lives? That’s not failure. That’s evolution.
Y’all are underestimating how much hope this brings. I’ve seen patients who couldn’t afford Humira - now they’re getting off steroids, going back to work, playing with their kids. That’s what this is about.
Yes, it’s complex. Yes, it’s expensive. But if we keep pushing, we’ll make it accessible. I’ve seen it happen. Don’t give up on the science - it’s saving lives.
Let’s be real - if you’re not using NMR, cryo-EM, and high-res mass spec, you’re not even in the game. Most ‘biosimilars’ on the market are just ‘biosimilar-ish’ - barely regulated, barely tested. Regulatory agencies are asleep at the wheel.
And don’t get me started on the FDA’s ‘similar enough’ loophole. This isn’t science - it’s corporate compromise dressed up as progress.
I work in a clinic and we’ve had patients switch to biosimilars - and honestly? No one noticed a difference. One lady with RA said she felt better because she wasn’t stressed about the price anymore.
It’s not magic, but it’s working. The science might be insane, but the outcome? Simple. More people get help. That’s what matters.
Biggest takeaway? The real heroes aren’t the CEOs or the regulators - they’re the process engineers in clean rooms, tweaking pH by 0.02 units at 3 a.m. so a batch doesn’t fail.
This isn’t just manufacturing. It’s art. And it’s happening in silence. We should celebrate them more.